Volume 21, Issue 4 (12-2024)
J Res Dev Nurs Midw 2024, 21(4): 41-46 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Beirami A, Rahemi Z. Investigating the effect of mindfulness-based art therapy on self-efficacy of multiparous and nulliparous women: A randomized controlled trial. J Res Dev Nurs Midw 2024; 21 (4) :41-46
URL: http://nmj.goums.ac.ir/article-1-1872-en.html
URL: http://nmj.goums.ac.ir/article-1-1872-en.html
1- Department of Nursing, Bandar Abbas Branch, Islamic Azad University, Bandar Abbas, Iran
2- School of Nursing, Clemson University, Carolina, United States ,zrahemi@clemson.edu
2- School of Nursing, Clemson University, Carolina, United States ,
Full-Text [PDF 653 kb]
(765 Downloads)
| Abstract (HTML) (2497 Views)
Discussion
This study was conducted with the purpose of determining the effect of mindfulness-based art therapy on the self-efficacy of multiparous and nulliparous women. It was designed as an experimental study with a control group. The data analysis revealed no significant differences in background variables among the three groups. The results of the present study showed that mindfulness-based art therapy during pregnancy can increase the self-efficacy of women in both intervention groups. Our results are consistent with the findings of related studies.
Relevant studies indicated that the self-efficacy of pregnant women, including their choices regarding delivery type, adaptation to labor, and postpartum care, can be improved through educational programs such as childbirth preparation classes. Several studies have demonstrated the effectiveness of psychological interventions, such as education and counseling, in building and strengthening self-efficacy. These studies suggest that psychological counseling aimed at educating and increasing the awareness of pregnant women can empower them (12-14). Psychological interventions aimed at enhancing the self-efficacy of pregnant women can help reduce the fear of childbirth, particularly in first-time mothers. The use of an educational intervention based on self-efficacy theory had positive effects on the awareness of self-care and the behaviors of the participants. Moreover, self-efficacy-based training led to an increase in health-promoting behaviors, especially physical activity and motivational skills (Self-control and sense of self-efficacy) (15,16). Implementing an awareness-raising intervention can effectively improve pregnant women’s understanding of the benefits and safety of physical activity during pregnancy, while also enhancing their self-efficacy to engage in physical activity (17).
Nezamian et al. investigated the effect of cognitive-behavioral therapy on sexual function and sexual self-efficacy in pregnant women. Their study showed that cognitive-behavioral therapy-based counseling improved sexual function and sexual self-efficacy in pregnant women compared to routine prenatal care. The group that received eight consecutive weeks of counseling had higher sexual function and self-efficacy scores than the control group that received only routine prenatal care (18). An investigation into the effect of an educational intervention based on self-efficacy theory and health literacy on pregnancy outcomes showed that the intervention effectively improved maternal health literacy and self-efficacy. This, in turn, led to favorable pregnancy outcomes, including the birth of a normal-weight baby (19). Additionally, it was found that childbirth preparation classes enhance mothers’ ability to adapt to labor and delivery, with participants showing higher self-efficacy after attending the classes, which aligns with the results of the present study. However, no significant difference was observed in childbirth self-efficacy between the control and intervention groups. This could be attributed to differences in the educational content and the number of sessions (Three sessions) provided (11).
In the present study, the results of the comparison between the groups before the intervention, immediately after the intervention, and four weeks after the intervention showed no significant difference in the mindfulness score between the two intervention groups and the control group. However, the mean mindfulness score was significantly higher in both intervention groups compared to the control group immediately after the intervention and four weeks after the intervention, with a notable increase in the intervention groups. This suggests that mindfulness-based art therapy has a positive effect on increasing mindfulness in the intervention groups. In line with the present study, Venti and Rustin found that pregnant mothers who received a mindfulness-based intervention experienced a significant decrease in anxiety levels during the third trimester of pregnancy compared to the control group (28). Furthermore, mindfulness-based group therapy was found to reduce depression and anxiety both during pregnancy and postpartum (29). Given that the results of these studies align with the present study, it is important to note that an increase in mindfulness scores can be a key condition for the effectiveness of various mindfulness-based interventions on desired outcomes. As mindfulness increases, participants experience a decrease in stress, depression, anxiety, and fear of childbirth (3-5). Practicing mindfulness-based yoga during the second trimester of pregnancy leads to a decrease in perceived stress and anxiety during the third trimester (10). In a study investigating the effect of mindfulness-based counseling on anxiety during pregnancy and the physiological parameters of newborns, the results showed that mindfulness-based counseling effectively reduced anxiety during pregnancy (6).
Traditionally, the primary goal of a cesarean section was to save the lives of mothers at risk of death due to conditions such as labor arrest. However, in recent years, the indications for cesarean sections have expanded, leading to an increased rate of unnecessary procedures. This trend has placed both the mother and fetus at risk of various health conditions. While cesarean sections are necessary for 10-15% of deliveries, studies suggest that approximately 35-90% of deliveries could be performed naturally without any medical intervention (7,8). In recent years, cesarean section has become one of the most common surgeries among women (8). In the present study, the results showed that the preferred method of delivery in all study groups before the intervention was cesarean section. However, after the intervention, the majority of participants who received the mindfulness intervention preferred natural delivery. Another study indicated that higher levels of perceived stress are associated with an increased likelihood of choosing cesarean section as an elective method of delivery (30). These findings highlight the importance of implementing strategies to reduce perceived stress in pregnant women, which may help decrease the rate of choosing cesarean section as an elective method of delivery. In the present study, mindfulness-based art therapy was used to enhance preparedness and increase self-efficacy in women. As a result, women in the intervention group showed a preference for natural childbirth, reflecting the positive impact of increased self-efficacy among the participants.
Conclusion
The results of this study suggest that mindfulness-based art therapy classes for pregnant women are an effective intervention for enhancing self-efficacy and mindfulness. These improvements can play a significant role in empowering women to make informed decisions about their preferred method of delivery, leading to a preference for natural childbirth. By addressing the lack of self-efficacy, this intervention can help reduce unnecessary cesarean sections, thereby improving maternal and fetal health outcomes. The findings highlight the potential of mindfulness-based approaches in promoting better pregnancy experiences and outcomes, ultimately contributing to the reduction of complications associated with childbirth. Therefore, it is recommended that individuals with a fear of childbirth, especially primiparous women, be identified and assessed during pregnancy, as these women can benefit from receiving interventions similar to the one used in this study.
Acknowledgement
The authors thank the pregnant women who participated in the study for their support in conducting this research.
Funding sources
None.
Ethical statement
The code of ethics was obtained from Hormozgan University of Medical Sciences (IR.HUMS.REC.1403.156). Informed consent was obtained from participants before entering the study. The information of the study participants remained confidential. The principles of ethics in human research were observed. Withdrawal from the intervention sessions in this study was completely voluntary; there was no compulsion to continue the intervention sessions. Thirty-one ethical codes related to medical science studies were followed during the study.
Conflicts of interest
The authors declare that they have no competing interests.
Author contributions
All authors read and approved the final manuscript. All authors take responsibility for the integrity of the data and the accuracy of the data analysis.
Full-Text: (512 Views)
Introduction
Pregnancy and childbirth are among the most significant events in a woman's life. Labor pain is one of the most intense pains women can experience (1,2). Natural childbirth follows a physiological process that begins with a series of pains, which gradually become more intense and frequent, culminating in the final stage with the expulsion of the fetus (2,3). The experience of severe pain during labor can lead to varying levels of fear in pregnant women, ranging from rational concerns to an extreme fear of childbirth (3). A certain level of fear, as a natural protective psychological response, helps pregnant women prepare for and address challenges during childbirth. An important factor influencing fear of childbirth is self-efficacy. Childbirth self-efficacy refers to a woman’s confidence in her ability to successfully navigate the childbirth process. Women assess their capacity to manage various aspects of childbirth and make decisions accordingly (4-6). Therefore, if a woman believes that childbirth is too difficult or impossible for her, she is likely to exhibit behaviors that align with this perception (7). Self-efficacy in pregnant women refers to their assessment of their ability to cope with stressful situations and respond appropriately, particularly during labor and delivery. Women with low self-efficacy are more likely to perceive natural childbirth as unattainable and experience significant fear during pregnancy. Consequently, self-efficacy plays a crucial role in determining their choice of delivery method (8). As a personal resource, self-efficacy supports adaptation to challenging situations, including childbirth (9).
Recent studies indicate that self-efficacy significantly influences labor and delivery, shaping pregnant women’s motivation and attitude toward natural childbirth. Women with lower confidence in their ability to cope with labor tend to experience greater pain during childbirth (10,11). As previously mentioned, self-efficacy is directly related to the fear of childbirth (11-13). The resultant maternal anxiety and fear have been associated with outcomes such as preterm or late delivery, low birth weight, and intrauterine growth restriction (14). In the case of the fetus, anxiety can reduce nutrient and oxygen supply, as well as decrease cord blood flow. Elevated cortisol levels may result in the birth of a more vulnerable and anxious newborn (15,16). In addition, these newborns are exposed to the medications prescribed to alleviate the mother’s anxiety symptoms. After birth, children of anxious mothers often experience lower-than-normal early life functions. Maternal anxiety can also serve as a risk factor for delayed mental and motor development in the newborn (17). Maternal distress during the prenatal period can impact the fetus in utero. Prolonged maternal distress, for example, may make the child more sensitive and prone to anxiety and depressive disorders during childhood and adolescence (14). High levels of cortisol in the amniotic fluid can also impact fetal brain development, adversely affecting brain regions responsible for social skills, language, and memory (18). A woman’s mental state, particularly her level of anxiety during pregnancy and the postpartum period, as well as how she adapts to these challenges, can impact her own postpartum mental health, her child’s well-being, and the overall family dynamics (14). Low self-efficacy is considered one of the main reasons for the increased demand for cesarean sections among mothers (19).
To create an appropriate supportive and therapeutic environment for women with fear of childbirth, a multidisciplinary approach and interdisciplinary collaboration among all healthcare providers involved in the process are essential (20). Complementary treatments have been shown to be effective in enhancing health in various medical and non-medical conditions (21,4). Art therapy, as a comprehensive treatment method, holds promise for managing a range of psychological issues before and after childbirth, although it has not been extensively studied. As a creative form of psychotherapy, art therapy can be used to address severe mental distress, trauma, and crisis reactions (21). Without forcing individuals to talk, art therapy encourages them to transform their fears and conflicts into new representations, empowering them as mothers (12). Art activities appear to enhance quality of life by increasing mindfulness. Mindfulness is defined as the awareness that arises from paying intentional attention to the present moment, without judgment, allowing individuals to observe and accept physical sensations and emotions as they occur (15,16). Combining mindfulness concepts with art therapy has resulted in a treatment known as mindfulness-based art therapy or focused art therapy. This approach is a subset of the contemplative method first proposed by Rappaport (18,19). In this type of therapy, the main elements of mindfulness are integrated into an artistic process. In other words, the individual engages in a creative activity as a means of self-exploration (20). Fear of childbirth is an indicator that women may need intervention (18). Given the possibility that fear of childbirth may differ between nulliparous and multiparous women, and based on the team's knowledge and an extensive search of available databases, no clinical trial has yet examined the effect of mindfulness-based art therapy on increasing self-efficacy, either in Iran or internationally. Given that mindfulness-based art therapy can impact women’s quality of life and mental health (16), this study was conducted to determine its effect on self-efficacy in nulliparous and multiparous women.
Methods
The present study was a randomized controlled trial with two parallel arms: two intervention groups and one control group. The population of the study included multiparous and nulliparous pregnant women who visited health centers (Both urban and rural), clinics, private offices, and maternity centers in a southern city of Iran (Bandar Abbas) for prenatal care. After the project was approved by the university research council and the ethics committee of Hormozgan University of Medical Sciences, the researcher visited the centers, providing a written introduction for participation. The research samples in this study consisted of individuals from the research population who met the inclusion criteria. The sampling process began in May 2024. A convenience sampling method was used, where an initial call for participation was posted in health centers, clinics, private offices, and maternity centers in Bandar Abbas, Iran. Additionally, advertisements were shared through social networks and pregnancy groups. Nulliparous and multiparous pregnant women who were 26-28 weeks pregnant and either experienced fear of childbirth or preferred cesarean section due to this fear were invited to participate.
A total of 90 eligible individuals were included in the study. At each stage of sampling, participants were randomly assigned to the intervention and control groups using a blocked random allocation method. The sample size in this study was calculated based on a difference of 10 points in the mean fear of childbirth score and a standard deviation of 1.13, according to Toohill’s study (20), and considering a significance level of 5% and a test power of 90%.
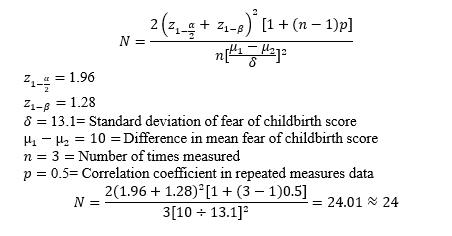
The number of samples determined in each group was 24. Considering a 20% dropout rate, the number of samples in each group increased to 29, and the total sample size was 87. To ensure reliability, a total sample size of 90 was considered.
However, at the time of the results announcement, two individuals in the multiparous group and two individuals in the nulliparous group were excluded due to bleeding, labor, and severe hypertension related to previous pregnancy. The inclusion criteria were: gestational age of 26-28 weeks (Given the higher prevalence of fear of childbirth in the third trimester of pregnancy) (14), attendance at the number of intervention and follow-up sessions, single pregnancy, living with a spouse, Iranian nationality, and fluency in Persian. The exclusion criteria were: high-risk pregnancy, pregnancy through assisted reproductive methods, experience of recurrent miscarriage (Two or more times), history of psychiatric illnesses (Schizophrenia, bipolar disorders, and severe depression) or having them at the time of the study as self-reported or recorded in the file, use of psychiatric medications, drug abuse, alcohol consumption, having chronic physical diseases, and receiving other treatment methods or participating in other interventions to control stress, anxiety, and fear (22-25).
The blocked random allocation method was used to randomly assign the samples to three groups: the intervention group (Art therapy based on mindfulness) and the control group (Routine care). Blocks of four were used for this purpose. Specifically, all six participants were grouped together as a block. The blocks had the combinations TnTnCCTmTm, CTnTnTmTmC, and CTnCTn, where Tn represents the nulliparous intervention group, Tm represents the multiparous intervention group, and C represents the control group. Each block had a unique code. Based on the sample size (n=90), 15 blocks, each consisting of six participants, were selected. For example, four participants in the TnTnCCTmTm block were assigned to the null intervention, control, and multi-intervention groups. To conceal the allocation, 90 envelopes were prepared, each labeled with a number from 1 to 90. The group assignments were placed inside the envelopes based on the computer-generated program. The researcher opened the envelopes sequentially, and the participants were randomly assigned to either the intervention or control group. All steps were conducted using random assignment software (2.0.0) and under the supervision of a statistician. In this study, three tools were used to collect data before, immediately after, and four weeks after the intervention. These tools included: a) the Demographic-Socio-Reproductive Characteristics Questionnaire, b) the Iranian Childbirth Self-Efficacy Questionnaire, and c) the Five-Factor Mindfulness Questionnaire. Each of these tools is described below.
A) The demographic-socio-reproductive characteristics questionnaire included questions such as age, gestational age, duration of marriage, education level, spouse's education level, job position, spouse’s job, type of residence, housing status, satisfaction with socio-economic status, satisfaction with personal economic status, pregnancy status, family support, source of information about childbirth, and participation in childbirth preparation classes.
B) The Iranian childbirth self-efficacy questionnaire was designed by Lowe based on the Childbirth Self-Efficacy Questionnaire to measure a mother’s confidence in her ability to give birth (23). This scale is a 62-item self-report instrument that is scored on a Likert scale from 1 to 10. The minimum score on this questionnaire is 62, and the maximum score is 620. This questionnaire consists of two parts: the active phase and the second stage of labor, and each of these parts has two separate sections. The first dimension is self-efficacy a, which includes 15 questions measuring outcome expectations related to the active stage of labor, as well as 15 questions assessing self-efficacy expectations for this stage. The second dimension is self-efficacy b, which pertains to the second stage of labor and is divided into two sections with 16 questions (Outcome expectations and self-efficacy). Lowe estimated the reliability of this questionnaire using the internal consistency method for the subscales, which ranged from 0.86 to 0.95. The convergent validity of the questionnaire has also been confirmed through positive and significant correlations with the general self-efficacy, self-esteem, and internal locus of control questionnaires (22). By removing the repeated items from Lowe’s questionnaire, et al., a short form of the Childbirth Self-Efficacy Questionnaire was designed, which consists of two 16-item sections. The findings of this study showed high internal consistency (Cronbach's alpha 0.96) and test-retest reliability (Internal correlation coefficient between the two subscales 0.88) (23). To adapt this questionnaire to Iranian culture, Danielson et al. added two religion-related items to each of the subscales of the 32-item Childbirth Self-Efficacy Questionnaire. As a result, this questionnaire has 18 items in each subscale, which are scored on a Likert scale from 1 to 10 points. Therefore, this scale has a minimum of 36 and a maximum of 360 points. The reliability and validity of this questionnaire within Iran were evaluated in the study by Danielson et al. Content validity was confirmed by experts. Factor analysis supported the two-factor conceptual structure of the measure and, therefore, supported its construct validity. Cronbach’s alpha of 0.92 for the entire scale and 0.88 for each of the subscales indicates good internal consistency (24). Consequently, due to the validity and acceptability of the Iranian Childbirth Self-Efficacy Questionnaire in the study by Khorsandi et al., it was used in this study.
C) The five-factor mindfulness questionnaire is a 39-item self-rating scale developed by Baer et al. in 2006 by combining items from the Freiberg Mindfulness Inventory, the Mindfulness Awareness and Attention Scale, the Konczuk Mindfulness Scale, the Revised Cognitive and Emotional Mindfulness Scale, and the Southampton Mindfulness Inventory using a factor analysis approach. Bauer conducted a factor analysis on a sample of university students. The internal consistency of the questionnaire factors was good, with alpha coefficients for observation being 0.83, action with mindfulness being 0.87, non-judgmentalness toward inner experience being 0.87, description being 0.91, and non-reactivity being 0.75. The correlations between the factors were moderate and statistically significant, ranging from 0.15 to 0.34. The observing factor involves paying attention to external and internal stimuli such as feelings, cognitions, emotions, sounds, and smells. Describing involves naming external experiences with words, and mindful action involves acting with full presence of mind at all times, as opposed to mechanical action that occurs when one’s mind is elsewhere. Nonjudgmental toward internal experience involves being nonjudgmental toward thoughts and feelings, and nonreactive to internal experience involves allowing internal thoughts and feelings to come and go without getting caught up in them. This scale is a self-report instrument that is scored on a Likert scale from 1 (Never or very rarely) to 5 (Often or always). The range of scores is from 39 to 195. Items 3, 5, 8, 10, 12, 13, 14, 16, 17, 18, 22, 23, 25, 28, 30, 34, 35, 38, and 39 are scored in reverse order. The higher the score, the greater the mindfulness (25). According to the results, the internal consistency of the factors was adequate, with alpha coefficients ranging from 0.75 (For the non-reactive factor) to 0.91 (For the descriptive factor). The correlation between the factors was moderate and significant in all cases, ranging from 0.15 to 0.34. In a study conducted on the validity and reliability of this questionnaire in Iran, the test-retest correlation coefficients ranged from r=0.57 (For the non-judgmental factor) to r=0.84 (For the observational factor). Moreover, the alpha coefficients ranged from 0.55 (For the non-reactive factor) to 0.83 (For the descriptive factor), which was acceptable (26,27).
Intervention
The number of participants in the group therapy sessions ranged from 3 to 15, depending on the type of group. Prior to the sessions, the necessary details regarding the days, locations, and times were communicated to the members of the intervention group either in person or through direct contact. Additionally, after obtaining consent, a WhatsApp group was created for each intervention group to facilitate communication and interaction. Sessions at the Bandar Abbas Counseling Center were held on Sundays and Tuesdays by a psychology master’s student trained in mindfulness-based art therapy, under the supervision of the research team. Participants in both the intervention and control groups completed the questionnaires three times: before the intervention, immediately after the intervention, and four weeks later. Due to the nature of the intervention, it was not possible to blind the participants or the researcher responsible for delivering the intervention. To control for evaluator bias, blinding was implemented for those responsible for data collection and analysis.
Structure of treatment
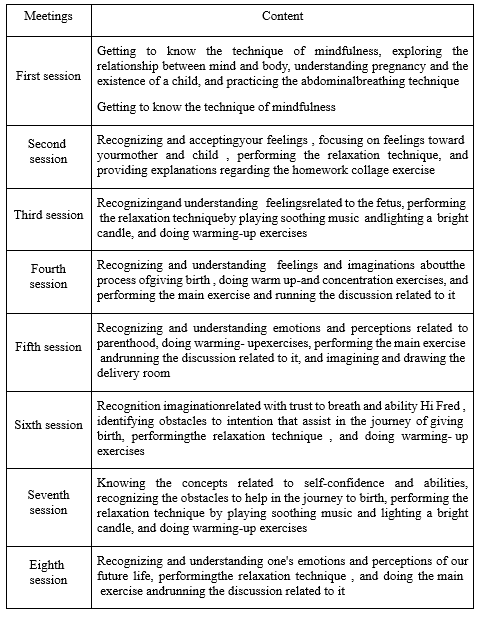
Evaluation of the program: The content validity of the intervention program was assessed by a group of relevant experts, including a midwife, psychiatrist, clinical psychologist, and art therapy specialist (14-17). The content of the meeting schedule was as follows: After completing the final questionnaire (Four weeks after the intervention), a brief mindfulness-based art therapy session was conducted for the control group to allow them to benefit from the study. During this session, their questions regarding the fear of childbirth were addressed (Table 1).
Pregnancy and childbirth are among the most significant events in a woman's life. Labor pain is one of the most intense pains women can experience (1,2). Natural childbirth follows a physiological process that begins with a series of pains, which gradually become more intense and frequent, culminating in the final stage with the expulsion of the fetus (2,3). The experience of severe pain during labor can lead to varying levels of fear in pregnant women, ranging from rational concerns to an extreme fear of childbirth (3). A certain level of fear, as a natural protective psychological response, helps pregnant women prepare for and address challenges during childbirth. An important factor influencing fear of childbirth is self-efficacy. Childbirth self-efficacy refers to a woman’s confidence in her ability to successfully navigate the childbirth process. Women assess their capacity to manage various aspects of childbirth and make decisions accordingly (4-6). Therefore, if a woman believes that childbirth is too difficult or impossible for her, she is likely to exhibit behaviors that align with this perception (7). Self-efficacy in pregnant women refers to their assessment of their ability to cope with stressful situations and respond appropriately, particularly during labor and delivery. Women with low self-efficacy are more likely to perceive natural childbirth as unattainable and experience significant fear during pregnancy. Consequently, self-efficacy plays a crucial role in determining their choice of delivery method (8). As a personal resource, self-efficacy supports adaptation to challenging situations, including childbirth (9).
Recent studies indicate that self-efficacy significantly influences labor and delivery, shaping pregnant women’s motivation and attitude toward natural childbirth. Women with lower confidence in their ability to cope with labor tend to experience greater pain during childbirth (10,11). As previously mentioned, self-efficacy is directly related to the fear of childbirth (11-13). The resultant maternal anxiety and fear have been associated with outcomes such as preterm or late delivery, low birth weight, and intrauterine growth restriction (14). In the case of the fetus, anxiety can reduce nutrient and oxygen supply, as well as decrease cord blood flow. Elevated cortisol levels may result in the birth of a more vulnerable and anxious newborn (15,16). In addition, these newborns are exposed to the medications prescribed to alleviate the mother’s anxiety symptoms. After birth, children of anxious mothers often experience lower-than-normal early life functions. Maternal anxiety can also serve as a risk factor for delayed mental and motor development in the newborn (17). Maternal distress during the prenatal period can impact the fetus in utero. Prolonged maternal distress, for example, may make the child more sensitive and prone to anxiety and depressive disorders during childhood and adolescence (14). High levels of cortisol in the amniotic fluid can also impact fetal brain development, adversely affecting brain regions responsible for social skills, language, and memory (18). A woman’s mental state, particularly her level of anxiety during pregnancy and the postpartum period, as well as how she adapts to these challenges, can impact her own postpartum mental health, her child’s well-being, and the overall family dynamics (14). Low self-efficacy is considered one of the main reasons for the increased demand for cesarean sections among mothers (19).
To create an appropriate supportive and therapeutic environment for women with fear of childbirth, a multidisciplinary approach and interdisciplinary collaboration among all healthcare providers involved in the process are essential (20). Complementary treatments have been shown to be effective in enhancing health in various medical and non-medical conditions (21,4). Art therapy, as a comprehensive treatment method, holds promise for managing a range of psychological issues before and after childbirth, although it has not been extensively studied. As a creative form of psychotherapy, art therapy can be used to address severe mental distress, trauma, and crisis reactions (21). Without forcing individuals to talk, art therapy encourages them to transform their fears and conflicts into new representations, empowering them as mothers (12). Art activities appear to enhance quality of life by increasing mindfulness. Mindfulness is defined as the awareness that arises from paying intentional attention to the present moment, without judgment, allowing individuals to observe and accept physical sensations and emotions as they occur (15,16). Combining mindfulness concepts with art therapy has resulted in a treatment known as mindfulness-based art therapy or focused art therapy. This approach is a subset of the contemplative method first proposed by Rappaport (18,19). In this type of therapy, the main elements of mindfulness are integrated into an artistic process. In other words, the individual engages in a creative activity as a means of self-exploration (20). Fear of childbirth is an indicator that women may need intervention (18). Given the possibility that fear of childbirth may differ between nulliparous and multiparous women, and based on the team's knowledge and an extensive search of available databases, no clinical trial has yet examined the effect of mindfulness-based art therapy on increasing self-efficacy, either in Iran or internationally. Given that mindfulness-based art therapy can impact women’s quality of life and mental health (16), this study was conducted to determine its effect on self-efficacy in nulliparous and multiparous women.
Methods
The present study was a randomized controlled trial with two parallel arms: two intervention groups and one control group. The population of the study included multiparous and nulliparous pregnant women who visited health centers (Both urban and rural), clinics, private offices, and maternity centers in a southern city of Iran (Bandar Abbas) for prenatal care. After the project was approved by the university research council and the ethics committee of Hormozgan University of Medical Sciences, the researcher visited the centers, providing a written introduction for participation. The research samples in this study consisted of individuals from the research population who met the inclusion criteria. The sampling process began in May 2024. A convenience sampling method was used, where an initial call for participation was posted in health centers, clinics, private offices, and maternity centers in Bandar Abbas, Iran. Additionally, advertisements were shared through social networks and pregnancy groups. Nulliparous and multiparous pregnant women who were 26-28 weeks pregnant and either experienced fear of childbirth or preferred cesarean section due to this fear were invited to participate.
A total of 90 eligible individuals were included in the study. At each stage of sampling, participants were randomly assigned to the intervention and control groups using a blocked random allocation method. The sample size in this study was calculated based on a difference of 10 points in the mean fear of childbirth score and a standard deviation of 1.13, according to Toohill’s study (20), and considering a significance level of 5% and a test power of 90%.
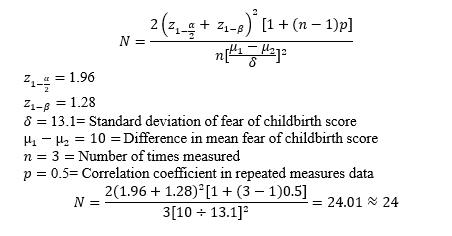
The number of samples determined in each group was 24. Considering a 20% dropout rate, the number of samples in each group increased to 29, and the total sample size was 87. To ensure reliability, a total sample size of 90 was considered.
However, at the time of the results announcement, two individuals in the multiparous group and two individuals in the nulliparous group were excluded due to bleeding, labor, and severe hypertension related to previous pregnancy. The inclusion criteria were: gestational age of 26-28 weeks (Given the higher prevalence of fear of childbirth in the third trimester of pregnancy) (14), attendance at the number of intervention and follow-up sessions, single pregnancy, living with a spouse, Iranian nationality, and fluency in Persian. The exclusion criteria were: high-risk pregnancy, pregnancy through assisted reproductive methods, experience of recurrent miscarriage (Two or more times), history of psychiatric illnesses (Schizophrenia, bipolar disorders, and severe depression) or having them at the time of the study as self-reported or recorded in the file, use of psychiatric medications, drug abuse, alcohol consumption, having chronic physical diseases, and receiving other treatment methods or participating in other interventions to control stress, anxiety, and fear (22-25).
The blocked random allocation method was used to randomly assign the samples to three groups: the intervention group (Art therapy based on mindfulness) and the control group (Routine care). Blocks of four were used for this purpose. Specifically, all six participants were grouped together as a block. The blocks had the combinations TnTnCCTmTm, CTnTnTmTmC, and CTnCTn, where Tn represents the nulliparous intervention group, Tm represents the multiparous intervention group, and C represents the control group. Each block had a unique code. Based on the sample size (n=90), 15 blocks, each consisting of six participants, were selected. For example, four participants in the TnTnCCTmTm block were assigned to the null intervention, control, and multi-intervention groups. To conceal the allocation, 90 envelopes were prepared, each labeled with a number from 1 to 90. The group assignments were placed inside the envelopes based on the computer-generated program. The researcher opened the envelopes sequentially, and the participants were randomly assigned to either the intervention or control group. All steps were conducted using random assignment software (2.0.0) and under the supervision of a statistician. In this study, three tools were used to collect data before, immediately after, and four weeks after the intervention. These tools included: a) the Demographic-Socio-Reproductive Characteristics Questionnaire, b) the Iranian Childbirth Self-Efficacy Questionnaire, and c) the Five-Factor Mindfulness Questionnaire. Each of these tools is described below.
A) The demographic-socio-reproductive characteristics questionnaire included questions such as age, gestational age, duration of marriage, education level, spouse's education level, job position, spouse’s job, type of residence, housing status, satisfaction with socio-economic status, satisfaction with personal economic status, pregnancy status, family support, source of information about childbirth, and participation in childbirth preparation classes.
B) The Iranian childbirth self-efficacy questionnaire was designed by Lowe based on the Childbirth Self-Efficacy Questionnaire to measure a mother’s confidence in her ability to give birth (23). This scale is a 62-item self-report instrument that is scored on a Likert scale from 1 to 10. The minimum score on this questionnaire is 62, and the maximum score is 620. This questionnaire consists of two parts: the active phase and the second stage of labor, and each of these parts has two separate sections. The first dimension is self-efficacy a, which includes 15 questions measuring outcome expectations related to the active stage of labor, as well as 15 questions assessing self-efficacy expectations for this stage. The second dimension is self-efficacy b, which pertains to the second stage of labor and is divided into two sections with 16 questions (Outcome expectations and self-efficacy). Lowe estimated the reliability of this questionnaire using the internal consistency method for the subscales, which ranged from 0.86 to 0.95. The convergent validity of the questionnaire has also been confirmed through positive and significant correlations with the general self-efficacy, self-esteem, and internal locus of control questionnaires (22). By removing the repeated items from Lowe’s questionnaire, et al., a short form of the Childbirth Self-Efficacy Questionnaire was designed, which consists of two 16-item sections. The findings of this study showed high internal consistency (Cronbach's alpha 0.96) and test-retest reliability (Internal correlation coefficient between the two subscales 0.88) (23). To adapt this questionnaire to Iranian culture, Danielson et al. added two religion-related items to each of the subscales of the 32-item Childbirth Self-Efficacy Questionnaire. As a result, this questionnaire has 18 items in each subscale, which are scored on a Likert scale from 1 to 10 points. Therefore, this scale has a minimum of 36 and a maximum of 360 points. The reliability and validity of this questionnaire within Iran were evaluated in the study by Danielson et al. Content validity was confirmed by experts. Factor analysis supported the two-factor conceptual structure of the measure and, therefore, supported its construct validity. Cronbach’s alpha of 0.92 for the entire scale and 0.88 for each of the subscales indicates good internal consistency (24). Consequently, due to the validity and acceptability of the Iranian Childbirth Self-Efficacy Questionnaire in the study by Khorsandi et al., it was used in this study.
C) The five-factor mindfulness questionnaire is a 39-item self-rating scale developed by Baer et al. in 2006 by combining items from the Freiberg Mindfulness Inventory, the Mindfulness Awareness and Attention Scale, the Konczuk Mindfulness Scale, the Revised Cognitive and Emotional Mindfulness Scale, and the Southampton Mindfulness Inventory using a factor analysis approach. Bauer conducted a factor analysis on a sample of university students. The internal consistency of the questionnaire factors was good, with alpha coefficients for observation being 0.83, action with mindfulness being 0.87, non-judgmentalness toward inner experience being 0.87, description being 0.91, and non-reactivity being 0.75. The correlations between the factors were moderate and statistically significant, ranging from 0.15 to 0.34. The observing factor involves paying attention to external and internal stimuli such as feelings, cognitions, emotions, sounds, and smells. Describing involves naming external experiences with words, and mindful action involves acting with full presence of mind at all times, as opposed to mechanical action that occurs when one’s mind is elsewhere. Nonjudgmental toward internal experience involves being nonjudgmental toward thoughts and feelings, and nonreactive to internal experience involves allowing internal thoughts and feelings to come and go without getting caught up in them. This scale is a self-report instrument that is scored on a Likert scale from 1 (Never or very rarely) to 5 (Often or always). The range of scores is from 39 to 195. Items 3, 5, 8, 10, 12, 13, 14, 16, 17, 18, 22, 23, 25, 28, 30, 34, 35, 38, and 39 are scored in reverse order. The higher the score, the greater the mindfulness (25). According to the results, the internal consistency of the factors was adequate, with alpha coefficients ranging from 0.75 (For the non-reactive factor) to 0.91 (For the descriptive factor). The correlation between the factors was moderate and significant in all cases, ranging from 0.15 to 0.34. In a study conducted on the validity and reliability of this questionnaire in Iran, the test-retest correlation coefficients ranged from r=0.57 (For the non-judgmental factor) to r=0.84 (For the observational factor). Moreover, the alpha coefficients ranged from 0.55 (For the non-reactive factor) to 0.83 (For the descriptive factor), which was acceptable (26,27).
Intervention
The number of participants in the group therapy sessions ranged from 3 to 15, depending on the type of group. Prior to the sessions, the necessary details regarding the days, locations, and times were communicated to the members of the intervention group either in person or through direct contact. Additionally, after obtaining consent, a WhatsApp group was created for each intervention group to facilitate communication and interaction. Sessions at the Bandar Abbas Counseling Center were held on Sundays and Tuesdays by a psychology master’s student trained in mindfulness-based art therapy, under the supervision of the research team. Participants in both the intervention and control groups completed the questionnaires three times: before the intervention, immediately after the intervention, and four weeks later. Due to the nature of the intervention, it was not possible to blind the participants or the researcher responsible for delivering the intervention. To control for evaluator bias, blinding was implemented for those responsible for data collection and analysis.
Structure of treatment
Evaluation of the program: The content validity of the intervention program was assessed by a group of relevant experts, including a midwife, psychiatrist, clinical psychologist, and art therapy specialist (14-17). The content of the meeting schedule was as follows: After completing the final questionnaire (Four weeks after the intervention), a brief mindfulness-based art therapy session was conducted for the control group to allow them to benefit from the study. During this session, their questions regarding the fear of childbirth were addressed (Table 1).
Data analysis
The description of the variables was reported in terms of frequency, percentage, mean, and standard deviation. The assumption of normality was tested using the Shapiro-Wilk test, and the results indicated a normal distribution. Based on this, parametric tests were applied. An independent t-test was used to compare the means of quantitative variables between the two groups, while the chi-square test (Fisher’s exact test) was employed to compare the frequencies of qualitative variables. To compare the mean scores of response variables over time, the repeated measures ANOVA test was utilized. To examine the effectiveness of the intervention, a repeated measures test was performed with the effect size reported. Data analysis was conducted using SPSS version 26 software, and a significance level of less than 0.05 was considered statistically significant.
Results
The results indicated that the distribution of variables such as age, gestational age, duration of marriage, education, employment status, type of residence, satisfaction with socioeconomic status, and participation in childbirth preparation classes were similar between the two intervention and control groups (Table 2).
The study results indicated that the preferred method of delivery before the intervention was similar across the three groups. Most women in all groups preferred cesarean section, with no significant differences observed between the intervention and control groups (p = 0.999). Immediately after the intervention and four weeks later, most women in the intervention groups preferred natural delivery, whereas most women in the control group continued to prefer cesarean section (p < 0.001) (Table 3).
Using an independent t-test, we compared the groups before the intervention, immediately after the intervention, and four weeks after the intervention on the self-efficacy score A (Expectations for the active stage of labor). The results indicated that the mean self-efficacy A before the intervention did not differ significantly between the two intervention groups and the control group. However, immediately after the intervention (p = 0.004) and four weeks post-intervention (p = 0.005), the mean self-efficacy score A in the two intervention groups was significantly higher compared to the control group.
Repeated measures analysis of variance was used to compare the mean self-efficacy A score before the intervention, immediately after, and four weeks post-intervention between the two intervention groups and the control group. To examine the assumption of homogeneity of the variance-covariance matrix, the M-Box test was performed, and the assumption was met (p = 0.05). The average scores of the two dimensions, self-efficacy A and self-efficacy B, did not differ significantly among the three groups before the intervention. The results indicated that time significantly influenced the self-efficacy A score (p = 0.009), and the intervention also had a significant effect on the self-efficacy score A (p = 0.017). Overall, the results showed that the mean self-efficacy A score increased from 142.97 to 162.07 (An increase of 19.10 points) in the intervention groups, while in the control group, it increased from 144.17 to 146.37 (An increase of 2.20 points) (Table 4).
Using an independent t-test, the intergroup comparison of the self-efficacy B (Expectations for the fourth stage of labor) before the intervention, immediately after the intervention, and four weeks after the intervention was examined in the two intervention groups compared to the control. The mean self-efficacy B score before the intervention in the two intervention groups compared to the control was not significantly different. However, the mean self-efficacy B score immediately after the intervention (p = 0.001) and four weeks after the intervention (p = 0.001) was significantly greater in the two intervention groups compared to the control. To compare the mean score of the self-efficacy variable B before, immediately, and four weeks after delivery in the two intervention groups compared to the control, the repeated measures analysis of variance test was used. To examine the assumption of homogeneity of the variance-covariance matrix, the M-Box test was performed, and the assumption was met (p = 0.05). The assumption of multiple correlations of the dependent variables was confirmed with the Mauchly’s sphericity test. The significance level was 0.05. The results indicated that time and the intervention were influential factors in the self-efficacy B score (p = 0.001). Overall, the results showed that the mean self-efficacy score B increased from 118.48 to 152.46 (An increase of 33.98 points) in the intervention groups, while in the control group, it increased from 118.21 to 121.23 (An increase of 3.02 points) (Table 5).
There was no significant difference in the mean mindfulness score between the two intervention groups and the control group before the intervention. However, the mean mindfulness score immediately after the intervention (p = 0.001) and four weeks after the intervention (p = 0.001) was significantly higher in the two intervention groups compared to the control, showing a substantial increase in mindfulness scores in the intervention groups. The repeated measures analysis of variance test was used to compare the mean mindfulness scores before the intervention, immediately after the intervention, and four weeks after the intervention between the two intervention groups and the control group. To examine the assumption of homogeneity of the variance-covariance matrix, the M-box test was used, which was met (p = 0.05). A significance level of 0.05 was obtained, thus confirming the assumption of sphericity. The results indicated that time was an influential factor in the mindfulness score (p = 0.001) and that the intervention was an influential factor in the mindfulness score (p = 0.017). Overall, the results showed that the average mindfulness score in the intervention group increased from 127.20 to 161.34 (an increase of 14.34 points). However, in the control group, the average mindfulness score increased from 123.80 to 124.67 (An increase of 0.87 points). These results indicate the effectiveness of the intervention among the participants (Table 6).
The description of the variables was reported in terms of frequency, percentage, mean, and standard deviation. The assumption of normality was tested using the Shapiro-Wilk test, and the results indicated a normal distribution. Based on this, parametric tests were applied. An independent t-test was used to compare the means of quantitative variables between the two groups, while the chi-square test (Fisher’s exact test) was employed to compare the frequencies of qualitative variables. To compare the mean scores of response variables over time, the repeated measures ANOVA test was utilized. To examine the effectiveness of the intervention, a repeated measures test was performed with the effect size reported. Data analysis was conducted using SPSS version 26 software, and a significance level of less than 0.05 was considered statistically significant.
Results
The results indicated that the distribution of variables such as age, gestational age, duration of marriage, education, employment status, type of residence, satisfaction with socioeconomic status, and participation in childbirth preparation classes were similar between the two intervention and control groups (Table 2).
The study results indicated that the preferred method of delivery before the intervention was similar across the three groups. Most women in all groups preferred cesarean section, with no significant differences observed between the intervention and control groups (p = 0.999). Immediately after the intervention and four weeks later, most women in the intervention groups preferred natural delivery, whereas most women in the control group continued to prefer cesarean section (p < 0.001) (Table 3).
Using an independent t-test, we compared the groups before the intervention, immediately after the intervention, and four weeks after the intervention on the self-efficacy score A (Expectations for the active stage of labor). The results indicated that the mean self-efficacy A before the intervention did not differ significantly between the two intervention groups and the control group. However, immediately after the intervention (p = 0.004) and four weeks post-intervention (p = 0.005), the mean self-efficacy score A in the two intervention groups was significantly higher compared to the control group.
Repeated measures analysis of variance was used to compare the mean self-efficacy A score before the intervention, immediately after, and four weeks post-intervention between the two intervention groups and the control group. To examine the assumption of homogeneity of the variance-covariance matrix, the M-Box test was performed, and the assumption was met (p = 0.05). The average scores of the two dimensions, self-efficacy A and self-efficacy B, did not differ significantly among the three groups before the intervention. The results indicated that time significantly influenced the self-efficacy A score (p = 0.009), and the intervention also had a significant effect on the self-efficacy score A (p = 0.017). Overall, the results showed that the mean self-efficacy A score increased from 142.97 to 162.07 (An increase of 19.10 points) in the intervention groups, while in the control group, it increased from 144.17 to 146.37 (An increase of 2.20 points) (Table 4).
Using an independent t-test, the intergroup comparison of the self-efficacy B (Expectations for the fourth stage of labor) before the intervention, immediately after the intervention, and four weeks after the intervention was examined in the two intervention groups compared to the control. The mean self-efficacy B score before the intervention in the two intervention groups compared to the control was not significantly different. However, the mean self-efficacy B score immediately after the intervention (p = 0.001) and four weeks after the intervention (p = 0.001) was significantly greater in the two intervention groups compared to the control. To compare the mean score of the self-efficacy variable B before, immediately, and four weeks after delivery in the two intervention groups compared to the control, the repeated measures analysis of variance test was used. To examine the assumption of homogeneity of the variance-covariance matrix, the M-Box test was performed, and the assumption was met (p = 0.05). The assumption of multiple correlations of the dependent variables was confirmed with the Mauchly’s sphericity test. The significance level was 0.05. The results indicated that time and the intervention were influential factors in the self-efficacy B score (p = 0.001). Overall, the results showed that the mean self-efficacy score B increased from 118.48 to 152.46 (An increase of 33.98 points) in the intervention groups, while in the control group, it increased from 118.21 to 121.23 (An increase of 3.02 points) (Table 5).
There was no significant difference in the mean mindfulness score between the two intervention groups and the control group before the intervention. However, the mean mindfulness score immediately after the intervention (p = 0.001) and four weeks after the intervention (p = 0.001) was significantly higher in the two intervention groups compared to the control, showing a substantial increase in mindfulness scores in the intervention groups. The repeated measures analysis of variance test was used to compare the mean mindfulness scores before the intervention, immediately after the intervention, and four weeks after the intervention between the two intervention groups and the control group. To examine the assumption of homogeneity of the variance-covariance matrix, the M-box test was used, which was met (p = 0.05). A significance level of 0.05 was obtained, thus confirming the assumption of sphericity. The results indicated that time was an influential factor in the mindfulness score (p = 0.001) and that the intervention was an influential factor in the mindfulness score (p = 0.017). Overall, the results showed that the average mindfulness score in the intervention group increased from 127.20 to 161.34 (an increase of 14.34 points). However, in the control group, the average mindfulness score increased from 123.80 to 124.67 (An increase of 0.87 points). These results indicate the effectiveness of the intervention among the participants (Table 6).
|
Table 2. Demographic characteristics of pregnant women across the two intervention groups and the control group
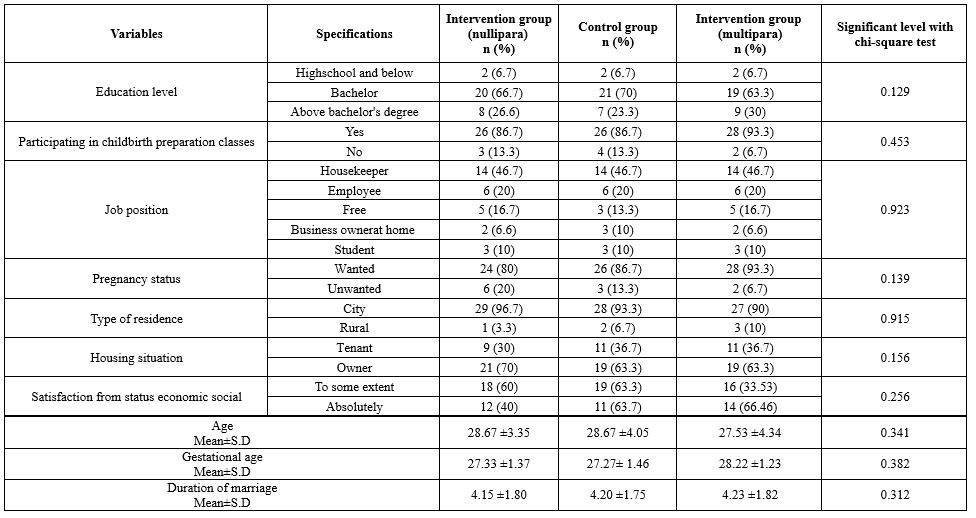 Table 3. Frequency distribution of preferred method of delivery among pregnant women 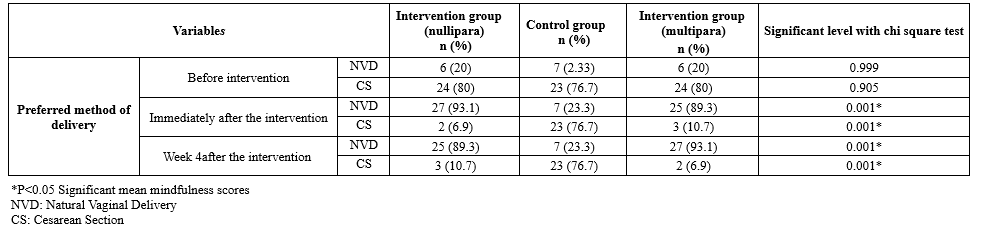 Table 4. Comparison of mean self-efficacy score (a) or the active stage of labor overtime in the intervention and control groups 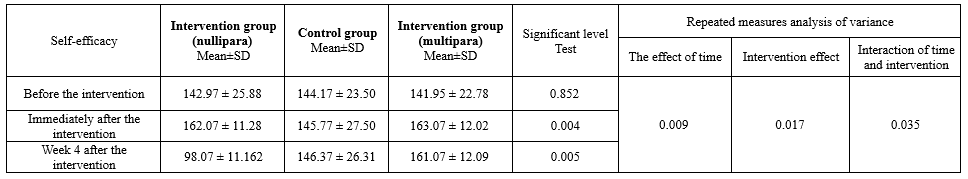 Table 5. Comparison of mean self-efficacy score (b) for the fourth stage of labor overtime in the intervention and control groups 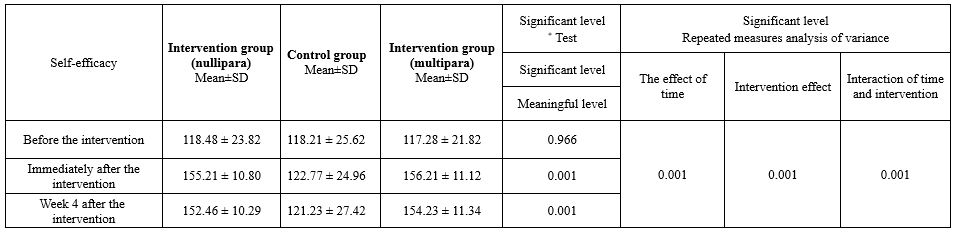 |
Table 6. Comparison of mean mindfulness scores over time in the intervention and control groups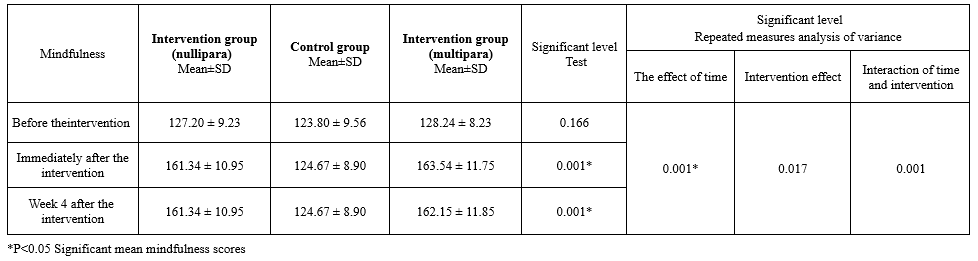 |
Discussion
This study was conducted with the purpose of determining the effect of mindfulness-based art therapy on the self-efficacy of multiparous and nulliparous women. It was designed as an experimental study with a control group. The data analysis revealed no significant differences in background variables among the three groups. The results of the present study showed that mindfulness-based art therapy during pregnancy can increase the self-efficacy of women in both intervention groups. Our results are consistent with the findings of related studies.
Relevant studies indicated that the self-efficacy of pregnant women, including their choices regarding delivery type, adaptation to labor, and postpartum care, can be improved through educational programs such as childbirth preparation classes. Several studies have demonstrated the effectiveness of psychological interventions, such as education and counseling, in building and strengthening self-efficacy. These studies suggest that psychological counseling aimed at educating and increasing the awareness of pregnant women can empower them (12-14). Psychological interventions aimed at enhancing the self-efficacy of pregnant women can help reduce the fear of childbirth, particularly in first-time mothers. The use of an educational intervention based on self-efficacy theory had positive effects on the awareness of self-care and the behaviors of the participants. Moreover, self-efficacy-based training led to an increase in health-promoting behaviors, especially physical activity and motivational skills (Self-control and sense of self-efficacy) (15,16). Implementing an awareness-raising intervention can effectively improve pregnant women’s understanding of the benefits and safety of physical activity during pregnancy, while also enhancing their self-efficacy to engage in physical activity (17).
Nezamian et al. investigated the effect of cognitive-behavioral therapy on sexual function and sexual self-efficacy in pregnant women. Their study showed that cognitive-behavioral therapy-based counseling improved sexual function and sexual self-efficacy in pregnant women compared to routine prenatal care. The group that received eight consecutive weeks of counseling had higher sexual function and self-efficacy scores than the control group that received only routine prenatal care (18). An investigation into the effect of an educational intervention based on self-efficacy theory and health literacy on pregnancy outcomes showed that the intervention effectively improved maternal health literacy and self-efficacy. This, in turn, led to favorable pregnancy outcomes, including the birth of a normal-weight baby (19). Additionally, it was found that childbirth preparation classes enhance mothers’ ability to adapt to labor and delivery, with participants showing higher self-efficacy after attending the classes, which aligns with the results of the present study. However, no significant difference was observed in childbirth self-efficacy between the control and intervention groups. This could be attributed to differences in the educational content and the number of sessions (Three sessions) provided (11).
In the present study, the results of the comparison between the groups before the intervention, immediately after the intervention, and four weeks after the intervention showed no significant difference in the mindfulness score between the two intervention groups and the control group. However, the mean mindfulness score was significantly higher in both intervention groups compared to the control group immediately after the intervention and four weeks after the intervention, with a notable increase in the intervention groups. This suggests that mindfulness-based art therapy has a positive effect on increasing mindfulness in the intervention groups. In line with the present study, Venti and Rustin found that pregnant mothers who received a mindfulness-based intervention experienced a significant decrease in anxiety levels during the third trimester of pregnancy compared to the control group (28). Furthermore, mindfulness-based group therapy was found to reduce depression and anxiety both during pregnancy and postpartum (29). Given that the results of these studies align with the present study, it is important to note that an increase in mindfulness scores can be a key condition for the effectiveness of various mindfulness-based interventions on desired outcomes. As mindfulness increases, participants experience a decrease in stress, depression, anxiety, and fear of childbirth (3-5). Practicing mindfulness-based yoga during the second trimester of pregnancy leads to a decrease in perceived stress and anxiety during the third trimester (10). In a study investigating the effect of mindfulness-based counseling on anxiety during pregnancy and the physiological parameters of newborns, the results showed that mindfulness-based counseling effectively reduced anxiety during pregnancy (6).
Traditionally, the primary goal of a cesarean section was to save the lives of mothers at risk of death due to conditions such as labor arrest. However, in recent years, the indications for cesarean sections have expanded, leading to an increased rate of unnecessary procedures. This trend has placed both the mother and fetus at risk of various health conditions. While cesarean sections are necessary for 10-15% of deliveries, studies suggest that approximately 35-90% of deliveries could be performed naturally without any medical intervention (7,8). In recent years, cesarean section has become one of the most common surgeries among women (8). In the present study, the results showed that the preferred method of delivery in all study groups before the intervention was cesarean section. However, after the intervention, the majority of participants who received the mindfulness intervention preferred natural delivery. Another study indicated that higher levels of perceived stress are associated with an increased likelihood of choosing cesarean section as an elective method of delivery (30). These findings highlight the importance of implementing strategies to reduce perceived stress in pregnant women, which may help decrease the rate of choosing cesarean section as an elective method of delivery. In the present study, mindfulness-based art therapy was used to enhance preparedness and increase self-efficacy in women. As a result, women in the intervention group showed a preference for natural childbirth, reflecting the positive impact of increased self-efficacy among the participants.
Conclusion
The results of this study suggest that mindfulness-based art therapy classes for pregnant women are an effective intervention for enhancing self-efficacy and mindfulness. These improvements can play a significant role in empowering women to make informed decisions about their preferred method of delivery, leading to a preference for natural childbirth. By addressing the lack of self-efficacy, this intervention can help reduce unnecessary cesarean sections, thereby improving maternal and fetal health outcomes. The findings highlight the potential of mindfulness-based approaches in promoting better pregnancy experiences and outcomes, ultimately contributing to the reduction of complications associated with childbirth. Therefore, it is recommended that individuals with a fear of childbirth, especially primiparous women, be identified and assessed during pregnancy, as these women can benefit from receiving interventions similar to the one used in this study.
Acknowledgement
The authors thank the pregnant women who participated in the study for their support in conducting this research.
Funding sources
None.
Ethical statement
The code of ethics was obtained from Hormozgan University of Medical Sciences (IR.HUMS.REC.1403.156). Informed consent was obtained from participants before entering the study. The information of the study participants remained confidential. The principles of ethics in human research were observed. Withdrawal from the intervention sessions in this study was completely voluntary; there was no compulsion to continue the intervention sessions. Thirty-one ethical codes related to medical science studies were followed during the study.
Conflicts of interest
The authors declare that they have no competing interests.
Author contributions
All authors read and approved the final manuscript. All authors take responsibility for the integrity of the data and the accuracy of the data analysis.
Type of study: Original Article |
Subject:
Midwifery
References
1. Andaroon N, Kordi M, Ghasemi M, Mazlom R. The validity and reliability of the Wijma delivery expectancy/experience questionnaire (Version a) in primiparous women in Mashhad, Iran. Iran J Med Sci. 2020;45(2):110-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Alizadeh-Dibazari Z, Maghalain M, Mirghafourvand M. The effect of non-pharmacological prenatal interventions on fear of childbirth: an overview of systematic reviews and meta-analysis. BMC Psychiatry. 2024;24(1):415. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Sahraei F, Rahemi Z, Sadat Z, Zamani B, Mirbagher Ajorpaz N, Afshar M, et al. The Effect of Swedish Massage on Pain in Rheumatoid Arthritis Patients: A Randomized Controlled Trial. Complement Ther Clin Pract. 2022;46:101524. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Abedi F, Ajorpaz NM, Esalatmanesh S, Rahemi Z, Gilasi HR, Atrian MK, et al. The Effect of Tactile-Kinesthetic Stimulation on Growth Indices of Healthy Neonates. J Bodyw Mov Ther. 2018;22(2):308-12. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Dai J, Shi Y, Guo L, Wang Y, Kong X. Discrepancy in parental fear of childbirth: A scoping review. Midwifery. 2023;126:103830 [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Heydarpour S, Feli R, Yazdanbakhsh K, Heydarpour F. The impact of mindfulness-based counselling on the levels of anxiety during pregnancy and on newborns' physiological parameters. Scientific Journal of Nursing, Midwifery and Paramedical Faculty. 2020:6(1):106-17. [View at Publisher] [Google Scholar]
7. Leng LL, Yin XC, Ng SM. Mindfulness-based intervention for clinical and subthreshold perinatal depression and anxiety: A systematic review and meta-analysis of randomized controlled trial. Compr Psychiatry. 2023;122:152375. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Veringa-Skiba IK, Ziemer K, de Bruin EI, de Bruin EJ, Bögels SM. Mindful awareness as a mechanism of change for natural childbirth in pregnant women with high fear of childbirth: a randomised controlled trial. BMC Pregnancy Childbirth. 2022;22(1):47. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Van der Meulen RT, Veringa-Skiba IK, Van Steensel FJA, Bögels SM, De Bruin EI. Mindfulness-based childbirth and parenting for pregnant women with high fear of childbirth and their partners: outcomes of a randomized controlled trial assessing short- and longer-term effects on psychological well-being, birth and pregnancy experience. Midwifery. 2023;116:103545. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Fenwick J, Toohill J, Gamble J, Creedy DK, Buist A, Turkstra E, et al. Effects of a midwife psycho-education intervention to reduce childbirth fear on women's birth outcomes and postpartum psychological wellbeing. BMC Pregnancy Childbirth. 2015;15(1):284. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Jones KA, Freijah I, Brennan SE, McKenzie JE, Bright TM, Fiolet R, et al. Interventions from pregnancy to two years after birth for parents experiencing complex post-traumatic stress disorder and/or with childhood experience of maltreatment. Cochrane Database Syst Rev. 2023;5(5):CD014874. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Barış M, Lim X, Almonte MT, Shaw D, Brierley J, Porsdam Mann S, et al. Ethics of Procuring and Using Organs or Tissue from Infants and Newborns for Transplantation, Research, or Commercial Purposes: Protocol for a Bioethics Scoping Review. Wellcome Open Res. 2024;9:717. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. O'Connell MA, Khashan AS, Leahy-Warren P, Stewart F, O'Neill SM. Interventions for fear of childbirth including tocophobia. Cochrane Database Syst Rev. 2021;7(7):CD013321. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Gómez-Sánchez L, García-Banda G, Servera M, Verd S, Filgueira A, Cardo E. Beneficios del mindfulness en mujeres embarazadas [Benefits of mindfulness in pregnant women]. Medicina (B Aires). 2020;80(Suppl 2):47-52. [View at Publisher] [Google Scholar]
15. Webb R, Bond R, Romero-Gonzalez B, Mycroft R, Ayers S. Interventions to treat fear of childbirth in pregnancy: a systematic review and meta-analysis. Psychological Medicine. 2021;51(12):1964-77. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Abdolalipour S, Mohammad-Alizadeh Charandabi S, Mashayekh-Amiri S, Mirghafourvand M. The effectiveness of mindfulness-based interventions on self-efficacy and fear of childbirth in pregnant women: A systematic review and meta-analyses. J Affect Disord. 2023;333:257-70. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Mousavi A SE, Sadeghi R, Tol A, Rahimi Foroshani A, Mohebbi B. The effect of educational intervention on self-efficacy, knowledge of benefits and safety tips of physical activity among pregnant women. Razi J Med Sci. 2020;26(11):98-111. [View at Publisher] [Google Scholar]
18. Nezamnia M, Iravani M, Bargard MS, Latify M. Effectiveness of cognitive-behavioral therapyon sexual function and sexual self-efficacy in pregnant women: An RCT. Int J Reprod Biomed. 2020;18(8):625-36. [View at Publisher] [DOI] [Google Scholar]
19. Kharazi SS, Peyman N, Esmaily H. The effect of educational intervention based on self-efficacy theory and health literacy on pregnancy outcomes. Iran J Obstet Gynecol Infertil. 2018;21(5):33-46. [View at Publisher] [DOI] [Google Scholar]
20. Toohill J, Fenwick J, Gamble J, Creedy DK, Buist A, Turkstra E, et al. A randomized controlled trial of a psycho‐education intervention by midwives in reducing childbirth fear in pregnant women. Birth. 2014;41(4):384-94. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Shakarami, A., Mirghafourvand, M., Abdolalipour, S. et al. Comparison of fear, anxiety and self-efficacy of childbirth among primiparous and multiparous women. BMC Pregnancy Childbirth. 2021;21(1):642. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Lowe NK. Self-efficacy for labor and childbirth fears in nulliparous pregnant women.J Psychosom Obstet Gynaecol. 2000;21(4):219-24. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Khorsandi M, Asghari Jafarabadi M, Jahani F, Rafiei M. Cultural adaptation and psychometric testing of the short form of Iranian childbirth self efficacy inventory. Iran Red Crescent Med J. 2013;15(11):e11741-e. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Danielson C, Jones S. Five Facet Mindfulness Questionnaire (FFMQ). The Sourcebook of Listening Research: Methodology and Measures. 2017. p.281-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27-45. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Heydarinasab L. An investigation of the validity and reliability of psychometric characteristics of five facet mindfulness questionnaire in Iranian non-clinical samples. International Journal of Behavioral Sciences. 2013;7(3):229-37. [View at Publisher] [Google Scholar]
27. Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: results of a pilot study. Arch Womens Ment Health. 2008;11(1):67-74. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Pan WL, Chang CW, Chen SM, Gau ML. Assessing the effectiveness of mindfulness-based programs on mental health during pregnancy and early motherhood - a randomized control trial. BMC Pregnancy Childbirth. 2019;19(1):346. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Dhillon A, Sparkes E, Duarte RV. Mindfulness-Based Interventions During Pregnancy: a Systematic Review and Meta-analysis. Mindfulness. 2017;8(6):1421-37. [View at Publisher] [DOI] [PMID] [Google Scholar]
30. Nazeri S, Amini L, Sadeghi Avval Shahr H, Haghani S, Heshmati H. The Association of the Levels of Perceived Stress With the Preferred Mode of Delivery in Primiparous Women. Iran Journal of Nursing. 2022;34(134):102-15. [View at Publisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |