Volume 19, Issue 2 (9-2022)
J Res Dev Nurs Midw 2022, 19(2): 10-13 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Eslami A, Hanifi N, Namadian M. Assessment of the Relationship between Patient Safety Culture and the Second Victim Experience in Critical Care Unit and Emergency Department Nurses. J Res Dev Nurs Midw 2022; 19 (2) :10-13
URL: http://nmj.goums.ac.ir/article-1-1325-en.html
URL: http://nmj.goums.ac.ir/article-1-1325-en.html
1- Department of Emergency and Critical Care Nursing, Zanjan University of Medical Sciences Iran
2- Department of Emergency and Critical Care Nursing, Zanjan University of Medical Sciences Iran , nasrinhanifi@gmail.com
3- Social Determinants of Health Research Center, Zanjan University of Medical Sciences Iran
2- Department of Emergency and Critical Care Nursing, Zanjan University of Medical Sciences Iran , nasrinhanifi@gmail.com
3- Social Determinants of Health Research Center, Zanjan University of Medical Sciences Iran
Full-Text [PDF 741 kb]
(536 Downloads)
| Abstract (HTML) (1621 Views)
Full-Text: (104 Views)
Introduction
The safety of care is one of the most important parts of healthcare service quality that reduces negative consequences for patients (1). The safety culture aims to keep the patient safe from any damage during the care services (2). However, medical error is inevitable, even in the best patient safety cultures (3).
After an adverse event or outcome, the patient and his/her family members are considered the first victims, while the healthcare staff members are considered second victims (4). A health care provider involved in an unanticipated adverse patient event, medical error, and/or a patient-related injury is the second victim (5). The second victim may suffer from various symptoms and disorders following an adverse event (6). These symptoms include physiological disorders, sleeping disorders, job burnout, reduced job satisfaction and self-confidence, work-related stress, feeling guilty, angry, and embarrassed, and concern about punishment, dismissal, and judicial conflicts (7-14). Therefore, considering the significant effect of the second victim phenomenon on patients' safety and the physical and emotional health of healthcare personnel, supporting the second victim(s) is of utmost importance (12).
A positive patient safety culture provides an environment in which staff can easily discuss errors and achieve successful coping after an adverse event (15, 16). Promoting open discussions, support about events, and meaningful patient safety event feedback in the hospital environment could enhance the possibility of learning from mistakes and responding to errors in no punitive ways that may be beneficial for effectively coping with the second victim event (17, 18). Conversely, a patient safety culture that encourages blame, criticism, silence, or stigmatization of patient safety events can intensify the physical and psychological distress in the second victim (19-21).
Intensive care unit (ICU) and emergency department (ED) nurses are under heavy workloads and constantly deal with stressful situations. This could be frustrating and depressing for the nurses, which may ultimately increase the rate of errors (22). According to previous studies in Iran, the level of patient safety is unacceptable, and the support resources for the hospital staff are limited (20, 23, 24). Therefore, this study aimed to determine the relationship between patient safety culture and the second victim experience in ICU and ED nurses.
Methods
This cross-sectional study was conducted on ICU and ED nurses working in hospitals affiliated with the Zanjan University of Medical Sciences (Zanjan, Iran) from October to December 2019. After a pilot study on 30 nurses, the required sample size was determined as 31 using the following formula and considering 95% confidence interval and 10% dropout rate:

The subjects were enrolled via the convenience sampling method. Inclusion criteria were having at least 1 year of job experience, having a bachelor's or master's degree in nursing, and willingness to participate in the study. Nurses who did not complete questionnaires were excluded from the study.
Data were collected using a demographic information questionnaire (Sex, age, job experience, marital status, educational level, organizational position, Unit), the Persian version of the Hospital Survey on Patient Safety Culture (HSOPSC), and the Second Victim Experience and Support Tool (SVEST). The validity and reliability of the Persian version of the HOSPSCQ have been confirmed (25). In this study, the internal reliability of the tool was also confirmed by obtaining a Cronbach’s alpha of 0.83. The HOSPSCQ includes 42 items and 12 components: 1) the overall perception of patient safety, 2) organizational learning-continuous improvement, 3) supervisor/manager expectations and actions promoting patient safety, 4) teamwork within units of the organization, 5) non-punitive response to error, 6) staffing, 7) management support for patient safety, 8) teamwork across units, 9) hand-offs and transitions, 10) communication openness, 11) feedback and communication about errors, and 12) frequency of events reporting. Components 1 to 9 were scored using a 5-point Likert scale, ranging from strongly disagree (1 point) to strongly agree (5 points). Components 10 to 12 were scored from 1 (never) to 5 (always). Agree, strongly agree, sometimes, and always were considered positive responses, while disagree, strongly disagree, rarely, and never were considered negative responses. However, some items (17 items) were scored inversely. According to the questionnaire guide, the components with a minimum of 50% positive responses were considered acceptable, and those with less than 50% were considered as cases, which should be improved. In the present study, the content validity method was used to examine the validity. The reliability of the dimensions of this questionnaire was 79% to 83%.
The SVEST was used to evaluate the second victim experience among the nurses (26). The tool includes 29 items in nine dimensions. The items were scored via a 5-point Likert scale, ranging from strongly disagree (1 point) to strongly agree (5 points). Items 9, 11, 15, and 25 were scored inversely. The three dimensions of psychological distress (4 items), physical distress (4 items), and professional self-efficacy (4 items) were used to measure the distress level of the second victim phenomenon. Moreover, 4 dimensions of colleague support, supervisor support (4 items), institutional support (3 items), and non-work-related support (2 items) were used to measure the supporting level of the second victim phenomenon. Finally, two dimensions of turnover intentions (2 items) and absenteeism (2 items) were applied to measure the outcomes resulting from an error.
It is of note that this study is the first to use the SVEST tool in Iran. After gaining permission from the original author of the tool (Hoffman, JM), the original version was translated into Persian and then back-translated into English by another person. In the next step, the Persian, original, and re-translated English versions were evaluated by a third person who was an expert in both Persian and English languages to approve the final Persian version. The content validity of the translated version was checked by 10 experts in the field, and the content validity index (CVI) and content validity ratio (CVR) of the tool were estimated to be 0.97 and 0.9, respectively. The Cronbach's alpha reliability scores for the SVEST dimensions also ranged from 0.78 to 0.83.
The study received approval from the Ethics Committee of Zanjan University of Medical Sciences (ethical code: IR. ZUMS. REC. 1397. 205). Written informed consent was taken from all subjects after explaining the study objectives and ensuring the confidentiality of personal information. The questionnaires were given to the nurses working in all three work shifts (morning, evening, and night), and enough time was given to the subjects to fill the questionnaires considering their workload.
The collected data were analyzed using the SPSS software (version 22). Mean, standard deviation, frequency, and percentage were used to describe the data. The skewness and kurtosis of the data were in the range of -2 to +2. The normality of data distribution was confirmed by using the Kolmogorov–Smirnov test. Missing data were replaced with mean. Pearson's correlation coefficient was used to examine the relationship between HSOPSC dimensions and the SVEST dimensions. Statistical analysis of data was carried out at a significance level of 0.05.
Results
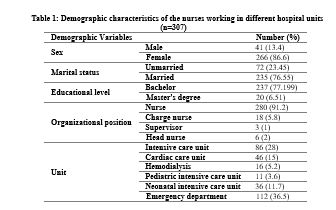
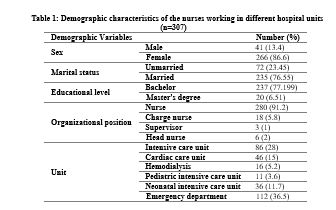
Three participants were excluded from the analysis due to having an uncompleted questionnaire. Finally, the data from 307 subjects were subjected to analysis. The mean age of the participants and their job experience were 35.15±6.86 years and 8.83±6.46 years, respectively. Most of the participants were women (86.6%), married (76.55%), and with a bachelor’s degree (77.19%) (Table 1).
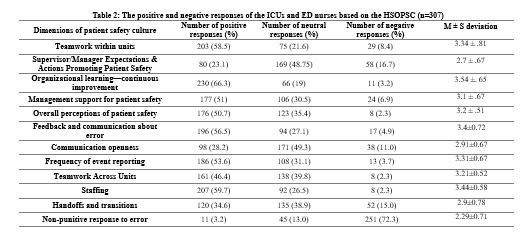
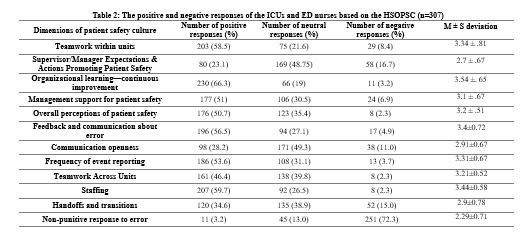
Based on the results, the HOSPSCQ components including “non-punitive response to error”, “supervisor/manager expectations”, “communication openness”, “handoffs, and teamwork across units” had an unacceptable level, while other components had an acceptable level. The “organizational learning-continuous improvement” (66.3%) was scored highest, while the “non-punitive response to error” (3.2%) was scored lowest (Table 2).
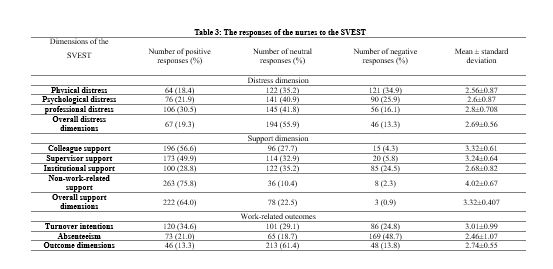
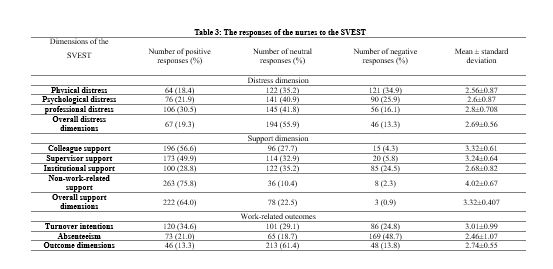
According to the responses of the subjects to the SVEST, the participants perceived the highest distress level from the professional self-efficacy dimension (30.5%). The maximum support was received from non-work-related support (75.8%) and colleague support (56.6%). The results showed that the turnover intentions dimension (34.6%) achieved the highest score (Table 3).
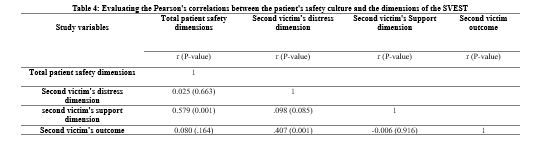
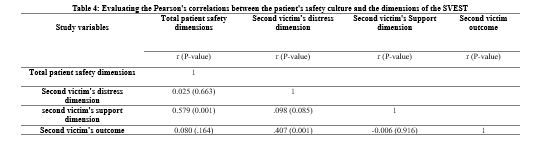
There was a significant positive correlation between the patient safety culture and the second victim's supportive sources (P=0.001). In other words, the total patient safety culture and its dimensions were associated with a sense of receiving support. However, the patient safety culture had no significant correlation with the second victim's distress rate and its outcomes. There was a significant positive correlation between the dimensions of distress and outcomes (P=0.001) (Table 4).
Discussion
The results of this study showed that out of 12 dimensions of the patient safety culture, 7 dimensions had an acceptable level. In the SVEST, the participants perceived the highest distress level from the professional self-efficacy dimension, and the maximum support was received from non-work-related support. Moreover, increasing the total patient safety culture was associated with an increased sense of receiving support. In line with the findings of previous studies, the HOSPSCQ components of organizational learning and teamwork within units received the most positive responses from the nurses (27, 28). Similar to previous studies, the components of “communication openness” and “non-punitive response to error” had an unacceptable level (29-32). In a previous study, communication and teamwork were identified as factors that could help to identify errors and improve organizational learning (27).
In this study, the subjects perceived maximum distress in their professional self-efficiency. In some studies, participants reported having unpleasant feelings and emotions as well as professional inefficacy after an adverse event and stated the weakness and inefficiency of the psychological support of the second victim (14, 33). The dimension of professional self-efficiency is affected by the supportive behavior of colleagues, supervisors, and institutions (14). In the present study, the participants received maximum support from the non-work-related environment. In Iran, people are family-centered, and the maximum support is usually received from family members. However, family support is not enough to reduce the distress level of nurses. Moreover, receiving workplace support would indeed decrease the level of professional self-efficiency distress in the second victim. It has been demonstrated that the second victim phenomenon in a non-supportive workplace could create a sense of hatred or feeling accused, victimized, judged, and embraced (14, 34, 35). Reducing punitive response to error and having encouraging, supportive coworkers, supervisors, and institutional interactions may be effective in the management of the second victim symptoms (21). In contrast with our findings, Joeste et al. reported that second victims received maximum support from their colleagues (36). Overall, studies have highlighted the importance of having supportive peers, which can contribute greatly to good safety culture (14, 35, 37).
In this study, when facing an adverse safety event, the nurses preferred the turnover of the workplace to absenteeism. Given the good social status of nursing in Iran and the reduction or absence of job opportunities in other professions, nurses continue to work in this profession regardless of the adversities and distress associated with the nursing profession. In the case of workplace turnover, nurses try to change their unit, which is usually impossible. Absenteeism can endanger their future, so it is not nurses' first choice.
Based on the findings, the patient safety culture was significantly associated with sources of support. When support from staff members against error is increased without any punitive response, the error-reporting rate is also increased. Consistent with our study, Quillivan et al. reported that punitive safety cultures may contribute to self-reported perceptions of the second victim—related psychological, physical, and professional distress, which could reflect a lack of organizational support (21). Supporting staff after safety events and informing other staff about errors reduce the incidence of errors. Studies have shown that organizational learning and having awareness of errors could help to prevent the occurrence of new errors (38, 39). Therefore, organizations should increase their support resources for staff in case of safety events.
Study limitations
The mental and emotional states of the participants during the study period were not assessed in the present study. However, to control these possible confounding factors, enough time was given to nurses to fill out the questionnaires.
Conclusion
The patient safety culture in an organization affects the behavior of the staff members following an adverse event. In this study, the subjects reported a low level of safety culture and organizational support. Since the lack of support and having a negative organizational perspective may reduce self-efficacy and increase distress as well as occurrence of errors, it is recommended to improve the supportive system for second victims. It is also suggested to research the impact of organizational support on the patient's safety culture and the second victim symptoms.
Acknowledgements
The authors would like to thank all nurses who participated in the present study.
Funding source
This article was derived from a thesis for the completion of a master’s degree in nursing, which was funded by the Research Department of Zanjan University of Medical Sciences, Zanjan, Iran.
Ethical statement
The study received approval from the Ethics Committee of Zanjan University of Medical Sciences (ethical code: IR. ZUMS. REC. 1397. 205). Written informed consent was taken from all subjects after explaining the study objectives and ensuring the confidentiality of personal information.
Conflict of interest
The authors declared no conflict of interest.
Author contributions
Study design: N.H and M.N; data gathering: A.E; statistical analysis and interpretation of the data; N.H, drafting of the manuscript: A.E; critical revision of the manuscript: N. H and; M. N, study supervision: N. H.
The safety of care is one of the most important parts of healthcare service quality that reduces negative consequences for patients (1). The safety culture aims to keep the patient safe from any damage during the care services (2). However, medical error is inevitable, even in the best patient safety cultures (3).
After an adverse event or outcome, the patient and his/her family members are considered the first victims, while the healthcare staff members are considered second victims (4). A health care provider involved in an unanticipated adverse patient event, medical error, and/or a patient-related injury is the second victim (5). The second victim may suffer from various symptoms and disorders following an adverse event (6). These symptoms include physiological disorders, sleeping disorders, job burnout, reduced job satisfaction and self-confidence, work-related stress, feeling guilty, angry, and embarrassed, and concern about punishment, dismissal, and judicial conflicts (7-14). Therefore, considering the significant effect of the second victim phenomenon on patients' safety and the physical and emotional health of healthcare personnel, supporting the second victim(s) is of utmost importance (12).
A positive patient safety culture provides an environment in which staff can easily discuss errors and achieve successful coping after an adverse event (15, 16). Promoting open discussions, support about events, and meaningful patient safety event feedback in the hospital environment could enhance the possibility of learning from mistakes and responding to errors in no punitive ways that may be beneficial for effectively coping with the second victim event (17, 18). Conversely, a patient safety culture that encourages blame, criticism, silence, or stigmatization of patient safety events can intensify the physical and psychological distress in the second victim (19-21).
Intensive care unit (ICU) and emergency department (ED) nurses are under heavy workloads and constantly deal with stressful situations. This could be frustrating and depressing for the nurses, which may ultimately increase the rate of errors (22). According to previous studies in Iran, the level of patient safety is unacceptable, and the support resources for the hospital staff are limited (20, 23, 24). Therefore, this study aimed to determine the relationship between patient safety culture and the second victim experience in ICU and ED nurses.
Methods
This cross-sectional study was conducted on ICU and ED nurses working in hospitals affiliated with the Zanjan University of Medical Sciences (Zanjan, Iran) from October to December 2019. After a pilot study on 30 nurses, the required sample size was determined as 31 using the following formula and considering 95% confidence interval and 10% dropout rate:

The subjects were enrolled via the convenience sampling method. Inclusion criteria were having at least 1 year of job experience, having a bachelor's or master's degree in nursing, and willingness to participate in the study. Nurses who did not complete questionnaires were excluded from the study.
Data were collected using a demographic information questionnaire (Sex, age, job experience, marital status, educational level, organizational position, Unit), the Persian version of the Hospital Survey on Patient Safety Culture (HSOPSC), and the Second Victim Experience and Support Tool (SVEST). The validity and reliability of the Persian version of the HOSPSCQ have been confirmed (25). In this study, the internal reliability of the tool was also confirmed by obtaining a Cronbach’s alpha of 0.83. The HOSPSCQ includes 42 items and 12 components: 1) the overall perception of patient safety, 2) organizational learning-continuous improvement, 3) supervisor/manager expectations and actions promoting patient safety, 4) teamwork within units of the organization, 5) non-punitive response to error, 6) staffing, 7) management support for patient safety, 8) teamwork across units, 9) hand-offs and transitions, 10) communication openness, 11) feedback and communication about errors, and 12) frequency of events reporting. Components 1 to 9 were scored using a 5-point Likert scale, ranging from strongly disagree (1 point) to strongly agree (5 points). Components 10 to 12 were scored from 1 (never) to 5 (always). Agree, strongly agree, sometimes, and always were considered positive responses, while disagree, strongly disagree, rarely, and never were considered negative responses. However, some items (17 items) were scored inversely. According to the questionnaire guide, the components with a minimum of 50% positive responses were considered acceptable, and those with less than 50% were considered as cases, which should be improved. In the present study, the content validity method was used to examine the validity. The reliability of the dimensions of this questionnaire was 79% to 83%.
The SVEST was used to evaluate the second victim experience among the nurses (26). The tool includes 29 items in nine dimensions. The items were scored via a 5-point Likert scale, ranging from strongly disagree (1 point) to strongly agree (5 points). Items 9, 11, 15, and 25 were scored inversely. The three dimensions of psychological distress (4 items), physical distress (4 items), and professional self-efficacy (4 items) were used to measure the distress level of the second victim phenomenon. Moreover, 4 dimensions of colleague support, supervisor support (4 items), institutional support (3 items), and non-work-related support (2 items) were used to measure the supporting level of the second victim phenomenon. Finally, two dimensions of turnover intentions (2 items) and absenteeism (2 items) were applied to measure the outcomes resulting from an error.
It is of note that this study is the first to use the SVEST tool in Iran. After gaining permission from the original author of the tool (Hoffman, JM), the original version was translated into Persian and then back-translated into English by another person. In the next step, the Persian, original, and re-translated English versions were evaluated by a third person who was an expert in both Persian and English languages to approve the final Persian version. The content validity of the translated version was checked by 10 experts in the field, and the content validity index (CVI) and content validity ratio (CVR) of the tool were estimated to be 0.97 and 0.9, respectively. The Cronbach's alpha reliability scores for the SVEST dimensions also ranged from 0.78 to 0.83.
The study received approval from the Ethics Committee of Zanjan University of Medical Sciences (ethical code: IR. ZUMS. REC. 1397. 205). Written informed consent was taken from all subjects after explaining the study objectives and ensuring the confidentiality of personal information. The questionnaires were given to the nurses working in all three work shifts (morning, evening, and night), and enough time was given to the subjects to fill the questionnaires considering their workload.
The collected data were analyzed using the SPSS software (version 22). Mean, standard deviation, frequency, and percentage were used to describe the data. The skewness and kurtosis of the data were in the range of -2 to +2. The normality of data distribution was confirmed by using the Kolmogorov–Smirnov test. Missing data were replaced with mean. Pearson's correlation coefficient was used to examine the relationship between HSOPSC dimensions and the SVEST dimensions. Statistical analysis of data was carried out at a significance level of 0.05.
Results
Three participants were excluded from the analysis due to having an uncompleted questionnaire. Finally, the data from 307 subjects were subjected to analysis. The mean age of the participants and their job experience were 35.15±6.86 years and 8.83±6.46 years, respectively. Most of the participants were women (86.6%), married (76.55%), and with a bachelor’s degree (77.19%) (Table 1).
Based on the results, the HOSPSCQ components including “non-punitive response to error”, “supervisor/manager expectations”, “communication openness”, “handoffs, and teamwork across units” had an unacceptable level, while other components had an acceptable level. The “organizational learning-continuous improvement” (66.3%) was scored highest, while the “non-punitive response to error” (3.2%) was scored lowest (Table 2).
According to the responses of the subjects to the SVEST, the participants perceived the highest distress level from the professional self-efficacy dimension (30.5%). The maximum support was received from non-work-related support (75.8%) and colleague support (56.6%). The results showed that the turnover intentions dimension (34.6%) achieved the highest score (Table 3).
There was a significant positive correlation between the patient safety culture and the second victim's supportive sources (P=0.001). In other words, the total patient safety culture and its dimensions were associated with a sense of receiving support. However, the patient safety culture had no significant correlation with the second victim's distress rate and its outcomes. There was a significant positive correlation between the dimensions of distress and outcomes (P=0.001) (Table 4).
Discussion
The results of this study showed that out of 12 dimensions of the patient safety culture, 7 dimensions had an acceptable level. In the SVEST, the participants perceived the highest distress level from the professional self-efficacy dimension, and the maximum support was received from non-work-related support. Moreover, increasing the total patient safety culture was associated with an increased sense of receiving support. In line with the findings of previous studies, the HOSPSCQ components of organizational learning and teamwork within units received the most positive responses from the nurses (27, 28). Similar to previous studies, the components of “communication openness” and “non-punitive response to error” had an unacceptable level (29-32). In a previous study, communication and teamwork were identified as factors that could help to identify errors and improve organizational learning (27).
In this study, the subjects perceived maximum distress in their professional self-efficiency. In some studies, participants reported having unpleasant feelings and emotions as well as professional inefficacy after an adverse event and stated the weakness and inefficiency of the psychological support of the second victim (14, 33). The dimension of professional self-efficiency is affected by the supportive behavior of colleagues, supervisors, and institutions (14). In the present study, the participants received maximum support from the non-work-related environment. In Iran, people are family-centered, and the maximum support is usually received from family members. However, family support is not enough to reduce the distress level of nurses. Moreover, receiving workplace support would indeed decrease the level of professional self-efficiency distress in the second victim. It has been demonstrated that the second victim phenomenon in a non-supportive workplace could create a sense of hatred or feeling accused, victimized, judged, and embraced (14, 34, 35). Reducing punitive response to error and having encouraging, supportive coworkers, supervisors, and institutional interactions may be effective in the management of the second victim symptoms (21). In contrast with our findings, Joeste et al. reported that second victims received maximum support from their colleagues (36). Overall, studies have highlighted the importance of having supportive peers, which can contribute greatly to good safety culture (14, 35, 37).
In this study, when facing an adverse safety event, the nurses preferred the turnover of the workplace to absenteeism. Given the good social status of nursing in Iran and the reduction or absence of job opportunities in other professions, nurses continue to work in this profession regardless of the adversities and distress associated with the nursing profession. In the case of workplace turnover, nurses try to change their unit, which is usually impossible. Absenteeism can endanger their future, so it is not nurses' first choice.
Based on the findings, the patient safety culture was significantly associated with sources of support. When support from staff members against error is increased without any punitive response, the error-reporting rate is also increased. Consistent with our study, Quillivan et al. reported that punitive safety cultures may contribute to self-reported perceptions of the second victim—related psychological, physical, and professional distress, which could reflect a lack of organizational support (21). Supporting staff after safety events and informing other staff about errors reduce the incidence of errors. Studies have shown that organizational learning and having awareness of errors could help to prevent the occurrence of new errors (38, 39). Therefore, organizations should increase their support resources for staff in case of safety events.
Study limitations
The mental and emotional states of the participants during the study period were not assessed in the present study. However, to control these possible confounding factors, enough time was given to nurses to fill out the questionnaires.
Conclusion
The patient safety culture in an organization affects the behavior of the staff members following an adverse event. In this study, the subjects reported a low level of safety culture and organizational support. Since the lack of support and having a negative organizational perspective may reduce self-efficacy and increase distress as well as occurrence of errors, it is recommended to improve the supportive system for second victims. It is also suggested to research the impact of organizational support on the patient's safety culture and the second victim symptoms.
Acknowledgements
The authors would like to thank all nurses who participated in the present study.
Funding source
This article was derived from a thesis for the completion of a master’s degree in nursing, which was funded by the Research Department of Zanjan University of Medical Sciences, Zanjan, Iran.
Ethical statement
The study received approval from the Ethics Committee of Zanjan University of Medical Sciences (ethical code: IR. ZUMS. REC. 1397. 205). Written informed consent was taken from all subjects after explaining the study objectives and ensuring the confidentiality of personal information.
Conflict of interest
The authors declared no conflict of interest.
Author contributions
Study design: N.H and M.N; data gathering: A.E; statistical analysis and interpretation of the data; N.H, drafting of the manuscript: A.E; critical revision of the manuscript: N. H and; M. N, study supervision: N. H.
Type of Study: Original Article |
Subject:
Nursing
References
1. Vinagre T, Marques R. Strategies for an effective safety culture and prevent errors in nursing: literature review. International journal of nursing (New York, NY). 2018;5:25-32. [View at paplisher] [DOI] [Google Scholar]
2. Lee SE, Quinn BL. Safety culture and patient safety outcomes in East Asia: a literature review. Western journal of nursing research. 2020;42(3):220-30. [View at paplisher] [DOI] [PMID] [Google Scholar]
3. Manias E, Kusljic S, Wu A. Interventions to reduce medication errors in adult medical and surgical settings: A systematic review. Therapeutic advances in drug safety. 2020;11:2042098620968309. [View at paplisher] [DOI] [PMID] [Google Scholar]
4. Werthman JA, Brown A, Cole I, Sells JR, Dharmasukrit C, Rovinski-Wagner C, et al. Second Victim Phenomenon and Nursing Support: An Integrative Review. Journal of Radiology Nursing. 2021. [View at paplisher] [DOI] [Google Scholar]
5. Edrees HH, Morlock L, Wu AW. Do hospitals support second victims? Collective insights from patient safety leaders in Maryland. The Joint Commission Journal on Quality and Patient Safety. 2017;43(9):471-83. [View at paplisher] [DOI] [PMID] [Google Scholar]
6. Marran JE. Supporting staff who are second victims after adverse healthcare events. Nursing Management. 2021;28(2). [View at paplisher] [Google Scholar]
7. Stone M. Second victim support programs for healthcare organizations. Nursing Management. 2020;51(6):38-45. [View at paplisher] [DOI] [PMID] [Google Scholar]
8. Busch IM, Moretti F, Purgato M, Barbui C, Wu AW, Rimondini M. Dealing with adverse events: a meta-analysis on second victims' coping strategies. Journal of patient safety. 2020;16(2):e51-e60. [View at paplisher] [DOI] [PMID] [Google Scholar]
9. Huang H, Chen J, Xiao M, Cao S, Zhao Q. Experiences and responses of nursing students as second victims of patient safety incidents in a clinical setting: A mixed‐methods study. Journal of Nursing Management. 2020;28(6):1317-25. [View at paplisher] [DOI] [PMID] [Google Scholar]
10. Yan L, Tan J, Chen H, Yao L, Li Y, Zhao Q, et al. Experience and support of Chinese healthcare professionals as second victims of patient safety incidents: A cross‐sectional study. Perspectives in Psychiatric Care. 2021. [View at paplisher] [DOI] [PMID] [Google Scholar]
11. Busch IM, Moretti F, Purgato M, Barbui C, Wu AW, Rimondini M. Psychological and psychosomatic symptoms of second victims of adverse events: a systematic review and meta-analysis. Journal of patient safety. 2020;16(2):e61. [View at paplisher] [DOI] [PMID] [Google Scholar]
12. Abdollahi A, Talib MA, Yaacob SN, Ismail Z. Problem-solving skills and hardiness as protective factors against stress in Iranian nurses. Issues in mental health nursing. 2014;35(2):100-7. [View at paplisher] [DOI] [PMID] [Google Scholar]
13. Garrouste-Orgeas M, Perrin M, Soufir L, Vesin A, Blot F, Maxime V, et al. The Iatroref study: medical errors are associated with symptoms of depression in ICU staff but not burnout or safety culture. Intensive care medicine. 2015;41(2):273-84. [View at paplisher] [DOI] [PMID] [Google Scholar]
14. Mohsenpour M, Hosseini M, Abbaszadeh A, Shahboulaghi FM, Khankeh H. Iranian nurses' experience of "being a wrongdoer": a phenomenological study. Nursing ethics. 2018;25(5):653-64. [View at paplisher] [DOI] [PMID] [Google Scholar]
15. Zhang X, Li Q, Guo Y, Lee SY. From organisational support to second victim‐related distress: Role of patient safety culture. Journal of nursing management. 2019;27(8):1818-25. [View at paplisher] [DOI] [PMID] [Google Scholar]
16. White RM, Delacroix R. Second victim phenomenon: Is 'just culture'a reality? An integrative review. Applied Nursing Research. 2020;56:151319. [View at paplisher] [DOI] [PMID] [Google Scholar]
17. McDaniel LR, Morris C. The second victim phenomenon: how are midwives affected? Journal of midwifery & women's health. 2020;65(4):503-11. [View at paplisher] [DOI] [PMID] [Google Scholar]
18. Mok WQ, Chin GF, Yap SF, Wang W. A cross‐sectional survey on nurses' second victim experience and quality of support resources in Singapore. Journal of nursing management. 2020;28(2):286-93. [View at paplisher] [DOI] [PMID] [Google Scholar]
19. Ferrús L, Silvestre C, Olivera G, Mira JJ. Qualitative study about the experiences of colleagues of health professionals involved in an adverse event. Journal of patient safety. 2021;17(1):36-43. [View at paplisher] [DOI] [PMID] [Google Scholar]
20. Habibzadeh H, Baghaei R, Ajoudani F. Relationship between patient safety culture and job burnout in Iranian nurses: Assessing the mediating role of second victim experience using structural equation modelling. Journal of Nursing Management. 2020;28(6):1410-7. [View at publisher] [Google Scholar] [View at paplisher] [DOI] [PMID] [Google Scholar]
21. Quillivan RR, Burlison JD, Browne EK, Scott SD, Hoffman JM. Patient safety culture and the second victim phenomenon: connecting culture to staff distress in nurses. The Joint Commission Journal on Quality and Patient Safety. 2016;42(8):377-AP2. [View at paplisher] [DOI] [Google Scholar]
22. Melnyk BM, Tan A, Hsieh AP, Gawlik K, Arslanian-Engoren C, Braun LT, et al. Critical care nurses' physical and mental health, worksite wellness support, and medical errors. American Journal of Critical Care. 2021;30(3):176-84. [View at paplisher] [DOI] [PMID] [Google Scholar]
23. Mousavi S, Faraji Khiavi F, Sharifian R, Shaham G. Study of Implementation of Safety Regulations of Radiolog Departments in has petals of Tehran University of Medical Sciences. Journal of Payavard Salamat. 2010;3(3):31-7.[Persian] [View at paplisher] [Google Scholar]
24. Phaghizadeh S, motamed N, shoghli A, Asoori M, safaean M. Assessment of Nurses Viewpoints on Patient Safety Culture in Amol Hospitals in Iran, 2012. PCNM 2015; 4 (2) :45-55. [Persian] [View at paplisher] [Google Scholar]
25. Moghri J, Arab M, Saari AA, Nateqi E, Forooshani AR, Ghiasvand H, et al. The psychometric properties of the Farsi version of "Hospital survey on patient safety culture" in Iran's hospitals. Iranian journal of public health. 2012;41(4):80. [View at paplisher] [Google Scholar]
26. Burlison JD, Scott SD, Browne EK, Thompson SG, Hoffman JM. The second victim experience and support tool (SVEST): validation of an organizational resource for assessing second victim effects and the quality of support resources. Journal of patient safety. 2017;13(2):93. [View at paplisher] [DOI] [PMID] [Google Scholar]
27. Marques TV, Rita. Strategies for an Effective Safety Culture and Prevent Errors in Nursing: Literature Review. International Journal of Nursing. 2018;5(1):25-32. [View at paplisher] [DOI] [Google Scholar]
28. El-Jardali F, Sheikh F, Garcia NA, Jamal D, Abdo A. Patient safety culture in a large teaching hospital in Riyadh: baseline assessment, comparative analysis and opportunities for improvement. BMC health services research. 2014;14(1):122. [View at paplisher] [DOI] [PMID] [Google Scholar]
29. Rezaean M, Aqaie Borz Abad P, Yazdanpanah A, Zinat Motlagh S. Patient Safety Culture Status From The Perspective Medical Staff Of Yasuj Hospitals In 2015. armaghanj 2016; 20 (10) :935-946. [Persian] [View at paplisher] [Google Scholar]
30. Ali H, Ibrahem SZ, Al Mudaf B, Al Fadalah T, Jamal D, El-Jardali F. Baseline assessment of patient safety culture in public hospitals in Kuwait. BMC health services research. 2018;18(1):158. [View at paplisher] [DOI] [PMID] [Google Scholar]
31. Alswat K, Abdalla RAM, Titi MA, Bakash M, Mehmood F, Zubairi B, et al. Improving patient safety culture in Saudi Arabia (2012-2015): trending, improvement and benchmarking. BMC health services research. 2017;17(1):516. [View at paplisher] [DOI] [PMID] [Google Scholar]
32. Azami-Aghdash S, Ebadifard Azar F, Rezapour A, Azami A, Rasi V, Klvany K. Patient safety culture in hospitals of Iran: a systematic review and meta-analysis. Med J Islam Repub Iran 2015; 29 (1) :724-736. [View at paplisher] [Google Scholar]
33. Rinaldi C, Leigheb F, Vanhaecht K, Donnarumma C, Panella M. Becoming a "second victim" in health care: pathway of recovery after adverse event. Revista de Calidad Asistencial. 2016;31:11-9. [View at paplisher] [DOI] [PMID] [Google Scholar]
34. Scott SD, Hirschinger LE, Cox KR, McCoig M, Brandt J, Hall LW. The natural history of recovery for the healthcare provider "second victim" after adverse patient events. BMJ Quality & Safety. 2009;18(5):325-30. [View at paplisher] [DOI] [PMID] [Google Scholar]
35. Chard R. How perioperative nurses define, attribute causes of, and react to intraoperative nursing errors. AORN journal. 2010;91(1):132-45. [View at paplisher] [DOI] [PMID] [Google Scholar]
36. Joesten L, Cipparrone N, Okuno-Jones S, DuBose ER. Assessing the perceived level of institutional support for the second victim after a patient safety event. Journal of patient safety. 2015;11(2):73-8. [View at paplisher] [DOI] [PMID] [Google Scholar]
37. Sirriyeh R, Lawton R, Gardner P, Armitage G. Coping with medical error: a systematic review of papers to assess the effects of involvement in medical errors on healthcare professionals' psychological well-being. Quality & Safety in Health Care. 2010;19(6):e43-e. [View at paplisher] [DOI] [PMID] [Google Scholar]
38. Burlison JD, Quillivan RR, Kath LM, Zhou Y, Courtney SC, Cheng C, et al. A Multilevel Analysis of US Hospital Patient Safety Culture Relationships With Perceptions of Voluntary Event Reporting. Journal of patient safety. 2016. [View at paplisher] [DOI] [PMID] [Google Scholar]
39. Vrbnjak D, Denieffe S, O'Gorman C, Pajnkihar M. Barriers to reporting medication errors and near misses among nurses: A systematic review. International journal of nursing studies. 2016;63:162-78. [View at paplisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





