Volume 19, Issue 2 (9-2022)
J Res Dev Nurs Midw 2022, 19(2): 14-17 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Bhattacharya S, Dutta B, Chandra Mondal S. Knowledge and Practice About Birth Preparedness and Complication Readiness (BPACR) Among Primigravida Women: A Cross-Sectional Study. J Res Dev Nurs Midw 2022; 19 (2) :14-17
URL: http://nmj.goums.ac.ir/article-1-1338-en.html
URL: http://nmj.goums.ac.ir/article-1-1338-en.html
1- Department of Health and Family Welfare, Balurghat Nursing Training School, India
2- Department of Medical and Surgical Nursing, B.M. Birla College of Nursing, India
3- Department of Obstetrics and gynaecology, Malda Medical College and Hospital, India ,sureshmondal77@gmail.com
2- Department of Medical and Surgical Nursing, B.M. Birla College of Nursing, India
3- Department of Obstetrics and gynaecology, Malda Medical College and Hospital, India ,
Full-Text [PDF 693 kb]
(2070 Downloads)
| Abstract (HTML) (3486 Views)
Full-Text: (571 Views)
Introduction
Maternal mortality has become an unavoidable nightmare for developing nations for a decade and continues to be a significant public health issue. Literature states that about 66% of the maternal deaths worldwide happens in South Asia (1). In low and lower-middle-income countries, 94% of all maternal deaths globally are reported (2). According to the national Sample Registration System (SRS) 2016-18, India’s Maternal Mortality Ratio (MMR) is 113 per 100,000 live births, showing a decline of 17 points, from 130 per 100,000 live births in 2014-16 (3). In West Bengal, MMR is 98 per 100,000 live births as per data given by SRS for the time duration of 2016-18 (4).
A World Health Organization (WHO) report states that nearly 830 women die during pregnancy and childbirth from avoidable causes; also, in developing countries, about 300 million females suffer from short-term or long-term morbidities because of childbirth and pregnancy (5,6). Maternal deaths occur when there is rise in blood pressure throughout pregnancy (pre-eclampsia and eclampsia), the occurrence of infections (mainly after childbirth), when unsafe abortions are performed, complications due to delivery, and severe bleeding (usually bleeding after childbirth). These are some major complications that cause about 75% of maternal deaths (7). Hypertensive disorders, including gestational hypertension, pre-eclampsia superimposed on chronic hypertension, and pre-eclampsia, affect 10% of pregnancies globally (8). Literature shows that the incidence of post-partum infection is approximately 10–20% after cesarean section and1–4% after vaginal delivery (9, 10). Post-partum hemorrhage, a condition where there is loss of more than 500 mL of blood after delivery, has become the primary cause of maternal mortality universally (10–12). Results of a scoping review put a glance at social determinants influencing maternal health in India, which are education, gender (in terms of autonomy and decision making of women in the household), economic status, religion, culture, and caste/ethnicity (13).
Maternal mortalities can be reduced with help of healthcare facilities and infrastructure if availed at right time. There are three significant delays documented by Thaddeus and Maine which contribute to overall maternal mortality. These are the delay of decision making to take medical help when complications arise, delay in reaching healthcare facilities and delay in availing healthcare services that help in reducing maternal mortality (7,14). To tackle these three delays Program of Johns Hopkins Program for International Education in Gynaecology and Obstetrics (JHPIEGO) under the program of the Maternal and Neonatal Health (MNH) established the birth preparedness and complication readiness (BPACR) matrix at the various levels. Firstly, the pregnant woman, next is her family, after family comes to her community, health providers near her, health facilities available in her locality, and policymakers during pregnancy, childbirth, and the postpartum period (15, 16). Few important elements of BPACR are pregnancy registration of the mother, awareness of danger signs during pregnancy, planning for the place of delivery, planning of skilled birth attendant, transportation facilities availability, a companion at the time of birth, and spotting of blood group donors of compatible blood groups if needed in emergency cases (17).
There exists sufficient evidence in the literature showing the benefits and positive effects of the BPACR strategy in safe pregnancy and motherhood (15, 16, 18, 19). This study was conducted with objectives to assess knowledge and practice about BPACR to assess the knowledge and practices of BPACR among third-trimester women attending Antenatal clinics.
Methods
The present study was a descriptive cross-sectional study conducted in the antenatal clinic of Howrah District Hospital West Bengal. The study population was 200 Primigravida mothers who were in the third trimester of pregnancy, before the onset of labor, and who were attending the antenatal clinic during the study period. Non- probability convenience sampling technique was followed to recruit the participants during their antenatal visits.
The required sample size was 200 (prevalence=41% as per Anita Shankar Acharya et al (20) study)
The sample size was derived from the following formula:
Sample size (n) = (Z^2 (P*Q))/d^2 where;
Z=Confidence Interval, D=absolute precision=0.07, P=expected proportion= 41% and q=1-p
The sample size was calculated using the above formula by Daniel WW et al (21).
Primigravida mothers attending the antenatal clinic for the first time and Primigravida mothers with high-risk pregnancies (such as elderly primi, short stature etc) were excluded from the study. The data collection of the study was done from 15th December 2020 to 20th January 2021. Ethical approval was obtained from the Institutional Ethics Committee of BM Birla Heart Research Center (Ref: ECR/55/Inst/WB/2013/RR-19) and Written informed consent was obtained from the individual subject before including in the study.
To conduct the study, we developed three pre-designed and pre-tested tools which were - Structured interview schedule to collect demographic data, a structured knowledge questionnaire regarding BPACR, Checklist to assess practice about BPACR based on previous studies. These three tools were translated from English to (regional) Bengali language by an expert in Bengali language and retranslated from Bengali to English by an expert in the English language to determine linguistic equivalency. The content validity was assessed by three independent subject experts. The principal investigator collected the responses of the mothers during their antenatal visits. In this study knowledge refers to the correct response of the antenatal primigravida mothers in the third trimester of pregnancy about BPACR which would be assessed by a structured knowledge questionnaire. Adequate knowledge was considered when women have given correct answers more than equal to 10 questions and inadequate knowledge when answered less than 10 questions correctly. In this present studyrefers to the stated practice of antenatal mothers in the third trimester of pregnancy which would be assessed by a checklist. The adequate practice was considered when women has answered more than or equal to 10 questions correctly and inadequate practice was considered when less than 10 questions were answered correctly. In this study, BPACR were considered primigravida mothers could prepare all component of BPACR like skilled birth providers, save money, identify place of delivery, identified the mode of transport, identify the escort persons, identify decision-makers, arranged of blood donor and spontaneously responded the key danger sign of all periods antenatal, intra-natal, and postnatal period (16). In this study, a primigravida mother refers to mothers who were pregnant for the first time and existed in the third trimester in pregnancy till before the onset of labor.
Statistical Methods
Knowledge Items and Practice were considered as primary outcome variables. Demographic parameter and maternal outcome and related parameter were considered as Primary explanatory variables. Descriptive analysis was carried out by frequency and proportion for categorical variables. The Chi-square test or Fischer’s exact test was used as a test of significance for qualitative data. Correlations were performed with the Pearson Correlation coefficient. Data was analyzed by using coGuide software, V.1.03 (21).
Results
A total of 200 primigravida mothers were included in the final analysis
In the primigravida mothers in third trimester of pregnancy, 151(75.5 %) belonged to the age group of 20-30 years. The proportion of Hindu and Muslim was 146(73%) and 54(27%). Out of 200 mothers, 169(84.5%) had higher secondary level of education and 31(15.5%) were graduate and above, 7(3.5%) women were in service, 17(8.5%) women were self-employed and 176(88%) women were home maker. Majority of the mothers were from Nuclear family 146(73%) and 161(80.5%) had income between Rs.5001/- to Rs.10, 000/- and 39(19.5%) had between Rs. 10001/- to Rs. 15,000/ as family income. Among mothers, 125(62.5%) ailed from urban areas and 75(37.5%) lived in rural area. (Table 1)
Among the primigravida mother’s, 52.5% were more than 34 weeks of gestational age, 48% had three antenatal visits, 65.5% pregnant women had taken Iron, Folic acid and Calcium supplementation up to three months. Out of 200 pregnant women, 97% primigravida mothers received information about BPACR, 77.32% received information from health care provider, followed by 20(10.31%) from electronic media. (Table 2)
Out of 200 mothers, 62 (31%) primigravida mothers had adequate levels of knowledge about birth BPACR whereas 138 (69%) primigravida mothers had inadequate levels of knowledge about BPACR. Individual knowledge parameters responses were recorded in (Table 3).
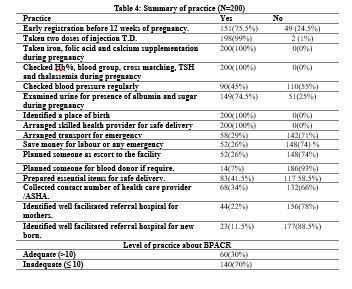
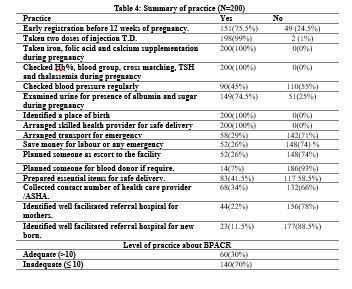
Out of 200 mothers, 60 (30%) had adequate levels of practice whereas 140 (70%) had inadequate level of practice. (Table 4).
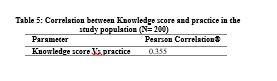
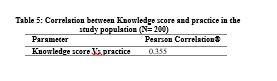
There is no significant relationship between knowledge and practice about BPACR at 0.05 level of significance with week positive correlation (r value=0.355). (Table 5)
.JPG)

Discussion
Based on the findings of this cross-sectional study, 69% of the participants had inadequate knowledge about BPACR, and 70% of the participants followed inadequate practices regarding BPACR. Studies conducted in other parts of India reported similar findings (22, 23). A study by Agarwal et al. among slum dwellers in Indore city reported an overall BPACR score of 47.8% (19). Acharya et al. reported overall BPACR score of 41% among 417 women seeking antenatal care in Delhi, India (15). Interestingly, two different studies conducted in the West Bengal revealed BPACR scores of 34.5% and 49.4% (23, 24). Wide range of studies have reported BPACR level globally. Various studies have reported an Overall BPACR values as Ethiopia (16.5±29.9%) (25–28), Uganda (35%) (29), Tanzania (58.2%) (29), Nepal (32±65%) (30, 31). It has been shown that women empowerment, literacy level, health-seeking behavior, education level of husbands, and major occupations may influence the knowledge of BPACR. Moreover, the method of assessing BPACR status can be considered as another attributing factor.
Previous national and international studies have documented the significant impact of women’s literacy on BPACR (19, 32–34). The low level of BPACR in the present study might be related to the limited access to healthcare providers during early pregnancy. Other studies have also attributed unsatisfactory BPACR practices to poor knowledge of the key danger signs (15, 26). Adequate knowledge of danger signs aids in early recognition of potentially life-threatening complications, which may avert the unnecessary delay in seeking healthcare (17). Healthcare workers should educate pregnant women and their families regarding the danger signs during pregnancy.
The most common causes of maternal mortality in India are maternal anemia and post-partum hemorrhage (4). This indicates the importance of identifying a compatible blood donor and the availability of blood in case of emergencies. With the current lack of resources in India complications among antenatal women have to be anticipated early so as to manage on time by providing adequate referral services. Given the poor knowledge an practices of BPACR among our subjects, it is recommended to provide appropriate health education and awareness programs to the subjects in order to reduce the risk of maternal mortality.
The cross-sectional nature of the methodology was a limitation of this study. Moreover, follow-up and outcomes of pregnancy were not assessed in the present study. The questionnaires used in the study were self-reported; hence, there was a chance of subjective assessment bias.
Conclusion
In this study, the knowledge and practices of BPACR were low among primigravida women. Ideal BPACR knowledge can be achieved by increasing the number of healthcare provider visits. Healthcare workers should explain BPACR to pregnant women as well as their family members. Adolescent girls and newly married couples should be targeted for BPACR advice.
Acknowledgements
The authors acknowledge the technical support in data entry, analysis, and manuscript editing by “Evidencian Research Associates.
Funding source
The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical statement
Ethics approval was obtained from the Institutional Ethics Committee of BM Birla Heart Research Center (Reference number: ECR/55/Inst/WB/2013/RR-19). Participation in the study was voluntary, and consent was obtained from the subjects after explaining the objectives ensuring about confidentiality of personal information.
Conflict of interest
The authors declare that there is no conflict of interest regarding publication of this article.
Author contributions
Suresh Chandra Mondal conducted study design. Data were collected by Suparna Bhattacharya and Bhanumati Dutta. Suparna Bhattacharya, Bhanumati Dutta, and Suresh Chandra Mondal analysed the data. All authors contributed equally to manuscript preparation.
Maternal mortality has become an unavoidable nightmare for developing nations for a decade and continues to be a significant public health issue. Literature states that about 66% of the maternal deaths worldwide happens in South Asia (1). In low and lower-middle-income countries, 94% of all maternal deaths globally are reported (2). According to the national Sample Registration System (SRS) 2016-18, India’s Maternal Mortality Ratio (MMR) is 113 per 100,000 live births, showing a decline of 17 points, from 130 per 100,000 live births in 2014-16 (3). In West Bengal, MMR is 98 per 100,000 live births as per data given by SRS for the time duration of 2016-18 (4).
A World Health Organization (WHO) report states that nearly 830 women die during pregnancy and childbirth from avoidable causes; also, in developing countries, about 300 million females suffer from short-term or long-term morbidities because of childbirth and pregnancy (5,6). Maternal deaths occur when there is rise in blood pressure throughout pregnancy (pre-eclampsia and eclampsia), the occurrence of infections (mainly after childbirth), when unsafe abortions are performed, complications due to delivery, and severe bleeding (usually bleeding after childbirth). These are some major complications that cause about 75% of maternal deaths (7). Hypertensive disorders, including gestational hypertension, pre-eclampsia superimposed on chronic hypertension, and pre-eclampsia, affect 10% of pregnancies globally (8). Literature shows that the incidence of post-partum infection is approximately 10–20% after cesarean section and1–4% after vaginal delivery (9, 10). Post-partum hemorrhage, a condition where there is loss of more than 500 mL of blood after delivery, has become the primary cause of maternal mortality universally (10–12). Results of a scoping review put a glance at social determinants influencing maternal health in India, which are education, gender (in terms of autonomy and decision making of women in the household), economic status, religion, culture, and caste/ethnicity (13).
Maternal mortalities can be reduced with help of healthcare facilities and infrastructure if availed at right time. There are three significant delays documented by Thaddeus and Maine which contribute to overall maternal mortality. These are the delay of decision making to take medical help when complications arise, delay in reaching healthcare facilities and delay in availing healthcare services that help in reducing maternal mortality (7,14). To tackle these three delays Program of Johns Hopkins Program for International Education in Gynaecology and Obstetrics (JHPIEGO) under the program of the Maternal and Neonatal Health (MNH) established the birth preparedness and complication readiness (BPACR) matrix at the various levels. Firstly, the pregnant woman, next is her family, after family comes to her community, health providers near her, health facilities available in her locality, and policymakers during pregnancy, childbirth, and the postpartum period (15, 16). Few important elements of BPACR are pregnancy registration of the mother, awareness of danger signs during pregnancy, planning for the place of delivery, planning of skilled birth attendant, transportation facilities availability, a companion at the time of birth, and spotting of blood group donors of compatible blood groups if needed in emergency cases (17).
There exists sufficient evidence in the literature showing the benefits and positive effects of the BPACR strategy in safe pregnancy and motherhood (15, 16, 18, 19). This study was conducted with objectives to assess knowledge and practice about BPACR to assess the knowledge and practices of BPACR among third-trimester women attending Antenatal clinics.
Methods
The present study was a descriptive cross-sectional study conducted in the antenatal clinic of Howrah District Hospital West Bengal. The study population was 200 Primigravida mothers who were in the third trimester of pregnancy, before the onset of labor, and who were attending the antenatal clinic during the study period. Non- probability convenience sampling technique was followed to recruit the participants during their antenatal visits.
The required sample size was 200 (prevalence=41% as per Anita Shankar Acharya et al (20) study)
The sample size was derived from the following formula:
Sample size (n) = (Z^2 (P*Q))/d^2 where;
Z=Confidence Interval, D=absolute precision=0.07, P=expected proportion= 41% and q=1-p
The sample size was calculated using the above formula by Daniel WW et al (21).
Primigravida mothers attending the antenatal clinic for the first time and Primigravida mothers with high-risk pregnancies (such as elderly primi, short stature etc) were excluded from the study. The data collection of the study was done from 15th December 2020 to 20th January 2021. Ethical approval was obtained from the Institutional Ethics Committee of BM Birla Heart Research Center (Ref: ECR/55/Inst/WB/2013/RR-19) and Written informed consent was obtained from the individual subject before including in the study.
To conduct the study, we developed three pre-designed and pre-tested tools which were - Structured interview schedule to collect demographic data, a structured knowledge questionnaire regarding BPACR, Checklist to assess practice about BPACR based on previous studies. These three tools were translated from English to (regional) Bengali language by an expert in Bengali language and retranslated from Bengali to English by an expert in the English language to determine linguistic equivalency. The content validity was assessed by three independent subject experts. The principal investigator collected the responses of the mothers during their antenatal visits. In this study knowledge refers to the correct response of the antenatal primigravida mothers in the third trimester of pregnancy about BPACR which would be assessed by a structured knowledge questionnaire. Adequate knowledge was considered when women have given correct answers more than equal to 10 questions and inadequate knowledge when answered less than 10 questions correctly. In this present studyrefers to the stated practice of antenatal mothers in the third trimester of pregnancy which would be assessed by a checklist. The adequate practice was considered when women has answered more than or equal to 10 questions correctly and inadequate practice was considered when less than 10 questions were answered correctly. In this study, BPACR were considered primigravida mothers could prepare all component of BPACR like skilled birth providers, save money, identify place of delivery, identified the mode of transport, identify the escort persons, identify decision-makers, arranged of blood donor and spontaneously responded the key danger sign of all periods antenatal, intra-natal, and postnatal period (16). In this study, a primigravida mother refers to mothers who were pregnant for the first time and existed in the third trimester in pregnancy till before the onset of labor.
Statistical Methods
Knowledge Items and Practice were considered as primary outcome variables. Demographic parameter and maternal outcome and related parameter were considered as Primary explanatory variables. Descriptive analysis was carried out by frequency and proportion for categorical variables. The Chi-square test or Fischer’s exact test was used as a test of significance for qualitative data. Correlations were performed with the Pearson Correlation coefficient. Data was analyzed by using coGuide software, V.1.03 (21).
Results
A total of 200 primigravida mothers were included in the final analysis
In the primigravida mothers in third trimester of pregnancy, 151(75.5 %) belonged to the age group of 20-30 years. The proportion of Hindu and Muslim was 146(73%) and 54(27%). Out of 200 mothers, 169(84.5%) had higher secondary level of education and 31(15.5%) were graduate and above, 7(3.5%) women were in service, 17(8.5%) women were self-employed and 176(88%) women were home maker. Majority of the mothers were from Nuclear family 146(73%) and 161(80.5%) had income between Rs.5001/- to Rs.10, 000/- and 39(19.5%) had between Rs. 10001/- to Rs. 15,000/ as family income. Among mothers, 125(62.5%) ailed from urban areas and 75(37.5%) lived in rural area. (Table 1)
Among the primigravida mother’s, 52.5% were more than 34 weeks of gestational age, 48% had three antenatal visits, 65.5% pregnant women had taken Iron, Folic acid and Calcium supplementation up to three months. Out of 200 pregnant women, 97% primigravida mothers received information about BPACR, 77.32% received information from health care provider, followed by 20(10.31%) from electronic media. (Table 2)
Out of 200 mothers, 62 (31%) primigravida mothers had adequate levels of knowledge about birth BPACR whereas 138 (69%) primigravida mothers had inadequate levels of knowledge about BPACR. Individual knowledge parameters responses were recorded in (Table 3).
Out of 200 mothers, 60 (30%) had adequate levels of practice whereas 140 (70%) had inadequate level of practice. (Table 4).
There is no significant relationship between knowledge and practice about BPACR at 0.05 level of significance with week positive correlation (r value=0.355). (Table 5)
.JPG)

Discussion
Based on the findings of this cross-sectional study, 69% of the participants had inadequate knowledge about BPACR, and 70% of the participants followed inadequate practices regarding BPACR. Studies conducted in other parts of India reported similar findings (22, 23). A study by Agarwal et al. among slum dwellers in Indore city reported an overall BPACR score of 47.8% (19). Acharya et al. reported overall BPACR score of 41% among 417 women seeking antenatal care in Delhi, India (15). Interestingly, two different studies conducted in the West Bengal revealed BPACR scores of 34.5% and 49.4% (23, 24). Wide range of studies have reported BPACR level globally. Various studies have reported an Overall BPACR values as Ethiopia (16.5±29.9%) (25–28), Uganda (35%) (29), Tanzania (58.2%) (29), Nepal (32±65%) (30, 31). It has been shown that women empowerment, literacy level, health-seeking behavior, education level of husbands, and major occupations may influence the knowledge of BPACR. Moreover, the method of assessing BPACR status can be considered as another attributing factor.
Previous national and international studies have documented the significant impact of women’s literacy on BPACR (19, 32–34). The low level of BPACR in the present study might be related to the limited access to healthcare providers during early pregnancy. Other studies have also attributed unsatisfactory BPACR practices to poor knowledge of the key danger signs (15, 26). Adequate knowledge of danger signs aids in early recognition of potentially life-threatening complications, which may avert the unnecessary delay in seeking healthcare (17). Healthcare workers should educate pregnant women and their families regarding the danger signs during pregnancy.
The most common causes of maternal mortality in India are maternal anemia and post-partum hemorrhage (4). This indicates the importance of identifying a compatible blood donor and the availability of blood in case of emergencies. With the current lack of resources in India complications among antenatal women have to be anticipated early so as to manage on time by providing adequate referral services. Given the poor knowledge an practices of BPACR among our subjects, it is recommended to provide appropriate health education and awareness programs to the subjects in order to reduce the risk of maternal mortality.
The cross-sectional nature of the methodology was a limitation of this study. Moreover, follow-up and outcomes of pregnancy were not assessed in the present study. The questionnaires used in the study were self-reported; hence, there was a chance of subjective assessment bias.
Conclusion
In this study, the knowledge and practices of BPACR were low among primigravida women. Ideal BPACR knowledge can be achieved by increasing the number of healthcare provider visits. Healthcare workers should explain BPACR to pregnant women as well as their family members. Adolescent girls and newly married couples should be targeted for BPACR advice.
Acknowledgements
The authors acknowledge the technical support in data entry, analysis, and manuscript editing by “Evidencian Research Associates.
Funding source
The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical statement
Ethics approval was obtained from the Institutional Ethics Committee of BM Birla Heart Research Center (Reference number: ECR/55/Inst/WB/2013/RR-19). Participation in the study was voluntary, and consent was obtained from the subjects after explaining the objectives ensuring about confidentiality of personal information.
Conflict of interest
The authors declare that there is no conflict of interest regarding publication of this article.
Author contributions
Suresh Chandra Mondal conducted study design. Data were collected by Suparna Bhattacharya and Bhanumati Dutta. Suparna Bhattacharya, Bhanumati Dutta, and Suresh Chandra Mondal analysed the data. All authors contributed equally to manuscript preparation.
Type of study: Original Article |
Subject:
Nursing
References
1. Mondal D, Karmakar S, Banerjee A. Women's autonomy and utilization of maternal healthcare in India: Evidence from a recent national survey. PLoS One. 2020; 15(12):e0243553. [View at paplisher] [DOI] [PMID] [Google Scholar]
2. WHO. Maternal mortality: evidence brief [Internet]. World Health Organisation. 2019. [Cited 2022 Oct 02]. Available from: https://apps.who.int/iris/handle/10665/329886
3. Maternal health [Internet]. UNICEF. Published 2018. [Cited 2021 Aug.18]. Available from: https://www.unicef.org/india/what-we-do/maternal-health
4. India Registrar General Maternal mortality in India: 1997-2003 Trend, causes and risk factors [Internet]. IDEAS. Published 2003. [Cited 2021 Nov.10]. Availablefrom:https://www.pib.gov.in/PressReleasePage.aspx?PRID=1697441
5. Abrams J. Maternal mortality. N J Med. 1990;87(12):975-976.
6. Gupta S, Yadav R, Malhotra AK. Birth Preparedness and Complication Readiness Plans among Antenatal Attendees at Primary Health Centre of District Jhansi, U.P, India. Int J Integr Med Sci. 2016; 3(4):258-264. [View at paplisher] [DOI] [Google Scholar]
7. Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Heal. 2014; 2:e323-33. [View at paplisher] [DOI] [Google Scholar]
8. Sutton ALM, Harper LM, Tita ATN. Hypertensive Disorders in Pregnancy. Obstet Gynecol Clin North Am. 2018; 45(2):333-347. [View at paplisher] [DOI] [PMID] [Google Scholar]
9. Leth RA, Møller JK, Thomsen RW, Uldbjerg N, Nørgaard M. Risk of selected postpartum infections after cesarean section compared with vaginal birth: a five-year cohort study of 32,468 women. Acta obstetricia et gynecologica Scandinavica. 2009; 88(9):976-83. [View at paplisher] [DOI] [PMID] [Google Scholar]
10. French L. Prevention and treatment of postpartum endometritis. Curr Womens Health Rep. 2003;3(4):274-279. [View at paplisher] [Google Scholar]
11. Anderson JM, Etches D. Prevention and management of postpartum hemorrhage. Am Fam Physician. 2007;75(6):875-882. [View at paplisher] [Google Scholar]
12. Vogel JP, Oladapo OT, Dowswell T, Gülmezoglu AM. Updated WHO recommendation on intravenous tranexamic acid for the treatment of post-partum haemorrhage. Lancet Glob Heal. 2018; 6(1):e18-e19. [View at paplisher] [DOI] [Google Scholar]
13. Hamal M, Hamal M, Hamal M, Dieleman M, Dieleman M, De Brouwere V, et al. Social determinants of maternal health: A scoping review of factors influencing maternal mortality and maternal health service use in India. Public Health Rev. 2020; 41(1):13. [View at paplisher] [DOI] [PMID] [Google Scholar]
14. Thaddeus S, Maine D. Too far to walk: maternal mortality in context. Soc Sci Med. 1994;38(8):1091-1110. [View at paplisher] [DOI] [Google Scholar]
15. Acharya AS, Kaur R, Prasuna JG, Rasheed N. Making Pregnancy Safer - Birth Preparedness and Complication Readiness Study among Antenatal Women Attendees of A Primary Health Center, Delhi. Indian J Community Med. 2015;40(2):127-134. [View at paplisher] [DOI] [PMID] [Google Scholar]
16. Sharma N, Kumar N, Singh S, Malik JS, Jangra A. Status and determinants of birth preparedness and complication readiness in a rural block of Haryana. J Fam Med Prim care. 2019; 8(2):482-486. [View at paplisher] [DOI] [PMID] [Google Scholar]
17. Del B. monitoring birth preparedness and complication readiness tools and indicators for maternal and newborn health [Internet]. JHPIEGO. Published 2004.
18. Viswanathan VT, Patil SS, Joshi RN, Durgawale PM. Study to Assess Birth Preparedness and Complication Readiness to Promote Safe Motherhood among Women from a Rural Area of Western Maharashtra. Indian J community Med Off Publ Indian Assoc Prev Soc Med. 2020;45(4):511-515. [View at paplisher] [DOI] [PMID] [Google Scholar]
19. Agarwal S, Sethi V, Srivastava K, Jha PK, Baqui AH. Birth preparedness and complication readiness among slum women in Indore city, India. J Heal Popul Nutr. 2010;28(4):383-391. [View at paplisher] [DOI] [PMID] [Google Scholar]
20. Acharya AS, Kaur R, Prasuna JG, Rasheed N. Making Pregnancy Safer - Birth Preparedness and Complication Readiness Study among Antenatal Women Attendees of A Primary Health Center, Delhi. Indian J Community Med. 2015; 40(2):127-134. [View at paplisher] [DOI] [PMID] [Google Scholar]
21. BDSS Corp. Released 2020. coGuide Statistics software, Version 1.0, BDSS corp Bangalore, India. Available from: https://www.coguide.in. [Last accessed on 2022 Nov 01].
22. Sharma N, Kumar N, Singh S, Malik J, Jangra A. Status and determinants of birth preparedness and complication readiness in a rural block of Haryana. J Fam Med Prim Care. 2019;8(2):482. [View at paplisher] [DOI] [PMID] [Google Scholar]
23. Mukhopadhyay DK, Mukhopadhyay S, Bhattacharjee S, Nayak S, Biswas AK, Biswas AB. Status of birth preparedness and complication readiness in Uttar Dinajpur District, West Bengal. Indian J Public Health. 2013; 57(3):147-154. [View at paplisher] [DOI] [PMID] [Google Scholar]
24. Mazumdar R, Mukhopadhyay DK, Kole S, Mallik D. Status of birth preparedness and complication readiness in a rural community : a study from West Bengal , India. Al Ameen J Med Sci. 2014; 7(1):52-57. [View at paplisher] [DOI] [PMID] [Google Scholar]
25. Hailu M, Gebremariam A, Alemseged F, Deribe K. Birth preparedness and complication readiness among pregnant women in Southern Ethiopia. PLoS One. 2011; 6(6):e21432. [View at paplisher] [DOI] [PMID] [Google Scholar]
26. Kaso M, Addisse M. Birth preparedness and complication readiness in Robe Woreda, Arsi Zone, Oromia Region, Central Ethiopia: A cross-sectional study. Reprod Health. 2014; 11(1):55. [View at paplisher] [DOI] [PMID] [Google Scholar]
27. Debelew GT, Afework F, Yalew AW. Factors affecting birth preparedness and complication readiness in Jimma Zone, Southwest Ethiopia: A multilevel analysis. Pan Afr Med J. 2014;19:272. [View at paplisher] [DOI] [PMID] [Google Scholar]
28. Markos D, Bogale D. Birth preparedness and complication readiness among women of child bearing age group in Goba woreda, Oromia region, Ethiopia. BMC Pregnancy Childbirth. 2014;14(1):282. [View at paplisher] [DOI] [PMID] [Google Scholar]
29. Kabakyenga JK, Östergren PO, Turyakira E, Pettersson KO. Influence of birth preparedness, decision-making on location of birth and assistance by skilled birth attendants among women in south-western Uganda. PLoS One. 2012; 7(4):e35747. [View at paplisher] [DOI] [PMID] [Google Scholar]
30. Nawal D, Goli S. Birth Preparedness and Its Effect on Place of Delivery and Post-Natal Check-Ups in Nepal. PLoS One. 2013; 8(5):e60957. [View at paplisher] [DOI] [PMID] [Google Scholar]
31. Karkee R, Lee AH, Binns CW. Birth preparedness and skilled attendance at birth in Nepal: implications for achieving millennium development goal 5. Midwifery. 2013;29(10):1206-1210. [View at paplisher] [DOI] [PMID] [Google Scholar]
32. Ekabua JE, Ekabua KJ, Odusolu P, Agan TU, Iklaki CU, Etokidem AJ. Awareness of birth preparedness and complication readiness in southeastern Nigeria. ISRN Obstet Gynecol. 2011; 2011:560641. [View at paplisher] [DOI] [PMID] [Google Scholar]
33. Pembe AB, Urassa DP, Carlstedt A, Lindmark G, Nyström L, Darj E. Rural Tanzanian women's awareness of danger signs of obstetric complications. BMC Pregnancy Childbirth. 2009; 9:12. [View at paplisher] [DOI] [PMID] [Google Scholar]
34. Kabakyenga JK, Östergren PO, Turyakira E, Pettersson KO. Knowledge of obstetric danger signs and birth preparedness practices among women in rural Uganda. Reprod Health. 2011;8(1):33. [View at paplisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |