Volume 20, Issue 2 (10-2023)
J Res Dev Nurs Midw 2023, 20(2): 5-8 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Chabok R, Gholami A, Mahdavifar N, Rad M. The effect of the Benson relaxation technique on sleep quality in women with breast cancer after mastectomy. J Res Dev Nurs Midw 2023; 20 (2) :5-8
URL: http://nmj.goums.ac.ir/article-1-1356-en.html
URL: http://nmj.goums.ac.ir/article-1-1356-en.html
1- Student Research Committee, School of Nursing and Midwifery, Sabzevar University of Medical Sciences, Sabzevar, Iran
2- Department of radiation oncology, Mashhad University of Medical Sciences, Mashhad, Iran
3- Department of Biostatistics and Epidemiology, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
4- Department of Nursing, Nursing and Midwifery School, Iranian Research Center on Healthy Aging, Sabzevar University of Medical Sciences, Sabzevar, Iran ,mostafarad633@yahoo.com
2- Department of radiation oncology, Mashhad University of Medical Sciences, Mashhad, Iran
3- Department of Biostatistics and Epidemiology, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran
4- Department of Nursing, Nursing and Midwifery School, Iranian Research Center on Healthy Aging, Sabzevar University of Medical Sciences, Sabzevar, Iran ,
Keywords: Mastectomy, Sleep Quality, Benson Relaxation Technique, Relaxation therapy, Breast neoplasms
Full-Text [PDF 477 kb]
(1475 Downloads)
| Abstract (HTML) (3612 Views)
Full-Text: (770 Views)
Introduction
Sleep disorders can affect quality of life and increase the risk of developing a variety of systemic disorders and metabolic syndromes, as well as the risk of mortality in individuals (1). There is also a direct relationship between sleep disorders and types of mental disorders, such as anxiety, depression, and immune system disorders (2, 3). Mastectomy may cause physiological, psychosocial, and social problems for the patient, including sleep disorders (4). According to a report, 30% to 60% of breast cancer patients who have undergone mastectomy suffer from sleep disorders (5).
Benzodiazepines are widely used to treat sleep disorders (6, 7). However, these drugs cause side effects, such as tolerance and dependence (8). Another way to improve sleep quality is physical activity, but it may not be tolerable for patients due to the fact that these patients suffer from chronic fatigue (9).
In nursing, many methods of complementary therapy are used in the treatment of cancer-related complications, such as pain, fatigue, and anxiety. These complementary therapies include hypnosis, music therapy, relaxation, etc. (10). The Benson relaxation technique (BRT) is classified as one of the relaxation methods that have been widely used in the treatment of pain, anxiety, and stress, which can cause sleep disorders. This technique has been used in nursing care in the sleep disorders of different patients, but it has not been accomplished in the sleep disorders of breast cancer patients undergoing mastectomy. The Benson relaxation technique is a method that does not require special skills and can be easily learned by patients through oral training or by providing pamphlets and educational films. The patient can do it alone, and her independence is maintained. It does not require time and energy. No side effect has been mentioned, and it does not interfere with other treatments of the patient; it is considered a nursing action (11). When a person is relaxed, it reduces the pressure on the muscles by affecting vital signs and reducing muscle tension. This makes the person less affected by environmental stimuli and is effective in improving sleep quality (12).
Studies have shown that BRT improves sleep quality in the elderly (13), reduces stress, depression, and anxiety in patients with multiple sclerosis (14), and reduces stress in emergency care (15). Moradipour et al also showed that BRT might promote hope among patients with breast cancer (16).
Despite the benefits of BRT mentioned above, its effect on the sleep quality of cancer patients, especially patients who have undergone mastectomy, is still unknown. Therefore, this study aimed to determine the effect of BRT on sleep quality in women with breast cancer after mastectomy. If the technique is effective, it can be used as a supportive method to enhance sleep quality and improve the quality of life of these patients.
Methods
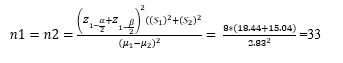
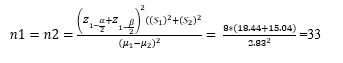
This clinical trial study was accomplished in Shahid Modarres Hospital in Kashmar City, Iran, between April and July 2021. The study population included all women with breast cancer who underwent unilateral modified radical mastectomy (MRM) or extensive radical mastectomy (ERM) and were referred to the screening and chemotherapy center of Shahid Modares Hospital. The sample size was calculated as 36 for each group using the following formula and based on the study of Rakhshani et al. (1), considering α = 0.05 and power = 80%, and 10% attrition rate.
Inclusion criteria were patients who have undergone complete unilateral mastectomy, aged between 30 and 55 years, willingness to participate in the study, full consciousness, no metastasis, had completed all stages of chemotherapy and radiation therapy both before and after the surgery for a duration of 2 weeks, no specific physical complications related to the surgery and chemotherapy, no severe mental disorders, and no addiction. The exclusion criterion was physical complications related to the surgery.
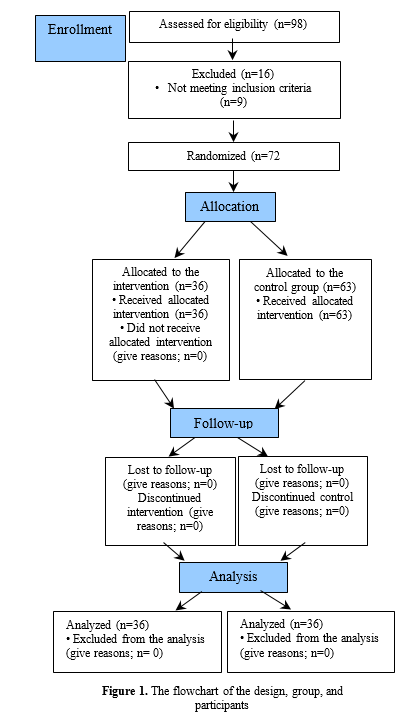
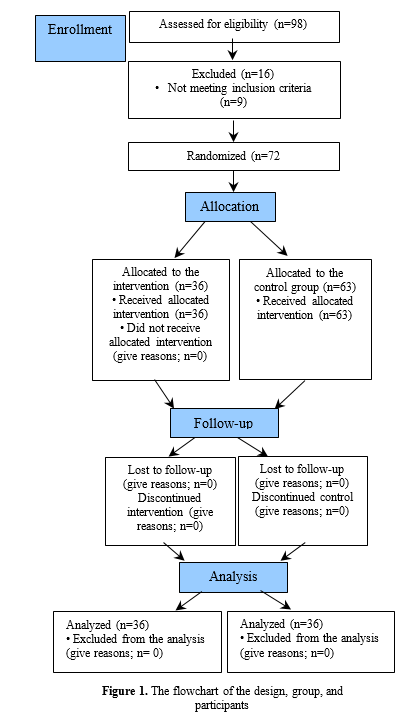
A total of 98 patients had undergone mastectomy in Omid Hospital, affiliated with Mashhad University of Medical Sciences. Of the 98 patients, 81 had sleep disorders, 72 of whom met the inclusion criteria and were included in the study (Figure 1). After completing the Pittsburgh Sleep Quality Index (PSQI) and confirming sleep quality disorders, the research units were selected through convenient sampling and randomly allocated to the intervention (n = 36) and control (n = 36) groups according to permutation blocks designed using R version 3.3.1. Initially, BRT training was conducted in the intervention group by a certified person, who was a psychologist and not aware of the study purpose. The psychologist first provided instruction on the steps of the BRT to each patient individually. This training took place in a quiet room in the surgery clinic. Then, the patient was asked to perform BRT at least once in the presence of the researcher. An audio file was provided to the research units in the intervention group that explained the stages of BRT for further learning. Then, the patient was asked to perform BRT twice a day (preferably in the morning and in the afternoon) and each time for 15 minutes for a period of 2 months at home. Due to the fact that some patients might forget the technique, a self-report questionnaire (checklist) was prepared daily and given to each patient to record their performance on a daily basis. Also, weekly phone calls were made with the patients to ensure that BRT was performed regularly. In addition, a contact number was provided to the research units to contact the researcher in case of any problem or question. If the patients did not perform BRT for 2 days or more a week, they were excluded from the study. The control group did not receive BRT. Since the patients performed the intervention at home, the possibility of diffusion of information between the 2 groups was minimal. After the end of the second month of intervention, the PSQI questionnaire was completed by the researcher for both the intervention and control groups. Data collection was done by the research assistant, who was not aware of the group allocation. The statistician was also unaware of the group allocation during data analysis.
Data were collected using the questionnaire, including demographic characteristics, clinical information, and PSQI. Demographic characteristics included age, marital status, family, children, social support system, income, and sports. The clinical information included the duration of breast cancer, history of surgery, medicinal history, history of other diseases, and use of hypnotics.
PSQI is a self-report tool that assesses sleep quality over the past month and includes 19 questions in 7 components (ie, subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction). Each component receives a score between 0 and 3 and the total score attained from this index ranged from 0 to 21. A score less than 5 indicates the desired sleep quality, and scores equal to or greater than 5 indicate that the person sleeps less or has many problems in at least 2 or more of these components. The validity of PSQI has been proven in various studies. The validity and reliability of this questionnaire were assessed by the Cronbach α method, which is 86% and 89%, respectively (18).
Data were analyzed using SPSS version 16 (SPSS Inc, Chicago, IL, USA) using the chi-square test, analysis of variance (ANOVA), paired t test, and independent t test. The significance level of the tests was considered to be 5%.
Result
A total of 72 women with a mean age of 47.11 ± 4.82 years were evaluated in this study. Most of the participants had secondary education (39%) and were housewives (36%) and married (56%). The 2 groups were not significantly different in terms of demographic characteristics, such as age, education, marital status, income, place of residence, family members whom the person lives with them, children, drug use, narcotic use, exercise, co-infection, family history of mastectomy and smoking (P > 0.05; Table 1). There was a significant difference in job and social-supportive systems between the 2 groups (P < 0.05).
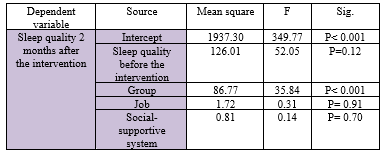
The mean score of sleep quality before the intervention was 9.25 ± 2.5 in the intervention group and 8.47 ± 2.13 in the control group. The result of the independent t test showed that the difference was not statistically significant, and the 2 groups were matched in terms of the mean score of sleep quality (P > 0.05). However, after the intervention, the mean score of sleep quality was 6.63 ± 1.92 in the intervention group and 8.41 ± 2.15 in the control group. The mean score of sleep quality decreased in the intervention group, and this difference was statistically significant (P < 0.001; Table 2). The results of the analysis of covariance (ANCOVA) for sleep quality after the intervention by adjusting the effect of job, social-supportive system, and sleep quality before the intervention showed that the mean of sleep quality was statistically significant between the 2 groups (P < 0.001; Table 3).
The results showed that by adjusting the effect of influential variables (such as age), the total score of sleep quality in the intervention group significantly decreased to 2.6 at the end of the intervention.
Discussion
The results of this study showed that the intervention improved the total score of sleep quality in most components (ie, subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, and daytime dysfunction) in the intervention group. Also, the intervention improved sleep quality for 3 scores. These findings are consistent with other studies conducted on sleep quality using BRT. Rakhshani et al showed that BRT affected sleep quality in chronic heart patients (20). Akıncı et al also showed that body posture and muscle relaxation can reduce pain and improve sleep quality in patients undergoing heart surgery, which is consistent with the present study (19). Since BRT reduces anxiety, depression (15), cancer-related fatigue (22), death anxiety (16) caused by disturbance in body image, and pain following surgery, it can play a role in improving the sleep quality of mastectomy patients. Debellemaniere et al showed that progressive muscle relaxation was effective in reducing anxiety and improving patients' sleep quality during the day, which is consistent with the present study (23). According to a study, BRT can improve sleep quality by affecting vital signs and muscle relaxation and reducing the patient's attention to environmental stimuli (20). In the present study, the total score of sleep quality improved after relaxation techniques in the intervention group. Although BRT improved the sleep quality of these patients, it was not able to return it to a normal level, which may be due to severe sleep disorders in women with cancer, as well as anxiety and depression in these patients; thus, supportive measurements should be taken in these patients before the severity of these disorders (24). These results can indicate that BRT improves a person's psychological symptoms, thus enhancing sleep quality and improving the patients' quality of life. In addition, BRT (as a self-regulation method in stress management) and ignoring deviant thoughts can reduce sleep-disturbing stimuli and improve the quality of sleep (25).
The present study showed that demographic variables (such as job and social-supportive system) have no effect on sleep quality; this is consistent with the study by Jalali et al, who showed no significant relationship between demographic variables, such as job and sleep quality (26). However, Norouzi et al showed that women with a low social-supportive system had a lower quality of sleep, which is not consistent with the results of the present study (27). This may be due to the fact that in our study, most of the participants in the intervention group were in the desired supportive system, and there was a significant difference between the intervention and control groups from the beginning in terms of social support.
Also, the participants had a low mean age, which removed some barriers (including cognitive barriers), facilitated learning, and increased the accuracy and focus of participants to implement the intervention. The other strength was the acceptable cultural level of individuals to cooperate and participate in the research. This means that many participants had the experience of participating in the research and had a high level of motivation to cooperate in the study due to the positive and satisfactory results that they had obtained from previous studies.
One of the limitations of this study was the COVID-19 pandemic. Since cancer patients were considered a high-risk group, this pandemic increased stress and anxiety in patients and acted as an intervening factor. On the other hand, one of the effects of the COVID-19 pandemic was a decrease in patient referrals to medical units, and the access to the participants was more difficult than the normal situation. To counteract this limitation, further studies are needed to be performed in non-pandemic situations. The other limitation of the study was the attitude of participants toward BRT, which led to the lack of cooperation and non-acceptance among some participants. To address this limitation, we explained to the participants that BRT, while not requiring time, energy, and expense, may be effective in resolving sleep disorders.
Conclusion
The Benson relaxation technique has a positive effect on sleep quality in patients with breast cancer undergoing mastectomy and improved sleep quality; thus, it can be taught by nurses as a useful method to improve the sleep quality of patients in oncology and chemotherapy wards.
Acknowledgement
We appreciate the support of Sabzevar University of Medical Sciences for the implementation of this project, the officials and staff of the Screening and Chemotherapy Clinic of Shahid Modares Hospital in Kashmar City, and the patients participating in the study.
Funding sources
This article is part of the thesis approved and supported by Sabzevar University of Medical Sciences (code: IR.MEDSAB.REC.1399.061) in 2020.
Ethical statement
This study was approved by the Ethics Committee of Sabzevar University of Medical Sciences (code: IR.MEDSAB.REC.1399.061). Also, the study was registered on the Iranian Registry of Clinical Trials website (IRCT20210108049964N1). The study method was completely explained to the participants. In addition, the participants were informed that their participation in the study was optional, and they could leave the study at any time and without any restrictions. They were assured that their data would remain confidential, and the results of the research would be reported to them. Finally, written informed consent was obtained from all participants. The study entered the implementation phase after obtaining permission from the Vice Chancellor for Research of Sabzevar University of Medical Sciences and the Vice Chancellor for Research of Kashmar Hospital.
Conflicts of interest
The authors declare that there is no conflict of interest.
Author contributions
M.R. and R.C. designed the study. R.C. gathered data. M.R., R.C., A.G., and N.M. contributed to data analysis, interpretation, and the writing of the manuscript. M.R. supervised the study. All authors read and approved the final manuscript.
Sleep disorders can affect quality of life and increase the risk of developing a variety of systemic disorders and metabolic syndromes, as well as the risk of mortality in individuals (1). There is also a direct relationship between sleep disorders and types of mental disorders, such as anxiety, depression, and immune system disorders (2, 3). Mastectomy may cause physiological, psychosocial, and social problems for the patient, including sleep disorders (4). According to a report, 30% to 60% of breast cancer patients who have undergone mastectomy suffer from sleep disorders (5).
Benzodiazepines are widely used to treat sleep disorders (6, 7). However, these drugs cause side effects, such as tolerance and dependence (8). Another way to improve sleep quality is physical activity, but it may not be tolerable for patients due to the fact that these patients suffer from chronic fatigue (9).
In nursing, many methods of complementary therapy are used in the treatment of cancer-related complications, such as pain, fatigue, and anxiety. These complementary therapies include hypnosis, music therapy, relaxation, etc. (10). The Benson relaxation technique (BRT) is classified as one of the relaxation methods that have been widely used in the treatment of pain, anxiety, and stress, which can cause sleep disorders. This technique has been used in nursing care in the sleep disorders of different patients, but it has not been accomplished in the sleep disorders of breast cancer patients undergoing mastectomy. The Benson relaxation technique is a method that does not require special skills and can be easily learned by patients through oral training or by providing pamphlets and educational films. The patient can do it alone, and her independence is maintained. It does not require time and energy. No side effect has been mentioned, and it does not interfere with other treatments of the patient; it is considered a nursing action (11). When a person is relaxed, it reduces the pressure on the muscles by affecting vital signs and reducing muscle tension. This makes the person less affected by environmental stimuli and is effective in improving sleep quality (12).
Studies have shown that BRT improves sleep quality in the elderly (13), reduces stress, depression, and anxiety in patients with multiple sclerosis (14), and reduces stress in emergency care (15). Moradipour et al also showed that BRT might promote hope among patients with breast cancer (16).
Despite the benefits of BRT mentioned above, its effect on the sleep quality of cancer patients, especially patients who have undergone mastectomy, is still unknown. Therefore, this study aimed to determine the effect of BRT on sleep quality in women with breast cancer after mastectomy. If the technique is effective, it can be used as a supportive method to enhance sleep quality and improve the quality of life of these patients.
Methods
This clinical trial study was accomplished in Shahid Modarres Hospital in Kashmar City, Iran, between April and July 2021. The study population included all women with breast cancer who underwent unilateral modified radical mastectomy (MRM) or extensive radical mastectomy (ERM) and were referred to the screening and chemotherapy center of Shahid Modares Hospital. The sample size was calculated as 36 for each group using the following formula and based on the study of Rakhshani et al. (1), considering α = 0.05 and power = 80%, and 10% attrition rate.
Inclusion criteria were patients who have undergone complete unilateral mastectomy, aged between 30 and 55 years, willingness to participate in the study, full consciousness, no metastasis, had completed all stages of chemotherapy and radiation therapy both before and after the surgery for a duration of 2 weeks, no specific physical complications related to the surgery and chemotherapy, no severe mental disorders, and no addiction. The exclusion criterion was physical complications related to the surgery.
A total of 98 patients had undergone mastectomy in Omid Hospital, affiliated with Mashhad University of Medical Sciences. Of the 98 patients, 81 had sleep disorders, 72 of whom met the inclusion criteria and were included in the study (Figure 1). After completing the Pittsburgh Sleep Quality Index (PSQI) and confirming sleep quality disorders, the research units were selected through convenient sampling and randomly allocated to the intervention (n = 36) and control (n = 36) groups according to permutation blocks designed using R version 3.3.1. Initially, BRT training was conducted in the intervention group by a certified person, who was a psychologist and not aware of the study purpose. The psychologist first provided instruction on the steps of the BRT to each patient individually. This training took place in a quiet room in the surgery clinic. Then, the patient was asked to perform BRT at least once in the presence of the researcher. An audio file was provided to the research units in the intervention group that explained the stages of BRT for further learning. Then, the patient was asked to perform BRT twice a day (preferably in the morning and in the afternoon) and each time for 15 minutes for a period of 2 months at home. Due to the fact that some patients might forget the technique, a self-report questionnaire (checklist) was prepared daily and given to each patient to record their performance on a daily basis. Also, weekly phone calls were made with the patients to ensure that BRT was performed regularly. In addition, a contact number was provided to the research units to contact the researcher in case of any problem or question. If the patients did not perform BRT for 2 days or more a week, they were excluded from the study. The control group did not receive BRT. Since the patients performed the intervention at home, the possibility of diffusion of information between the 2 groups was minimal. After the end of the second month of intervention, the PSQI questionnaire was completed by the researcher for both the intervention and control groups. Data collection was done by the research assistant, who was not aware of the group allocation. The statistician was also unaware of the group allocation during data analysis.
Data were collected using the questionnaire, including demographic characteristics, clinical information, and PSQI. Demographic characteristics included age, marital status, family, children, social support system, income, and sports. The clinical information included the duration of breast cancer, history of surgery, medicinal history, history of other diseases, and use of hypnotics.
PSQI is a self-report tool that assesses sleep quality over the past month and includes 19 questions in 7 components (ie, subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction). Each component receives a score between 0 and 3 and the total score attained from this index ranged from 0 to 21. A score less than 5 indicates the desired sleep quality, and scores equal to or greater than 5 indicate that the person sleeps less or has many problems in at least 2 or more of these components. The validity of PSQI has been proven in various studies. The validity and reliability of this questionnaire were assessed by the Cronbach α method, which is 86% and 89%, respectively (18).
Data were analyzed using SPSS version 16 (SPSS Inc, Chicago, IL, USA) using the chi-square test, analysis of variance (ANOVA), paired t test, and independent t test. The significance level of the tests was considered to be 5%.
Result
A total of 72 women with a mean age of 47.11 ± 4.82 years were evaluated in this study. Most of the participants had secondary education (39%) and were housewives (36%) and married (56%). The 2 groups were not significantly different in terms of demographic characteristics, such as age, education, marital status, income, place of residence, family members whom the person lives with them, children, drug use, narcotic use, exercise, co-infection, family history of mastectomy and smoking (P > 0.05; Table 1). There was a significant difference in job and social-supportive systems between the 2 groups (P < 0.05).
|
Table 3. The results of analysis of covariance with the control confounding Effect of the group before the intervention, job, and social-supportive system
 |
The results of this study showed that the intervention improved the total score of sleep quality in most components (ie, subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, and daytime dysfunction) in the intervention group. Also, the intervention improved sleep quality for 3 scores. These findings are consistent with other studies conducted on sleep quality using BRT. Rakhshani et al showed that BRT affected sleep quality in chronic heart patients (20). Akıncı et al also showed that body posture and muscle relaxation can reduce pain and improve sleep quality in patients undergoing heart surgery, which is consistent with the present study (19). Since BRT reduces anxiety, depression (15), cancer-related fatigue (22), death anxiety (16) caused by disturbance in body image, and pain following surgery, it can play a role in improving the sleep quality of mastectomy patients. Debellemaniere et al showed that progressive muscle relaxation was effective in reducing anxiety and improving patients' sleep quality during the day, which is consistent with the present study (23). According to a study, BRT can improve sleep quality by affecting vital signs and muscle relaxation and reducing the patient's attention to environmental stimuli (20). In the present study, the total score of sleep quality improved after relaxation techniques in the intervention group. Although BRT improved the sleep quality of these patients, it was not able to return it to a normal level, which may be due to severe sleep disorders in women with cancer, as well as anxiety and depression in these patients; thus, supportive measurements should be taken in these patients before the severity of these disorders (24). These results can indicate that BRT improves a person's psychological symptoms, thus enhancing sleep quality and improving the patients' quality of life. In addition, BRT (as a self-regulation method in stress management) and ignoring deviant thoughts can reduce sleep-disturbing stimuli and improve the quality of sleep (25).
The present study showed that demographic variables (such as job and social-supportive system) have no effect on sleep quality; this is consistent with the study by Jalali et al, who showed no significant relationship between demographic variables, such as job and sleep quality (26). However, Norouzi et al showed that women with a low social-supportive system had a lower quality of sleep, which is not consistent with the results of the present study (27). This may be due to the fact that in our study, most of the participants in the intervention group were in the desired supportive system, and there was a significant difference between the intervention and control groups from the beginning in terms of social support.
Also, the participants had a low mean age, which removed some barriers (including cognitive barriers), facilitated learning, and increased the accuracy and focus of participants to implement the intervention. The other strength was the acceptable cultural level of individuals to cooperate and participate in the research. This means that many participants had the experience of participating in the research and had a high level of motivation to cooperate in the study due to the positive and satisfactory results that they had obtained from previous studies.
One of the limitations of this study was the COVID-19 pandemic. Since cancer patients were considered a high-risk group, this pandemic increased stress and anxiety in patients and acted as an intervening factor. On the other hand, one of the effects of the COVID-19 pandemic was a decrease in patient referrals to medical units, and the access to the participants was more difficult than the normal situation. To counteract this limitation, further studies are needed to be performed in non-pandemic situations. The other limitation of the study was the attitude of participants toward BRT, which led to the lack of cooperation and non-acceptance among some participants. To address this limitation, we explained to the participants that BRT, while not requiring time, energy, and expense, may be effective in resolving sleep disorders.
Conclusion
The Benson relaxation technique has a positive effect on sleep quality in patients with breast cancer undergoing mastectomy and improved sleep quality; thus, it can be taught by nurses as a useful method to improve the sleep quality of patients in oncology and chemotherapy wards.
Acknowledgement
We appreciate the support of Sabzevar University of Medical Sciences for the implementation of this project, the officials and staff of the Screening and Chemotherapy Clinic of Shahid Modares Hospital in Kashmar City, and the patients participating in the study.
Funding sources
This article is part of the thesis approved and supported by Sabzevar University of Medical Sciences (code: IR.MEDSAB.REC.1399.061) in 2020.
Ethical statement
This study was approved by the Ethics Committee of Sabzevar University of Medical Sciences (code: IR.MEDSAB.REC.1399.061). Also, the study was registered on the Iranian Registry of Clinical Trials website (IRCT20210108049964N1). The study method was completely explained to the participants. In addition, the participants were informed that their participation in the study was optional, and they could leave the study at any time and without any restrictions. They were assured that their data would remain confidential, and the results of the research would be reported to them. Finally, written informed consent was obtained from all participants. The study entered the implementation phase after obtaining permission from the Vice Chancellor for Research of Sabzevar University of Medical Sciences and the Vice Chancellor for Research of Kashmar Hospital.
Conflicts of interest
The authors declare that there is no conflict of interest.
Author contributions
M.R. and R.C. designed the study. R.C. gathered data. M.R., R.C., A.G., and N.M. contributed to data analysis, interpretation, and the writing of the manuscript. M.R. supervised the study. All authors read and approved the final manuscript.
Type of study: Original Article |
Subject:
Nursing
References
1. Walker WH, Borniger JC. Molecular Mechanisms of Cancer-Induced Sleep Disruption. Int J Mol Sci. 2019;20(11):2780. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Miniati M, Palagini L, Maglio A, Marazziti D, Dell'Osso L. Can sleep disturbance be a cue of mood spectrum comorbidity? A preliminary study in panic disorder. CNS spectr. 2020:25(1):32-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Wang L, Zhang Y. The factors influencing psychological resilience in breast cancer patients undergoing mastectomy and the effects of mindfulness-based stress reduction on the patients' psychological resilience and anxiety. Int J Clin Exp Med. 2020;13(11):8924-32. [View at Publisher] [Google Scholar]
4. Zielonke N, Gini A, Jansen EE, Anttila A, Segnan N, Ponti A, et al. Evidence for reducing cancer-specific mortality due to screening for breast cancer in Europe: A systematic review. Eur J Cancer. 2020;127(1): 191-206. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Chang W-P, Chang Y-P. Meta-Analysis of Changes in Sleep Quality of Women with Breast Cancer before and after Therapy. Breast Care (Basel). 2020;15(3):227-35. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Aždajić MD, Likić R, Aždajić S, Šitum M, Lovrić I, Grbić DŠ. Outpatient benzodiazepine utilization in Croatia: drug use or misuse. Int J Clin Pharm. 2019;41(6):1526-35. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Baricault B, Palmaro A, Lapeyre-Mestre M. Mortality Related to Benzodiazepines or Other Psychotropic Drugs in Patients with Cancer. Clinical Therapeutics. 2017;39(8):e12-3. [View at Publisher] [DOI] [Google Scholar]
8. Freeman D, Sheaves B, Waite F, Harvey AG, Harrison PJ. Sleep disturbance and psychiatric disorders. Lancet Psychiatry. 2020;7(7):628-37. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Bower JE, Wiley J, Petersen L, Irwin MR, Cole SW, Ganz PA. Fatigue after breast cancer treatment: Biobehavioral predictors of fatigue trajectories. Health Psychol. 2018;37(11):1025-34. [] [DOI] [PMID] [Google Scholar]
10. Efendi S, Agus AI, Syatriani S, Amir H, Alam RI, Nurdin S, et al. The Effect of Benson Relaxation on Quality of Sleep of Cancer Patients. Open Access Maced J Med Sci. 2022;10(G):99-104. [View at Publisher] [DOI] [Google Scholar]
11. Moradipour S, Soleimani M A, Sheikhi M R, Pahlevan Sharif S. Examining the Effect of Benson's Relaxation Technique on Hope among Patients with Breast Cancer. IJPN. 2018;6(3) :10-17. [View at Publisher] [DOI] [Google Scholar]
12. Momen R, Roshandel M , Pishgooie SAH. The effect of Benson relaxation method on pain severity after laminectomy in admitted patients to AJA hospitals. Military Caring Sciences Journal. 2018; 4(3):168-77. [View at Publisher] [DOI] [Google Scholar]
13. Khazaei Ghozhdi M, Ghaljeh M, Khazaei N. The Effect of Progressive Muscle Relaxation Technique on Fatigue, Pain and Quality of Life in Dialysis Patients: A Clinical Trial Study. Evidence Based Care. 2022;12(4):7-16. [View at Publisher] [DOI] [Google Scholar]
14. Habibollahpour M, Ranjkesh F, Motalebi SA, Mohammadi F. The Impact of Benson's relaxation technique on the quality of sleep in the elderly. Topics in Geriatric Rehabilitation. 2019;35(1):88-94. [View at Publisher] [DOI] [Google Scholar]
15. Akbari A, Ahmadi F, Jalili E, Khazaei S. The effect of relaxation technique (Jacobsen and Benson) on depression, anxiety, and stress in patients with multiple sclerosis. Current Psychiatry Research and Reviews Formerly: Current Psychiatry Reviews. 2020;16(3):213-9. [View at Publisher] [DOI] [Google Scholar]
16. Ahmadi F, Dalvand S, Babaie M, Akbari A, Khazaei S. Impact of White Noise and Benson's Relaxation Technique on Death Anxiety in Patients Undergoing Coronary Artery Bypass Graft Surgery: A Randomized Clinical Trial. Evidence Based Care. 2022;12(1):40-7. [View at Publisher] [DOI] [Google Scholar]
17. Shorofi SA, Nozari-Mirarkolaei F, Arbon P, Bagheri-Nesamie M. Depression and Sleep Quality among Iranian Women with Breast Cancer. Asian Pac J Cancer Prev. 2021;22(11):3433-40. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Costa AR, Fontes F, Pereira S, Gonçalves M, Azevedo A, Lunet N. Impact of breast cancer treatments on sleep disturbances - A systematic review. Breast. 2014;23(6):697-709. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Akinci B, Yeldan I, Bayramoglu Z, Akpinar T. The effects of posture and relaxation training on sleep, dyspnea, pain and, quality of life in the short-term after cardiac surgery: Journal of Thoracic and Cardiovascular Surgery. 2016;24(2):258-65. [View at Publisher] [DOI] [Google Scholar]
20. Rakhshani M, Akbarzadeh R, Koshan M, Hashemi Nik SM. Effect of the benson relaxation technique on quality of sleep in patients with chronic heart disease. Journal of Sabzevar Univ Med Sci. 2014;21(3):492-50. [View at Publisher] [Google Scholar]
21. Farrahi J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Psychometric properties of the Persian version of the Pittsburgh Sleep Quality Index addendum for PTSD (PSQI-A). Sleep Breath. 2009;13(3): 259-62. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Demiralp M, Oflaz F, Komurcu S. Effects of relaxation training on sleep quality and fatigue in patients with breast cancer undergoing adjuvant chemotherapy. J Clin Nurs. 2010;19(7‐8):1073-83. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Debellemaniere E, Gomez-Merino D, Erblang M, Dorey R, Genot M, Perreaut-Pierre E, et al. Using relaxation techniques to improve sleep during naps. Ind Health. 2018;56(3):220-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Kim M-S, Kim SY, Kim J-H, Park B, Choi HG. Depression in breast cancer patients who have undergone mastectomy: a national cohort study. PloS One. 2017;12(4):e0175395. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Rambod M, Pourali-Mohammadi N, Pasyar N, Rafii F, Sharif F. The effect of Benson's relaxation technique on the quality of sleep of Iranian hemodialysis patients: a randomized trial. Complement Ther Med. 2013;21(6):577-84. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Jalali R, Rezaei M, Khaledi Paveh B, Aznab M, AmiriFard N, Mohammadi E. Sleep Disorder and its Correlates in Patients Undergoing Chemotherapy. IJN: Nursing Care Research Center. 2016;29(99 and 100):76-85. [View at Publisher] [DOI] [Google Scholar]
27. Rad AK, Noroozi M, AhmariTehran H, Rahmani A. Quality of sleep and related factors in Breast Cancer Patients Receiving Chemotherapy in Qom 2011. Iranian Journal of Breast Diseases. 2012;4(4):51-60. [View at Publisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |