Volume 21, Issue 4 (12-2024)
J Res Dev Nurs Midw 2024, 21(4): 36-40 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Medina-Fernández I A, Esparza-González S C, Torres Soto N Y, Carrillo-Cervantes A L, Trujillo-Hernández P E, Medina-Fernández J A. Sarcopenia, functional capacity, and physical components of quality of life in older adults Mexicans: An explanatory model. J Res Dev Nurs Midw 2024; 21 (4) :36-40
URL: http://nmj.goums.ac.ir/article-1-1871-en.html
URL: http://nmj.goums.ac.ir/article-1-1871-en.html
Isaí Arturo Medina-Fernández1 

 , Sandra Cecilia Esparza-González1
, Sandra Cecilia Esparza-González1 

 , Nissa Yaing Torres Soto2
, Nissa Yaing Torres Soto2 

 , Ana Laura Carrillo-Cervantes1
, Ana Laura Carrillo-Cervantes1 

 , Pedro Enrique Trujillo-Hernández1
, Pedro Enrique Trujillo-Hernández1 

 , Josué Arturo Medina-Fernández3
, Josué Arturo Medina-Fernández3 




 , Sandra Cecilia Esparza-González1
, Sandra Cecilia Esparza-González1 

 , Nissa Yaing Torres Soto2
, Nissa Yaing Torres Soto2 

 , Ana Laura Carrillo-Cervantes1
, Ana Laura Carrillo-Cervantes1 

 , Pedro Enrique Trujillo-Hernández1
, Pedro Enrique Trujillo-Hernández1 

 , Josué Arturo Medina-Fernández3
, Josué Arturo Medina-Fernández3 


1- Universidad Autónoma de Coahuila, México
2- Universidad Autónoma Del Estado De Quintana Roo, México
3- Universidad Autónoma Del Estado De Quintana Roo, México ,josue.medina@uqroo.edu.mx
2- Universidad Autónoma Del Estado De Quintana Roo, México
3- Universidad Autónoma Del Estado De Quintana Roo, México ,
Full-Text [PDF 542 kb]
(154 Downloads)
| Abstract (HTML) (528 Views)
Discussion
The objective of this study was to determine the influence of sarcopenia risk on the physical components of QoL and functional capacity in older adults. The results serve as a key reference for nursing professionals to identify risks that impact the health status of this vulnerable group.
In this study, the risk of sarcopenia was present at 44.8%, being higher than the results reported by Carrillo-Vega et al. (2022) at 31%, Meng et al. (2024) at 20.7%, and Veronose et al. (2024), who identified a prevalence of 25.72%. These findings highlight sarcopenia as an emerging area of geriatrics, particularly relevant in addressing functional impairment and dependency, which affect a significant portion of the aging population (22-25). The current investigation revealed that BMI is at the overweight level, which is higher compared to the studies conducted by Aiken et al. (2024) and Fantin et al. (2024) who found levels of overweight in their sample. In Mexico, obesity is considered a major public health issue due to its association with an increased risk of chronic diseases, which in turn raises the likelihood of developing sarcopenia (26,27). In this study, the participants had a normal calf circumference, with results lower than those reported by Kusaka et al. (2017) but slightly higher than those of Kim et al. (2018). This variation is likely due to the established link between calf circumference and sarcopenia (28,29).
Gait speed in this study was found to be above the normal threshold. The result presented above is lower than that presented by Álvares-Bustos et al. (2024); however, it was higher than the result found in the study conducted by Fantin et al. (2017). The foregoing is due to the modification of the body composition of the elderly; it impacts usual walking speed due to the decrease in strength in the lower extremities (27,30,31). Considering the grip strength, a low force was found in this sample, which is lower than that cited by Hua et al. (2016), as well as much lower than what was found in the study carried out by Iwatmoto et al. (2017) (32,33). Mean below normal parameters indicate changes in skeletal muscle mass cause changes in upper extremity muscle tissue (34). Correspondingly, the grip strength in Mexico was lower compared to studies from other countries.
Regarding appendicular skeletal muscle mass, the mean was 15.05 kg. Compared to other studies, this value was lower. For instance, in the study by Sun et al. (2024), the average muscle mass in older adults was 21.98 kg, while Moon et al. (2018) reported an average of 19.5 kg for men and 12.9 kg for women. This decline in muscle mass may be associated with structural and functional changes in muscle tissue (35,36). However, the BADL indicated a mean of 95.03 points. These results were lower than what was reported by Carrillo-Vega et al. (2024) with a mean of 99.36 points. Moreover, they were higher than those obtained by Moon et al. (2018) with a mean of 40.6 (23,36). In older adults, there are various factors such as the presence of decreased muscle mass and fist strength. This leads to difficulty in performing BADL; thereby increasing the risk of dependency (37).
In terms of instrumental activities of daily living (IADL), the average score in this sample was 7.09 points, which was lower than the results reported by Castillo (2017) and Jun et al. (2022) (38,39). The explanation of BADL and AIVD indicates that the presence of sarcopenia translates into a decrease in functional capacity that leads to the risk of various geriatric syndromes, such as the risk of frailty and an increase in disability (40). On the other hand, the physical components of the health-related QoL reflected an average of 31.33 for physical function and 29.88 for physical role; however, they are lower than what was reported by Silva et al. (2016), with a mean of 65 for the physical function and 65.46 for the physical role. Sánchez-García et al. (2017) reported a mean of 74.4 for the physical function and 65.1 for the physical role (41,42). Overall, the study found that as the signs of sarcopenia increased, physical function and physical role decreased. These results are similar to what was reported by Manrique-Espinoza et al. (2017) and Silva et al. (2016) (42,43). This explains the physical impact of muscle loss and its symptoms on the difficulty of performing physical activities that interfere with life.
The sarcopenia model influences the physical components of QoL and functional capacity by 51.1%. These results are consistent with other studies (44) which found that patients with sarcopenia experienced a decline in QoL within the physical domain and an increase in physical dependence. This occurs because the signs of sarcopenia lead to limitations in performing both daily living and instrumental activities, which are essential for maintaining a good perception of QoL. These limitations modify habits, daily activities, and leisure (8).
These findings have significant implications for nursing practice, highlighting the importance of early detection of factors affecting older adults, such as sarcopenia. Therefore, future interventions are necessary to promote activities that enhance muscle strength, muscle mass, and physical performance, ultimately preventing deterioration in QoL components and functional capacity. Although the relatively small sample size was sufficient to validate the statistical models, it may limit the generalizability of the findings. Additionally, one of the study’s limitations is the inability to generalize its results. Furthermore, economic status and depression were not considered confounding variables, which may have influenced the outcomes. It is suggested to increase the sample size and conduct the study in other areas of Mexico. Likewise, it is suggested to detect muscle mass with the dual-energy X-ray absorptiometry (DXA) as the gold standard, and apply the SPPB assessment instrument to assess physical performance.
Conclusion
Sarcopenia negatively affects approximately half of the physical components of QoL and functional capacity, making it a predictive factor. These findings will serve as a foundation for future research on sarcopenia in the state of Coahuila, Mexico, and will support nursing interventions focused on its prevention, aiming to reduce its impact on the QoL and functional capacity of the elderly. Future research can explore effective interventions to prevent or delay sarcopenia in older Mexican adults, including exercise programs, personalized nutrition, and pharmacological therapies. It may be valuable to assess the influence of psychosocial factors, such as social support and mental health, on physical and functional QoL. Additionally, longitudinal studies can examine how changes in sarcopenia affect functionality and QoL in the long term.
Acknowledgement
The authors thank the participants of this research.
Funding sources
Not applicable.
Ethical statement
This study adhered to the provisions of the General Health Law on Research for Health, specifically the second title concerning the ethical aspects of research involving human subjects. Additionally, it complied with the Official Mexican Standard NOM-012-SSA3-2012, which establishes the criteria for conducting health research on human participants. Written informed consent was obtained from all participants. This research was approved by the Ethics Committee of the Faculty of Nursing at the Autonomous University of Coahuila, under registration number (Missing number).
Conflicts of interest
The authors declare no conflict of interest.
Author contributions
IAMF and SCES conceptualized and designed the study. ALCC contributed to data collection and preliminary analysis. NYTS performed statistical analyses and contributed to the interpretation of results. PETH provided critical insights and supervised the research methodology. IAMF and JAMF supervised the study, and drafted and revised the manuscript. All authors read and approved the final version of the manuscript.
Full-Text: (102 Views)
Introduction
In Mexico, statistics indicate that there are 12.4 million people over 60 years of age, which represents 10.4% of the country's total population (1). This accelerated increase in the elderly population in Mexico makes its management more complex, so it is a priority to identify needs and risks; thus, providing care with humane and comprehensive quality (2). However, aging is a progressive, intrinsic, and universal process that over time occurs in all living beings as a result of the interaction of the individual's genetics and their environment, leading to functional losses (3). A physical change associated with functional loss is sarcopenia. This is defined as a muscle disease that can be acute or chronic, characterized by decreased muscle strength, low muscle mass and/or lower physical performance, which is related to increased morbidity and mortality (4).
This condition leads to a decrease in muscle mass due to a reduction in both the size and number of type II muscle fibers. As a result, individuals exhibit lower concentrations of myoglobin, capillaries, and mitochondria while possessing a high glycolytic capacity. Likewise, it presents an infiltration by fat and connective tissue and a decrease in the capillary/fiber ratio that alters the supply of nutrients from the bloodstream to the muscle fiber (5). On the other hand, the prevalence of sarcopenia increases with age, both in men and women, regardless of ethnicity; however, it is considered to be typical of the elderly. It is known that the decrease in muscle mass begins between the ages of 20 and 30, with a loss of about 20% at age 50, and various studies indicate that 50% of people over 80 suffer from sarcopenia (6).
In this regard, sarcopenia continues to be an important clinical problem that impacts millions of older adults (7). One of the significant impacts is on the quality of life (QoL), affecting an individual's ability to cope with this condition. Studying it from the perspective of physical function and physical role within the QoL components in the elderly highlights their ability to adapt to ongoing functional changes. The signs of sarcopenia contribute to limitations in performing daily living activities or instrumental tasks, providing valuable insights into certain diseases and the overall health status of patients. Therefore, its analysis plays a crucial role in clinical decision-making (8,9).
Another key effect is on functional capacity, which is assessed by evaluating daily living activities to monitor changes over time. It is also the most reliable indicator for determining the health status of an older adult, as it encompasses biological, psychological, and social interactions. Functional capacity is the most accurate reflection of an individual’s overall integrity during aging (3). The importance of studying this variable starts from assessing the physical impact that affects activities of daily living or instrumental activities, which can be modified by the decrease in strength, muscle mass, and physical performance.
For this reason, nursing professionals must focus on promoting successful aging through a comprehensive approach. In addition to addressing health aspects, factors such as personal well-being, functionality, and environmental influences on pathology should be considered. This approach facilitates continued personal development (10). Furthermore, the assessment of sarcopenia is essential for identifying risks, allowing for the implementation of preventive measures to avoid further deterioration. Therefore, it should be incorporated into routine clinical practice and serve as a fundamental pillar of nursing care. Conducting studies in this area is vital, as the findings will support the development of evidence-based proposals and intervention strategies for elderly adaptation.
Therefore, the objective of the study was to determine the modeling of the effect of sarcopenia on the functional capacity and the physical components of the QoL related to health in older adults from Saltillo, Coahuila, Mexico.
Methods
Design and study sample
The design of this research is predictive correlational design because of the prediction of the causal relationships between the variables (11). The study population was 500 older adults who attended the six clubs for older adults in Saltillo, Mexico. The sample of 144 older adults was determined with G*power 3.11 software, by simple sampling with a confidence level of 95%, margin of error of 5% and proportion of 15% (12). Adults 60 years of age or older were included, without cognitive impairment determined with the Pfeiffer instrument, and without neurological, motor, or neuromuscular deficits diagnosed by a physician prior to the study.
Measurements
Sociodemographic and clinical data
This questionnaire was prepared by the author and has questions that allowed characterizing the population with data such as sex, age, educational level, and anthropometric characteristics such as weight, height, body mass index (BMI), muscle mass, fat mass, waist circumference, calf circumference, and grip strength.
Sarcopenia
To measure the sarcopenia variable, the Simple Questionnaire to Rapidly Diagnose Sarcopenia (SARC-F scale) elaborated by Parra et al. was applied. It was validated in the older adult population of Mexico City with a Cronbach's alpha of 0.64, which was made up of five items that rate their intensity differently (Strength, assistance to walk, ability to get up from a chair, ability to climb stairs, falls). The score ranges from 0 to 10 points, indicating that greater than 4 points there is presence of Sarcopenia and less than 4 points indicates normal results (13,14).
Physical components of QoL
The physical function and physical role subscales of the SF-36 were used to measure the physical component, validated by Sánchez et al. in adults and older adults in the northern region of Mexico with Cronbach's Alpha of 0.94. The response format follows a Likert scale, ranging from "nothing" to "a lot," with scores from 1 to 5. According to the scale, lower scores indicate better health-related quality of life (HRQoL) in the physical components. However, for the purposes of this research, the measurement was inverted-higher scores indicate better physical components of HRQoL (15).
It was determined through the basic and instrumental activities of daily life. The functionality index was used to perform the BADL validated by Cabañero-Martínez et al (2009), which assesses the autonomy that the person has to perform basic activities in a dependent or independent manner. Your score ranges from 0 (Completely dependent) to 100 points (Completely independent). It contains 10 questions with answers of two to four options per question, the cut-off points are <20 = total dependency, 20-40 = severe dependency, 45-55 = moderate dependency, and >60 = mild dependency, the score is by intervals five points; Cronbach's alpha is 0.86. For this study, it will be determined that the higher the score, the greater the independence (16).
The instrumental activities of daily living (IADL) were assessed using the Lawton-Brody scale, Spanish version. It was used to evaluate the functional capacity to carry out instrumental activities through eight items with values of 1 = independent and 0 = dependent. The score goes from 0 to 8, the cut-off points are 0-1: total dependence, 2-3: severe dependence, 4-5: moderate dependence, 6-7: light dependence and 8 autonomous, whose Cronbach's alpha coefficient was 0.94 (17-19).
Body composition
Muscle mass was determined based on the European Consent and whose appendicular skeletal muscle mass formula (MMEA) kg = 0.215 × calf circumference (cm) + 0.093 × hand grip strength (kg) + 0.061 × weight (kg). + 3.637 × sex + 0.112 × height (cm) - 16.449; where sex: male =1; female =0 (20).
Muscle strength was performed with digital dynamometer, which procedure is observed in Appendix H; however, the EWGSOP (European Working Group on Sarcopenia in the Elderly) establishes the following cut-off points to detect risk of sarcopenia: women (<20 kg of grip strength) and men (<30 kg of grip strength) (21).
Gait speed was measured based on the subsection of the Short Physical Performance Battery (SPPB) scale, validated by Cruz et al. (Cronbach's Alpha) 0.76. It is determined through the formula: distance (m)/time (s). For the sample, participants walked six meters, with four meters considered for measurement. If the walking speed was greater than or equal to 0.8 m/s, the probability of sarcopenia increased (21).
On the other hand, the height was measured with a stadiometer and weight with an impedance scale. The BMI was determined using the Quetelet formula (weight/height2). BMI classifications were as follows: underweight (<22 kg/m²), normal weight (22-27 kg/m²), overweight (27.1-30 kg/m²), and obesity (>30 kg/m²). Calf circumference was measured using a flexible tape, with a value above 31 cm indicating a normal parameter (5).
In the first instance, six centers for the elderly were invited to participate in the study. Once the adults who met the inclusion criteria were identified (Adults 60 years of age or older were included, without cognitive impairment determined with the Pfeiffer instrument, without neurological, motor, or neuromuscular deficits diagnosed by a physician prior to the study), an appointment was scheduled for their lives. Before data collection, informed consent was obtained. Once participants gave their approval, the cognitive impairment assessment process began. If a maximum of two errors were recorded on the Pfeiffer instrument, the sociodemographic data form was administered. This was followed by the assessment of weight, height, BMI, grip strength, calf circumference, and gait speed, all of which were documented in the clinical characteristics section of the data form. However, once the body composition was completed, the SARC-F instrument, physical function, physical role subscales, and the BADL and, finally, the Lawton-Brody scale, were applied.
Statistical analysis
The information processing of the quantitative data was carried out in the Statistic Package for the Social Science (SPSS) software version 20. For statistical analysis, frequencies and percentages were used for categorical and ordinal variables, while means, medians, and standard deviations were used for continuous variables. The normality of continuous variables was assessed using the Kolmogorov-Smirnov test. Since the data followed a non-normal distribution (p<0.05), non-parametric tests were applied.
Differences in mean age, body composition, functional capacity, and physical components of QoL between older adults with and without risk of sarcopenia were analyzed using the Mann-Whitney U test. The Spearman test was used for variable correlations, while simple linear regressions determined the influence of functional capacity and physical components of QoL on the risk of sarcopenia.
A structural equation model was tested using EQS software version 6.1. The chi-square test was used as the statistical indicator. If the significance level was p > 0.05, the model was considered to have an adequate statistical fit. Since chi-square (χ²) is sensitive to sample size, the relative χ² was calculated by dividing the adjusted χ² index by the degrees of freedom. A relative χ² value of <5 was considered indicative of a good statistical fit. Additionally, statistical goodness-of-fit indicators suggested an acceptable model fit (χ² = 88.287, df = 77, p = 0.001, relative χ² = 1.14; BBNFI = 0.91; BBNNFI = 0.96; CFI = 0.96; RMSEA = 0.06). These values indicate that the theoretical model is well supported by the data.
Results
The sample consisted of 144 older adults, with ages ranging from 60 to 92 years, with a mean of 71.90 years (SD = 7.73 years). Table 1 shows the frequencies of the sociodemographic variables, with the majority being women, having a primary education level, and being widows. The clinical characteristics of the sample are as follows: 26.4% had type 2 diabetes mellitus (T2DM), diagnosed between 1 and 39 years of age, and a mean age of 13.84 ± 9.99 years. Additionally, 60.4% of the sample had arterial hypertension, with the duration of the condition ranging from 1 to 53 years, and a mean age of 15.66 ± 11.94 years. Regarding nutritional status, 4.9% were underweight, 33.3% had a normal weight, 33.3% were overweight, and 28.5% were obese. Furthermore, 25% were below the limit of the musculoskeletal index, 62.5% had low strength, and 65.3% had a speed above 0.8 m/s.
The results indicated that the prevalence of identified sarcopenia was 44.8%. The sarcopenia was higher in women with 45.2%, being more frequent in elderly widows with 55.9%. Regarding the presence of sarcopenia in people with chronic conditions, it was found in 52.9% of older adults with arterial hypertension, as well as in 47.4% of adults with T2DM and 43.9% in people with obesity. The functional capacity indicated that 32.6% had some degree of dependence on basic activities of daily living and 37.5% had some degree of dependence on instrumental activities of life. In terms of physical function within the physical components of QoL, the activities that most significantly limit older adults include bending over or kneeling (19.4%) and climbing multiple flights of stairs (15.3%). Conversely, the activities with the highest percentages of non-limitation were bathing or dressing (65.4%) and making a moderate effort to push (39.6%). Regarding the physical role of the physical components, 8.3% indicated that physical health had made their social and/or family activities very difficult. Moreover, it had made their usual work very difficult. On the other hand, a higher percentage, 41% indicated that the pain had not prevented them from doing their usual work at all and 38.9% indicated that their physical health had not caused them to completely stop their daily activities.
In Mexico, statistics indicate that there are 12.4 million people over 60 years of age, which represents 10.4% of the country's total population (1). This accelerated increase in the elderly population in Mexico makes its management more complex, so it is a priority to identify needs and risks; thus, providing care with humane and comprehensive quality (2). However, aging is a progressive, intrinsic, and universal process that over time occurs in all living beings as a result of the interaction of the individual's genetics and their environment, leading to functional losses (3). A physical change associated with functional loss is sarcopenia. This is defined as a muscle disease that can be acute or chronic, characterized by decreased muscle strength, low muscle mass and/or lower physical performance, which is related to increased morbidity and mortality (4).
This condition leads to a decrease in muscle mass due to a reduction in both the size and number of type II muscle fibers. As a result, individuals exhibit lower concentrations of myoglobin, capillaries, and mitochondria while possessing a high glycolytic capacity. Likewise, it presents an infiltration by fat and connective tissue and a decrease in the capillary/fiber ratio that alters the supply of nutrients from the bloodstream to the muscle fiber (5). On the other hand, the prevalence of sarcopenia increases with age, both in men and women, regardless of ethnicity; however, it is considered to be typical of the elderly. It is known that the decrease in muscle mass begins between the ages of 20 and 30, with a loss of about 20% at age 50, and various studies indicate that 50% of people over 80 suffer from sarcopenia (6).
In this regard, sarcopenia continues to be an important clinical problem that impacts millions of older adults (7). One of the significant impacts is on the quality of life (QoL), affecting an individual's ability to cope with this condition. Studying it from the perspective of physical function and physical role within the QoL components in the elderly highlights their ability to adapt to ongoing functional changes. The signs of sarcopenia contribute to limitations in performing daily living activities or instrumental tasks, providing valuable insights into certain diseases and the overall health status of patients. Therefore, its analysis plays a crucial role in clinical decision-making (8,9).
Another key effect is on functional capacity, which is assessed by evaluating daily living activities to monitor changes over time. It is also the most reliable indicator for determining the health status of an older adult, as it encompasses biological, psychological, and social interactions. Functional capacity is the most accurate reflection of an individual’s overall integrity during aging (3). The importance of studying this variable starts from assessing the physical impact that affects activities of daily living or instrumental activities, which can be modified by the decrease in strength, muscle mass, and physical performance.
For this reason, nursing professionals must focus on promoting successful aging through a comprehensive approach. In addition to addressing health aspects, factors such as personal well-being, functionality, and environmental influences on pathology should be considered. This approach facilitates continued personal development (10). Furthermore, the assessment of sarcopenia is essential for identifying risks, allowing for the implementation of preventive measures to avoid further deterioration. Therefore, it should be incorporated into routine clinical practice and serve as a fundamental pillar of nursing care. Conducting studies in this area is vital, as the findings will support the development of evidence-based proposals and intervention strategies for elderly adaptation.
Therefore, the objective of the study was to determine the modeling of the effect of sarcopenia on the functional capacity and the physical components of the QoL related to health in older adults from Saltillo, Coahuila, Mexico.
Methods
Design and study sample
The design of this research is predictive correlational design because of the prediction of the causal relationships between the variables (11). The study population was 500 older adults who attended the six clubs for older adults in Saltillo, Mexico. The sample of 144 older adults was determined with G*power 3.11 software, by simple sampling with a confidence level of 95%, margin of error of 5% and proportion of 15% (12). Adults 60 years of age or older were included, without cognitive impairment determined with the Pfeiffer instrument, and without neurological, motor, or neuromuscular deficits diagnosed by a physician prior to the study.
Measurements
Sociodemographic and clinical data
This questionnaire was prepared by the author and has questions that allowed characterizing the population with data such as sex, age, educational level, and anthropometric characteristics such as weight, height, body mass index (BMI), muscle mass, fat mass, waist circumference, calf circumference, and grip strength.
Sarcopenia
To measure the sarcopenia variable, the Simple Questionnaire to Rapidly Diagnose Sarcopenia (SARC-F scale) elaborated by Parra et al. was applied. It was validated in the older adult population of Mexico City with a Cronbach's alpha of 0.64, which was made up of five items that rate their intensity differently (Strength, assistance to walk, ability to get up from a chair, ability to climb stairs, falls). The score ranges from 0 to 10 points, indicating that greater than 4 points there is presence of Sarcopenia and less than 4 points indicates normal results (13,14).
Physical components of QoL
The physical function and physical role subscales of the SF-36 were used to measure the physical component, validated by Sánchez et al. in adults and older adults in the northern region of Mexico with Cronbach's Alpha of 0.94. The response format follows a Likert scale, ranging from "nothing" to "a lot," with scores from 1 to 5. According to the scale, lower scores indicate better health-related quality of life (HRQoL) in the physical components. However, for the purposes of this research, the measurement was inverted-higher scores indicate better physical components of HRQoL (15).
It was determined through the basic and instrumental activities of daily life. The functionality index was used to perform the BADL validated by Cabañero-Martínez et al (2009), which assesses the autonomy that the person has to perform basic activities in a dependent or independent manner. Your score ranges from 0 (Completely dependent) to 100 points (Completely independent). It contains 10 questions with answers of two to four options per question, the cut-off points are <20 = total dependency, 20-40 = severe dependency, 45-55 = moderate dependency, and >60 = mild dependency, the score is by intervals five points; Cronbach's alpha is 0.86. For this study, it will be determined that the higher the score, the greater the independence (16).
The instrumental activities of daily living (IADL) were assessed using the Lawton-Brody scale, Spanish version. It was used to evaluate the functional capacity to carry out instrumental activities through eight items with values of 1 = independent and 0 = dependent. The score goes from 0 to 8, the cut-off points are 0-1: total dependence, 2-3: severe dependence, 4-5: moderate dependence, 6-7: light dependence and 8 autonomous, whose Cronbach's alpha coefficient was 0.94 (17-19).
Body composition
Muscle mass was determined based on the European Consent and whose appendicular skeletal muscle mass formula (MMEA) kg = 0.215 × calf circumference (cm) + 0.093 × hand grip strength (kg) + 0.061 × weight (kg). + 3.637 × sex + 0.112 × height (cm) - 16.449; where sex: male =1; female =0 (20).
Muscle strength was performed with digital dynamometer, which procedure is observed in Appendix H; however, the EWGSOP (European Working Group on Sarcopenia in the Elderly) establishes the following cut-off points to detect risk of sarcopenia: women (<20 kg of grip strength) and men (<30 kg of grip strength) (21).
Gait speed was measured based on the subsection of the Short Physical Performance Battery (SPPB) scale, validated by Cruz et al. (Cronbach's Alpha) 0.76. It is determined through the formula: distance (m)/time (s). For the sample, participants walked six meters, with four meters considered for measurement. If the walking speed was greater than or equal to 0.8 m/s, the probability of sarcopenia increased (21).
On the other hand, the height was measured with a stadiometer and weight with an impedance scale. The BMI was determined using the Quetelet formula (weight/height2). BMI classifications were as follows: underweight (<22 kg/m²), normal weight (22-27 kg/m²), overweight (27.1-30 kg/m²), and obesity (>30 kg/m²). Calf circumference was measured using a flexible tape, with a value above 31 cm indicating a normal parameter (5).
In the first instance, six centers for the elderly were invited to participate in the study. Once the adults who met the inclusion criteria were identified (Adults 60 years of age or older were included, without cognitive impairment determined with the Pfeiffer instrument, without neurological, motor, or neuromuscular deficits diagnosed by a physician prior to the study), an appointment was scheduled for their lives. Before data collection, informed consent was obtained. Once participants gave their approval, the cognitive impairment assessment process began. If a maximum of two errors were recorded on the Pfeiffer instrument, the sociodemographic data form was administered. This was followed by the assessment of weight, height, BMI, grip strength, calf circumference, and gait speed, all of which were documented in the clinical characteristics section of the data form. However, once the body composition was completed, the SARC-F instrument, physical function, physical role subscales, and the BADL and, finally, the Lawton-Brody scale, were applied.
Statistical analysis
The information processing of the quantitative data was carried out in the Statistic Package for the Social Science (SPSS) software version 20. For statistical analysis, frequencies and percentages were used for categorical and ordinal variables, while means, medians, and standard deviations were used for continuous variables. The normality of continuous variables was assessed using the Kolmogorov-Smirnov test. Since the data followed a non-normal distribution (p<0.05), non-parametric tests were applied.
Differences in mean age, body composition, functional capacity, and physical components of QoL between older adults with and without risk of sarcopenia were analyzed using the Mann-Whitney U test. The Spearman test was used for variable correlations, while simple linear regressions determined the influence of functional capacity and physical components of QoL on the risk of sarcopenia.
A structural equation model was tested using EQS software version 6.1. The chi-square test was used as the statistical indicator. If the significance level was p > 0.05, the model was considered to have an adequate statistical fit. Since chi-square (χ²) is sensitive to sample size, the relative χ² was calculated by dividing the adjusted χ² index by the degrees of freedom. A relative χ² value of <5 was considered indicative of a good statistical fit. Additionally, statistical goodness-of-fit indicators suggested an acceptable model fit (χ² = 88.287, df = 77, p = 0.001, relative χ² = 1.14; BBNFI = 0.91; BBNNFI = 0.96; CFI = 0.96; RMSEA = 0.06). These values indicate that the theoretical model is well supported by the data.
Results
The sample consisted of 144 older adults, with ages ranging from 60 to 92 years, with a mean of 71.90 years (SD = 7.73 years). Table 1 shows the frequencies of the sociodemographic variables, with the majority being women, having a primary education level, and being widows. The clinical characteristics of the sample are as follows: 26.4% had type 2 diabetes mellitus (T2DM), diagnosed between 1 and 39 years of age, and a mean age of 13.84 ± 9.99 years. Additionally, 60.4% of the sample had arterial hypertension, with the duration of the condition ranging from 1 to 53 years, and a mean age of 15.66 ± 11.94 years. Regarding nutritional status, 4.9% were underweight, 33.3% had a normal weight, 33.3% were overweight, and 28.5% were obese. Furthermore, 25% were below the limit of the musculoskeletal index, 62.5% had low strength, and 65.3% had a speed above 0.8 m/s.
The results indicated that the prevalence of identified sarcopenia was 44.8%. The sarcopenia was higher in women with 45.2%, being more frequent in elderly widows with 55.9%. Regarding the presence of sarcopenia in people with chronic conditions, it was found in 52.9% of older adults with arterial hypertension, as well as in 47.4% of adults with T2DM and 43.9% in people with obesity. The functional capacity indicated that 32.6% had some degree of dependence on basic activities of daily living and 37.5% had some degree of dependence on instrumental activities of life. In terms of physical function within the physical components of QoL, the activities that most significantly limit older adults include bending over or kneeling (19.4%) and climbing multiple flights of stairs (15.3%). Conversely, the activities with the highest percentages of non-limitation were bathing or dressing (65.4%) and making a moderate effort to push (39.6%). Regarding the physical role of the physical components, 8.3% indicated that physical health had made their social and/or family activities very difficult. Moreover, it had made their usual work very difficult. On the other hand, a higher percentage, 41% indicated that the pain had not prevented them from doing their usual work at all and 38.9% indicated that their physical health had not caused them to completely stop their daily activities.
Table 1. Descriptive statistics of sociodemographic variables (n=114)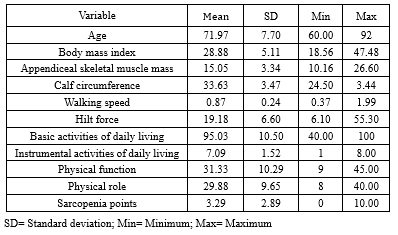 |
In Table 2, the results indicate that there is a significant difference in the means of the variables age, appendicular skeletal muscle mass, gait speed, grip strength, BADL, AIVD, physical function, and physical role among older adults with and without risk of sarcopenia (p<0.05).
Table 3 summarizes the higher signs of sarcopenia, the lower the physical function, the lower the physical role, and the lower the functional capacity. The results showed that there was a greater sign of sarcopenia, older age, lower appendicular skeletal muscle mass, slower walking and less fist strength. Also, it was found that the greater the independence and the better QoL from the physical components, the less slow walking and greater grip strength.
Sarcopenia significantly and negatively affected basic activities of daily living (r=-0.46, p=0.001). In turn, basic life activities positively and significantly affected the physical components of QoL (r=0.54, p=0.001) (Figure 1). Moreover, sarcopenia negatively and significantly affected the instrumental activities of daily living (r=-0.41, p=0.001) and this, in turn, positively and significantly affected the physical components of QoL (r=0.43, p=0.001). The model also demonstrated that sarcopenia directly and negatively affected the physical components of QoL (r=-0.58, p=0.001). Factor loadings were high and statistically significant (p<0.05), indicating convergent construct validity for all factors. The statistical goodness-of-fit indicators were acceptable (χ² = 88.287, df = 77, p = 0.001, relative χ² = 1.14; BBNFI = 0.91, BBNNFI = 0.96, CFI = 0.96, RMSEA = 0.06). All these values suggest that the theoretical model is supported by the data.
Table 3 summarizes the higher signs of sarcopenia, the lower the physical function, the lower the physical role, and the lower the functional capacity. The results showed that there was a greater sign of sarcopenia, older age, lower appendicular skeletal muscle mass, slower walking and less fist strength. Also, it was found that the greater the independence and the better QoL from the physical components, the less slow walking and greater grip strength.
Sarcopenia significantly and negatively affected basic activities of daily living (r=-0.46, p=0.001). In turn, basic life activities positively and significantly affected the physical components of QoL (r=0.54, p=0.001) (Figure 1). Moreover, sarcopenia negatively and significantly affected the instrumental activities of daily living (r=-0.41, p=0.001) and this, in turn, positively and significantly affected the physical components of QoL (r=0.43, p=0.001). The model also demonstrated that sarcopenia directly and negatively affected the physical components of QoL (r=-0.58, p=0.001). Factor loadings were high and statistically significant (p<0.05), indicating convergent construct validity for all factors. The statistical goodness-of-fit indicators were acceptable (χ² = 88.287, df = 77, p = 0.001, relative χ² = 1.14; BBNFI = 0.91, BBNNFI = 0.96, CFI = 0.96, RMSEA = 0.06). All these values suggest that the theoretical model is supported by the data.
|
Table 2. Mann-Whitney U test for anthropometry, clinical data, physical components of HRQOL, and functional capacity for adults with and without risk of sarcopenia (n=144)
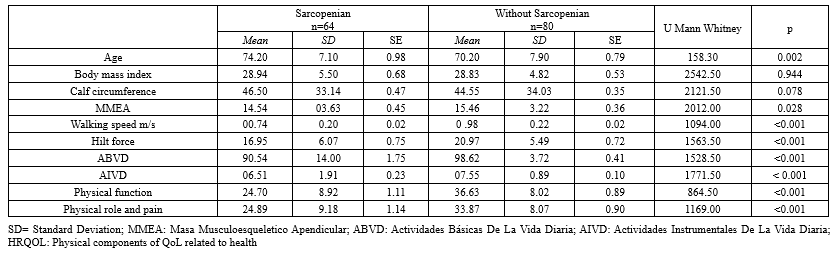 Table 3. Spearman's coefficient of relationship for the study variables (n=144) 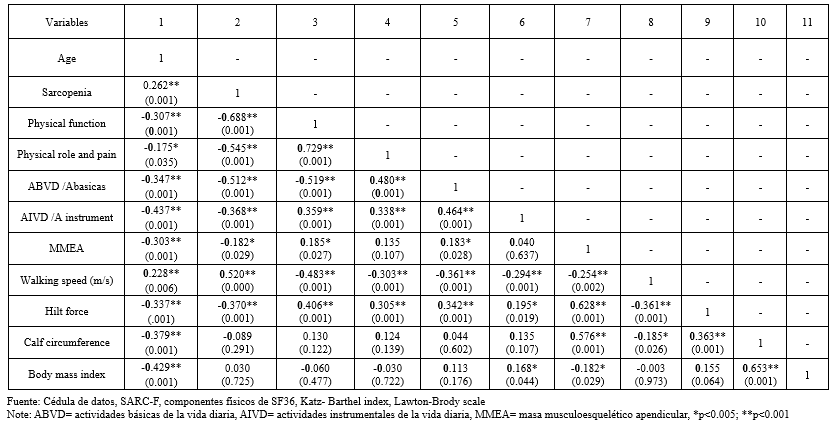 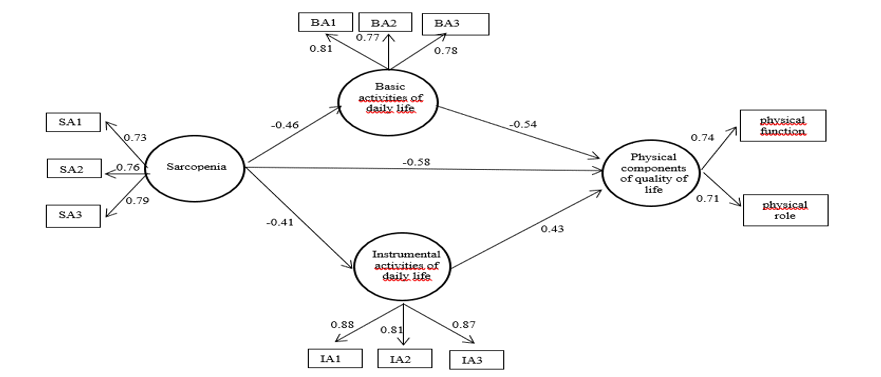 Figure 1. Structural model of sarcopenia, basic activities of daily living, instrumental activities of daily living, and physical components of QoL (χ2 =88.287, df =77, p=0.001, relative χ2=1.14, BBNFI=0.91; BBNNFI=0.96; CFI=0.96, RMSEA=0.06). |
Discussion
The objective of this study was to determine the influence of sarcopenia risk on the physical components of QoL and functional capacity in older adults. The results serve as a key reference for nursing professionals to identify risks that impact the health status of this vulnerable group.
In this study, the risk of sarcopenia was present at 44.8%, being higher than the results reported by Carrillo-Vega et al. (2022) at 31%, Meng et al. (2024) at 20.7%, and Veronose et al. (2024), who identified a prevalence of 25.72%. These findings highlight sarcopenia as an emerging area of geriatrics, particularly relevant in addressing functional impairment and dependency, which affect a significant portion of the aging population (22-25). The current investigation revealed that BMI is at the overweight level, which is higher compared to the studies conducted by Aiken et al. (2024) and Fantin et al. (2024) who found levels of overweight in their sample. In Mexico, obesity is considered a major public health issue due to its association with an increased risk of chronic diseases, which in turn raises the likelihood of developing sarcopenia (26,27). In this study, the participants had a normal calf circumference, with results lower than those reported by Kusaka et al. (2017) but slightly higher than those of Kim et al. (2018). This variation is likely due to the established link between calf circumference and sarcopenia (28,29).
Gait speed in this study was found to be above the normal threshold. The result presented above is lower than that presented by Álvares-Bustos et al. (2024); however, it was higher than the result found in the study conducted by Fantin et al. (2017). The foregoing is due to the modification of the body composition of the elderly; it impacts usual walking speed due to the decrease in strength in the lower extremities (27,30,31). Considering the grip strength, a low force was found in this sample, which is lower than that cited by Hua et al. (2016), as well as much lower than what was found in the study carried out by Iwatmoto et al. (2017) (32,33). Mean below normal parameters indicate changes in skeletal muscle mass cause changes in upper extremity muscle tissue (34). Correspondingly, the grip strength in Mexico was lower compared to studies from other countries.
Regarding appendicular skeletal muscle mass, the mean was 15.05 kg. Compared to other studies, this value was lower. For instance, in the study by Sun et al. (2024), the average muscle mass in older adults was 21.98 kg, while Moon et al. (2018) reported an average of 19.5 kg for men and 12.9 kg for women. This decline in muscle mass may be associated with structural and functional changes in muscle tissue (35,36). However, the BADL indicated a mean of 95.03 points. These results were lower than what was reported by Carrillo-Vega et al. (2024) with a mean of 99.36 points. Moreover, they were higher than those obtained by Moon et al. (2018) with a mean of 40.6 (23,36). In older adults, there are various factors such as the presence of decreased muscle mass and fist strength. This leads to difficulty in performing BADL; thereby increasing the risk of dependency (37).
In terms of instrumental activities of daily living (IADL), the average score in this sample was 7.09 points, which was lower than the results reported by Castillo (2017) and Jun et al. (2022) (38,39). The explanation of BADL and AIVD indicates that the presence of sarcopenia translates into a decrease in functional capacity that leads to the risk of various geriatric syndromes, such as the risk of frailty and an increase in disability (40). On the other hand, the physical components of the health-related QoL reflected an average of 31.33 for physical function and 29.88 for physical role; however, they are lower than what was reported by Silva et al. (2016), with a mean of 65 for the physical function and 65.46 for the physical role. Sánchez-García et al. (2017) reported a mean of 74.4 for the physical function and 65.1 for the physical role (41,42). Overall, the study found that as the signs of sarcopenia increased, physical function and physical role decreased. These results are similar to what was reported by Manrique-Espinoza et al. (2017) and Silva et al. (2016) (42,43). This explains the physical impact of muscle loss and its symptoms on the difficulty of performing physical activities that interfere with life.
The sarcopenia model influences the physical components of QoL and functional capacity by 51.1%. These results are consistent with other studies (44) which found that patients with sarcopenia experienced a decline in QoL within the physical domain and an increase in physical dependence. This occurs because the signs of sarcopenia lead to limitations in performing both daily living and instrumental activities, which are essential for maintaining a good perception of QoL. These limitations modify habits, daily activities, and leisure (8).
These findings have significant implications for nursing practice, highlighting the importance of early detection of factors affecting older adults, such as sarcopenia. Therefore, future interventions are necessary to promote activities that enhance muscle strength, muscle mass, and physical performance, ultimately preventing deterioration in QoL components and functional capacity. Although the relatively small sample size was sufficient to validate the statistical models, it may limit the generalizability of the findings. Additionally, one of the study’s limitations is the inability to generalize its results. Furthermore, economic status and depression were not considered confounding variables, which may have influenced the outcomes. It is suggested to increase the sample size and conduct the study in other areas of Mexico. Likewise, it is suggested to detect muscle mass with the dual-energy X-ray absorptiometry (DXA) as the gold standard, and apply the SPPB assessment instrument to assess physical performance.
Conclusion
Sarcopenia negatively affects approximately half of the physical components of QoL and functional capacity, making it a predictive factor. These findings will serve as a foundation for future research on sarcopenia in the state of Coahuila, Mexico, and will support nursing interventions focused on its prevention, aiming to reduce its impact on the QoL and functional capacity of the elderly. Future research can explore effective interventions to prevent or delay sarcopenia in older Mexican adults, including exercise programs, personalized nutrition, and pharmacological therapies. It may be valuable to assess the influence of psychosocial factors, such as social support and mental health, on physical and functional QoL. Additionally, longitudinal studies can examine how changes in sarcopenia affect functionality and QoL in the long term.
Acknowledgement
The authors thank the participants of this research.
Funding sources
Not applicable.
Ethical statement
This study adhered to the provisions of the General Health Law on Research for Health, specifically the second title concerning the ethical aspects of research involving human subjects. Additionally, it complied with the Official Mexican Standard NOM-012-SSA3-2012, which establishes the criteria for conducting health research on human participants. Written informed consent was obtained from all participants. This research was approved by the Ethics Committee of the Faculty of Nursing at the Autonomous University of Coahuila, under registration number (Missing number).
Conflicts of interest
The authors declare no conflict of interest.
Author contributions
IAMF and SCES conceptualized and designed the study. ALCC contributed to data collection and preliminary analysis. NYTS performed statistical analyses and contributed to the interpretation of results. PETH provided critical insights and supervised the research methodology. IAMF and JAMF supervised the study, and drafted and revised the manuscript. All authors read and approved the final version of the manuscript.
Type of study: Original Article |
Subject:
Nursing
References
1. Instituto Nacional de Estadística y Geogrrafía. Estadística a propósito del día internacional de las personas de edad. México:INGEI;2019. [View at Publisher]
2. Medina-Chávez JH. Envejecimiento de la población y necesidad de la intervención interdisciplinaria. Rev Enferm Inst Mex Seguro Soc. 2015;23(1):1-2. [View at Publisher] [Google Scholar]
3. Perou Y, Faez M, San Miguel J, Diaz Boloy M. Evaluación funcional del adulto mayor y el proceso de atención de enfermería. Rev Inf Cient. 2016;95(5):851-61. [View at Publisher]
4. Acosta Benito MÁ. FMC - Formación Médica Continuada en Atención Primaria. 2017;24(6):334-7. [View at Publisher] [DOI] [Google Scholar]
5. Nemerovsky J. Sarcopenia. Rev Argentina Gerontol y Geriatría. 2016;28-33 [View at Publisher]
6. Canto-Cetina T. Sarcopenia : ¿ epidemia del siglo XXl ? Rev Espec Médico- Quirúrgicas. 2016;21(4):115-6. [View at Publisher] [Google Scholar]
7. Santilli V, Bernetti A, Mangone M, Paoloni M. Clinical definition of sarcopenia. Clin Cases Miner Bone Metab. 2014;11(3):177-80. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Medina I, Carrillo A, Esparza S. Calidad de vida en el adulto mayor con sarcopenia. Rev Mex Enfer. 2018;6(3):93-6. [View at Publisher] [Google Scholar]
9. Rubio D, Rivera L, Borges L, González F. Calidad de vida en el adulto mayor. Varona. 2015;61:1-7. [View at Publisher] [Google Scholar]
10. Varela-Pinedo LF. Salud y calidad de vida en el adulto mayor. Rev Peru Med Exp Salud Publica. 2016;33(2):199-201. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Grove SK, Gray JR. Investigación en enfermería: Desarrollo de la práctica enfermera basada en la evidencia. 7th ed. Elsevier;2019. [View at Publisher]
12. Kang H. Sample size determination and power analysis using the G*Power software. J Educ Eval Health Prof. 2021;18:17. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Parra-Rodríguez L, Szlejf C, García-González AI, Malmstrom TK, Cruz-Arenas E, Rosas-Carrasco O. Cross-Cultural Adaptation and Validation of the Spanish-Language Version of the SARC-F to Assess Sarcopenia in Mexican Community-Dwelling Older Adults. J Am Med Dir Assoc. 2016;17(12):1142-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Bazán M, Peñafiel A, Falvy I, Runzer F. Validez de la escala SARC-F para predicción de dinapenia en adultos mayores, Hospital Central de la Fuerza Aérea del Perú. Gac Med Bilbao. 2022;119(1):20-6. [View at Publisher] [Google Scholar]
15. Sánchez R, García M, Martínez B. Encuesta de Salud SF-36 : Validación en Tres Contextos Culturales de México H. Rev Iberoam Diagnóstico y Evaluación. 2017;3(45):5-16. [View at Publisher] [DOI] [Google Scholar]
16. Cabañero-Martínez MJ, Cabrero-García J, Richart-Martínez M, Muñoz-Mendoza CL. The Spanish versions of the Barthel index (BI) and the Katz index (KI) of activities of daily living (ADL): A structured review. Arch Gerontol Geriatr. 2009;49(1):e77-88. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Velázquez MDC, Irigoyen ME, Delgadillo J, Lazarevich I. The relationship between sarcopenia,undernutrition, physical mobility and basic activities of daily living in a group of elderly women of Mexico City. Nutr Hosp. 2013;28(2):514-21. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Lawton M, Brody E. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9(3):179-86. [View at Publisher] [DOI] [Google Scholar]
19. Trigas-Ferrín M, Ferreira-González L, Meijide-Míguez H. Escalas de valoración funcional en el anciano. Galicia Clin. 2011;72(1):11-6. [View at Publisher] [Google Scholar]
20. Ramírez E, Enríquez-Reyna MC, Garza-Sepúlveda G, Tijerina-Sáenz A, Ramos-Peña E, De la Garza MG. Puntos de corte y validación de una ecuación antropométrica para estimar la masa muscular, en el estudio de la sarcopenia en población mexicana. Salud Publica Mex. 2015;57(6):485-6. [View at Publisher] [PMID] [Google Scholar]
21. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16-31. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Offord NJ, Witham MD. The emergence of sarcopenia as an important entity in older people. Clin Med. 2017;17(4):363-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Carrillo-Vega MF, Pérez-Zepeda MU, Salinas-Escudero G, García-Peña C, Reyes-Ramírez ED, Espinel-Bermúdez MC, et al. Patterns of Muscle-Related Risk Factors for Sarcopenia in Older Mexican Women. Int J Environ Res Public Health. 2022;19(16):10239. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Meng S, He X, Fu X, Zhang X, Tong M, Li W, et al. The prevalence of sarcopenia and risk factors in the older adult in China: a systematic review and meta-analysis. Front Public Health. 2024;12:1415398. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Veronese N, Smith L, Koyanagi A, Hoffman J, Snoussi M, Prokopidis K, et al. Prevalence of sarcopenia in Africa: a systematic review and meta-analysis of observational studies. Aging Clin Exp Res. 2024;36(1):12. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Aiken-Morgan AT, Capuano AW, Wilson RS, Barnes LL. Changes in Body Mass Index and Incident Mild Cognitive Impairment Among African American Older Adults. J Gerontol A Biol Sci Med Sci. 2024;79(3):glad263. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Fantin F, Giani A, Manzato G, Zampieri A, Comellato G, Urbani S, et al. Sarcopenia, sarcopenic obesity, and arterial stiffness among older adults. Front Cardiovasc Med. 2024;11:1272854. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Kusaka S, Takahashhi T, Hiyama Y, Kusumoto Y, Tsuchiya J, Umeda M. Large calf circumference indicates non-sarcopenia despite body mass. J Phys Ther Sci. 2017;29(11):1925-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Kim S, Kim M, Lee Y, Kim B, Yoon TY, Woon CW. Calf Circumference as a Simple Screening Marker for Diagnosing Sarcopenia in Older Korean Adults : the Korean Frailty and Aging Cohort Study ( KFACS ). J Korean Med Sci. 2018;33(20):e151. [View at Publisher] [DOI] [PMID] [Google Scholar]
30. Vergara A. Diagnóstico de sarcopenia mediante determinación de velocidad de archa e indice de masa muscular por método BIA, en adultos mayores del Municio de Ayapango, Estado de México. Universidad Autónoma del Estado de México; 2015. [Thesis] [View at Publisher] [Google Scholar]
31. Álvarez-Bustos A, Carnicero JA, Coelho-Junior HJ, Calvani R, García-García FJ, Marzetti E, et al. Diagnostic and prognostic value of calf circumference for sarcopenia in community-dwelling older adults. J Nutr Heal Aging. 2024;28(8):100290. [View at Publisher] [DOI] [PMID] [Google Scholar]
32. Hua N, Qin C, Wu F, Wang A, Chen J, Zhang Q. High-density lipoprotein cholesterol level and risk of muscle strength decline and sarcopenia in older adults. Clin Nutr. 2024;43(10):2289-95. [View at Publisher] [DOI] [PMID] [Google Scholar]
33. Iwamoto K, Kikuchi Y, Nakano H, Katsurasako T, Mori K, Shiraiwa K, et al. Relationship between Subjective Grip Strength and Physical Functioning among Community-Dwelling Older Women. Geriatr. 2024;9(3):1-10. [View at Publisher] [DOI] [PMID] [Google Scholar]
34. Rastogi Kalyani R, Corriere M, Ferruci L. Age-related and disease-related muscle loss: The effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol. 2014;2(10):819-29. [View at Publisher] [DOI] [PMID] [Google Scholar]
35. Sun Y, Yin T, Li M, Wang F, Qi J, Zhang H, et al. Development and Validation of Estimation Equations for Appendicular Skeletal Muscle Mass in Chinese Community-Dwelling Older Adults. Clin Interv Aging. 2024;19:265-76. [View at Publisher] [DOI] [PMID] [Google Scholar]
36. Moon JJ, Park S-G, Ryu SM, Park C-H. New Skeletal Muscle Mass Index in Diagnosis of Sarcopenia. J Bone Metab. 2018;25(1):15-21. [View at Publisher] [DOI] [PMID] [Google Scholar]
37. Molina JC. Sarcopenia: La importancia del ejercicio. Rev Hosp Clín Univ Chile. 2008;19(4):302-8 [View at Publisher] [Google Scholar]
38. Jun NR, Kim JH, Park JT, Jang JH. Association of Number of Teeth with ADL/IADL in Korean Middle-Aged and Older Adults: An Analysis of the 7th Korean Longitudinal Study of Aging. Int J Environ Res Public Health. 2022;19(19):12840. [View at Publisher] [DOI] [PMID] [Google Scholar]
39. Castillo A. Prevalencia de sarcopenia en el adulto mayor. Hospital Roosevelt Guatemala, Junio 2017. Universidad Rafael Landivar; 2017. [View at Publisher]
40. Masanés Torán F, Navarro López M, Sacanella Meseguer E, López Soto A. ¿Qué es la sarcopenia? Semin la Fund Esp Reumatol. 2010;11(1):14-23. [View at Publisher] [DOI] [Google Scholar]
41. Sánchez-García S, Gallegos-Carrillo K, Espinel-Bermudez MC, Doubova SV, Sánchez-Arenas R, García-Peña C, et al. Comparison of quality of life among community-dwelling older adults with the frailty phenotype. Qual Life Res. 2017;26(10):2693-703. [View at Publisher] [DOI] [PMID] [Google Scholar]
42. Silva L, Go M, Osório N, Pereira L, Mendes M, Galato D. Association between sarcopenia and quality of life in quilombola elderly in Brazil. Int J Gen Med. 2016;9:89-97. [View at Publisher] [DOI] [PMID] [Google Scholar]
43. Manrique-Espinoza B, Salinas-Rodríguez A, Rosas-Carrasco O, Gutiérrez-Robledo LM, Avila-Funes JA. Sarcopenia Is Associated With Physical and Mental Components of Health-Related Quality of Life in Older Adults. J Am Med Dir Assoc. 2017;18(7):636.e1-636.e5. [View at Publisher] [DOI] [PMID] [Google Scholar]
44. Bahat G, Kilic C, Eris S, Karan MA. Power Versus Sarcopenia: Associations with Functionality and Physical Performance Measures. J Nutr Heal Aging. 2021;25(1):13-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |