Volume 22, Issue 1 (3-2025)
J Res Dev Nurs Midw 2025, 22(1): 7-12 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Mohammadian B, Bakhtiarpour S, Naderi F, Dasht Bozorgi Z. The relationship between perceived stress and postpartum depression through the mediating role of marital satisfaction in postpartum women. J Res Dev Nurs Midw 2025; 22 (1) :7-12
URL: http://nmj.goums.ac.ir/article-1-1852-en.html
URL: http://nmj.goums.ac.ir/article-1-1852-en.html
1- Department of Psychology, Ahvaz Branch, Islamic Azad University, Ahvaz, Iran
2- Department of Psychology, Ahvaz Branch, Islamic Azad University, Ahvaz, Iran ,bakhtiyarpours@gmail.com
2- Department of Psychology, Ahvaz Branch, Islamic Azad University, Ahvaz, Iran ,
Full-Text [PDF 485 kb]
(1609 Downloads)
| Abstract (HTML) (3042 Views)
Discussion
This study investigated the intricate relationship between perceived stress, marital satisfaction, and PPD among postpartum women, specifically focusing on the mediating role of marital satisfaction. The findings revealed significant associations, shedding light on the complex interplay of these factors during the transition to motherhood.
Consistent with previous research (28), a significant negative correlation was observed between perceived stress and marital satisfaction. As perceived stress increased, marital satisfaction decreased. This suggests that the stressors inherent in the pre- and postpartum periods can significantly erode marital quality. Factors such as disagreements regarding the child's gender, unintended pregnancies, conflicts with extended family, parenting stress, and hormonal fluctuations likely contribute to this decline. The assumption of maternal caregiving responsibilities can lead to caregiving stress and self-doubt. At the same time, discrepancies between expected and actual parental roles and spousal differences can further strain marital satisfaction (15). Moreover, the physiological, psychological, and social changes associated with pregnancy can heighten anxiety and distress, negatively impacting marital harmony (18). This underscores the critical role of perceived stress as a significant risk factor for diminished marital satisfaction.
Furthermore, a significant negative correlation was found between marital satisfaction and PPD, aligning with previous studies (29). Lower marital satisfaction was associated with increased PPD, highlighting the interconnectedness of partners' experiences during the transition to parenthood. This period often sees heightened marital conflict and dissatisfaction, particularly among first-time parents (30). Psychological disorders like depression or anxiety in either partner can exacerbate interpersonal conflict and negative emotions, further contributing to this association. The stressors mentioned earlier, including disagreements regarding the child's sex, unintended pregnancies, and parenting stress, can directly impact marital quality and satisfaction, ultimately influencing the risk of PPD.
The study also demonstrated a significant correlation between perceived stress and PPD, consistent with previous research (31,32). Stressful life events, parental stress, unintended pregnancy, and neonatal hospitalization were identified as contributing factors to PPD. The presence of various stressors, such as primiparity, childbirth complications, infant illness, and substance abuse, can lead to psychological distress and harm in mothers. Pregnancy itself is a significant life event requiring substantial adjustments, and the social and economic burden of unplanned pregnancies can exacerbate stress and psychological distress (31).
Crucially, the analysis of indirect effects revealed that perceived stress can influence PPD through the mediating role of marital satisfaction. Elevated perceived stress negatively impacts marital satisfaction, which in turn increases PPD. This aligns with prior research (33), indicating that stress can lead to decreased marital satisfaction, increased conflict, and subsequent PPD. Unchecked perceived stress, stemming from factors like the transition to parenthood, infant temperament incompatibility, and feelings of parental inadequacy, can become chronic and prolonged. The psychological burden imposed by psychosocial stressors during and after pregnancy can significantly contribute to PPD (33).
The demands of motherhood present a unique set of stressors, often evolving into long-term parenting-related challenges. Breastfeeding can be time-consuming, and inadequate infant care can exacerbate interparental conflict, increasing the risk of PPD (34). The multitude of changes accompanying pregnancy and the postpartum period can lead to heightened worry, anxiety, and distress, impacting marital satisfaction. As hypothesized, elevated perceived stress, coupled with diminished marital satisfaction, creates a context conducive to the development of PPD in mothers. This study underscores the importance of addressing perceived stress and marital satisfaction in interventions to prevent and mitigate PPD. Future research should explore how these factors interact and evaluate the effectiveness of targeted interventions to support postpartum women and their families.
This study has several notable strengths. The relatively large sample size enhances statistical power and the generalizability of the findings to similar populations. The use of validated instruments, including the EPDS and PSS, strengthens the reliability and validity of the measurements. Furthermore, applying structural equation modeling allowed for examining complex relationships among multiple variables, including the mediating role of marital satisfaction. This study contributes to the literature by providing empirical evidence for this mediation, a relationship that has not been extensively explored in this population.
However, several limitations should be acknowledged. Using a convenience sampling method limits the generalizability of the findings to other populations. The cross-sectional design of this study precludes definitive conclusions about causality. Longitudinal studies are needed to establish the temporal ordering of the observed relationships. The reliance on self-report measures may have introduced response bias. Finally, the sample consisted of postpartum women in Ahvaz, Iran, which may limit the generalizability of the findings to women in other cultural contexts.
Conclusion
This study confirms that perceived stress and marital satisfaction are crucial predictors of PPD. As predicted, high perceived stress reduces marital satisfaction, which in turn elevates the risk of PPD, illustrating an indirect pathway. Direct links between perceived stress and PPD and marital satisfaction and PPD emphasize the complex nature of PPD's development. These findings highlight the need for interventions addressing both perceived stress and marital satisfaction to prevent and mitigate PPD. Cognitive behavioral therapy can effectively reduce stress and improve coping. Couple-based therapies, like Emotionally Focused Therapy, can enhance marital communication and intimacy. Future research should explore the specific cognitive and behavioral processes mediating these relationships and use longitudinal studies to identify optimal intervention times. A deeper understanding will enable clinicians, particularly midwives and family nurses, to provide more effective support for the mental health of postpartum women.
Acknowledgement
The authors express their sincere gratitude to the women who generously participated in this research by completing the questionnaires.
Funding sources
No financial support was received for this article.
Ethical statement
All ethical principles in human research, in accordance with the Helsinki Declaration, were adhered to, including written informed consent, the right to confidentiality and the protection of individual identities of participants, voluntary participation, and the right to withdraw from the study. The Ethics Review Board of the Islamic Azad University, Ahvaz Branch, approved the present study under the following reference number: IR.IAU.AHVAZ.REC.1402.028.
Conflicts of interest
There was no conflict of interest to be declared.
Author contributions
BM: Study concept and design, data acquisition, analysis and interpretation of data, and statistical analysis. SB: Administrative, technical, and material support, study supervision. FN and ZDB: Critical revision of the manuscript for important intellectual content.
Full-Text: (970 Views)
Introduction
Pregnancy is a transformative period marked by significant physical, psychological, and social changes that can lead to increased worry, anxiety, stress, and depression (1). Maternal depression, particularly during the postpartum period-a time of heightened challenges-can occur at twice the rate of other life stages, persisting for months or even a year, with a 50% recurrence risk in subsequent pregnancies. While commonly referred to as postpartum depression (PPD), the DSM-5 uses the term perinatal depression to encompass mood disorders occurring both during pregnancy (Antepartum) and after delivery (Postpartum). The DSM-5 recognizes that depressive symptoms can emerge during pregnancy and extend into the postpartum period (2). Specifically, Major Depressive Disorder with peripartum onset is diagnosed when a major depressive episode occurs during pregnancy or within four to six weeks postpartum (3). Globally, the estimated prevalence of perinatal depression is 10-15% (4). Early detection, risk factor identification, and timely intervention are crucial for safeguarding the mental health of postpartum women and their newborns (5).
Despite extensive research, the etiology of PPD remains incompletely understood (6,7). Numerous risk factors, categorized as psychological, physiological, and social, have been identified (8). Psychological factors such as perceived stress, low self-esteem, and a history of depression are consistently linked to the increased risk of PPD (9). Physiological factors, including hormonal changes, gestational diabetes, and thyroid dysfunction, also play a significant role. Social factors like lack of social support, marital dissatisfaction, and stressful life events further elevate the risk of PPD (10).
Stressful conditions and elevated perceived stress levels significantly impact PPD prevalence. Perceived stress directly correlates with the intensity of neuroendocrine responses, triggering hormone secretion (11). Stressors during childhood, adolescence, and adulthood can elevate stress levels and activate the hypothalamic-pituitary-adrenal axis, leading to cortisol release (12). Perceived stress reflects an individual's subjective evaluation of demands and coping abilities. In pregnant women, concerns about pregnancy, childbirth, parenthood, financial pressures, relationship changes, lack of social support, and past trauma contribute to elevated perceived stress, significantly increasing the risk of PPD (13,14).
Marital satisfaction is a key factor in PPD development (15). Postpartum, approximately 80% of first-time mothers experience decreased marital satisfaction (16). The transition to parenthood affects interpersonal resources (17). Intimacy and relationship satisfaction enhance mood and coping abilities (18). Partner support buffers stress, aiding in navigating childbirth and parenting challenges (19). Marital quality depends on couples' adaptation, with decreased satisfaction in one partner affecting the other (16). Hudson et al. (20) showed that high levels of intimacy and satisfaction in a partnership lead to improved emotional well-being.
Research exploring the relationship between perceived stress, marital satisfaction, and PPD is essential for understanding and addressing this significant global mental health concern. While existing research has established links between these factors, important gaps remain. Primarily, most studies have focused on individual factors like perceived stress or PPD in isolation rather than examining their complex interplay within the marital dyad. Although research has shown that a decline in one partner's satisfaction significantly affects the other (16), the specific mechanisms through which marital satisfaction influences PPD development remain unclear. Secondly, the predominantly cross-sectional nature of previous research limits the ability to determine causality. Therefore, this study aims to investigate the direct and indirect effects of perceived stress on PPD, specifically examining the mediating role of marital satisfaction in this relationship. We hypothesize that higher levels of perceived stress will be significantly associated with an increased risk of PPD and that marital satisfaction will mediate the relationship between perceived stress and PPD.
Methods
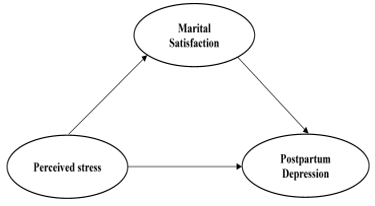
This study employed a cross-sectional design using structural equation modeling (SEM) to examine the direct and indirect effects of perceived stress on PPD, with marital satisfaction as a proposed mediator. A conceptual model (Figure 1) guided the analysis. Participants were recruited using convenience sampling, a form of non-probability sampling, from various health centers in Ahvaz City, Iran. These health centers provide primary healthcare services to a diverse population in Ahvaz, a major city in southwestern Iran. The inclusion criteria were as follows: (1) women within six months postpartum; (2) women living with their husbands; (3) women whose childbirth resulted in a live birth; (4) women who provided informed consent to participate in the study; and (5) women who had completed at least a high school education. The exclusion criteria included women who experienced a major stressful life event (e.g., death of a close family member, serious accident, natural disaster) in the three months preceding data collection, as such events could significantly confound the assessment of perceived stress related to the postpartum period.
Pregnancy is a transformative period marked by significant physical, psychological, and social changes that can lead to increased worry, anxiety, stress, and depression (1). Maternal depression, particularly during the postpartum period-a time of heightened challenges-can occur at twice the rate of other life stages, persisting for months or even a year, with a 50% recurrence risk in subsequent pregnancies. While commonly referred to as postpartum depression (PPD), the DSM-5 uses the term perinatal depression to encompass mood disorders occurring both during pregnancy (Antepartum) and after delivery (Postpartum). The DSM-5 recognizes that depressive symptoms can emerge during pregnancy and extend into the postpartum period (2). Specifically, Major Depressive Disorder with peripartum onset is diagnosed when a major depressive episode occurs during pregnancy or within four to six weeks postpartum (3). Globally, the estimated prevalence of perinatal depression is 10-15% (4). Early detection, risk factor identification, and timely intervention are crucial for safeguarding the mental health of postpartum women and their newborns (5).
Despite extensive research, the etiology of PPD remains incompletely understood (6,7). Numerous risk factors, categorized as psychological, physiological, and social, have been identified (8). Psychological factors such as perceived stress, low self-esteem, and a history of depression are consistently linked to the increased risk of PPD (9). Physiological factors, including hormonal changes, gestational diabetes, and thyroid dysfunction, also play a significant role. Social factors like lack of social support, marital dissatisfaction, and stressful life events further elevate the risk of PPD (10).
Stressful conditions and elevated perceived stress levels significantly impact PPD prevalence. Perceived stress directly correlates with the intensity of neuroendocrine responses, triggering hormone secretion (11). Stressors during childhood, adolescence, and adulthood can elevate stress levels and activate the hypothalamic-pituitary-adrenal axis, leading to cortisol release (12). Perceived stress reflects an individual's subjective evaluation of demands and coping abilities. In pregnant women, concerns about pregnancy, childbirth, parenthood, financial pressures, relationship changes, lack of social support, and past trauma contribute to elevated perceived stress, significantly increasing the risk of PPD (13,14).
Marital satisfaction is a key factor in PPD development (15). Postpartum, approximately 80% of first-time mothers experience decreased marital satisfaction (16). The transition to parenthood affects interpersonal resources (17). Intimacy and relationship satisfaction enhance mood and coping abilities (18). Partner support buffers stress, aiding in navigating childbirth and parenting challenges (19). Marital quality depends on couples' adaptation, with decreased satisfaction in one partner affecting the other (16). Hudson et al. (20) showed that high levels of intimacy and satisfaction in a partnership lead to improved emotional well-being.
Research exploring the relationship between perceived stress, marital satisfaction, and PPD is essential for understanding and addressing this significant global mental health concern. While existing research has established links between these factors, important gaps remain. Primarily, most studies have focused on individual factors like perceived stress or PPD in isolation rather than examining their complex interplay within the marital dyad. Although research has shown that a decline in one partner's satisfaction significantly affects the other (16), the specific mechanisms through which marital satisfaction influences PPD development remain unclear. Secondly, the predominantly cross-sectional nature of previous research limits the ability to determine causality. Therefore, this study aims to investigate the direct and indirect effects of perceived stress on PPD, specifically examining the mediating role of marital satisfaction in this relationship. We hypothesize that higher levels of perceived stress will be significantly associated with an increased risk of PPD and that marital satisfaction will mediate the relationship between perceived stress and PPD.
Methods
This study employed a cross-sectional design using structural equation modeling (SEM) to examine the direct and indirect effects of perceived stress on PPD, with marital satisfaction as a proposed mediator. A conceptual model (Figure 1) guided the analysis. Participants were recruited using convenience sampling, a form of non-probability sampling, from various health centers in Ahvaz City, Iran. These health centers provide primary healthcare services to a diverse population in Ahvaz, a major city in southwestern Iran. The inclusion criteria were as follows: (1) women within six months postpartum; (2) women living with their husbands; (3) women whose childbirth resulted in a live birth; (4) women who provided informed consent to participate in the study; and (5) women who had completed at least a high school education. The exclusion criteria included women who experienced a major stressful life event (e.g., death of a close family member, serious accident, natural disaster) in the three months preceding data collection, as such events could significantly confound the assessment of perceived stress related to the postpartum period.
Data collection took place from March to June 2023. Trained research assistants approached eligible women visiting the participating health centers and explained the study's purpose and procedures. Women who agreed to participate provided written informed consent before completing the questionnaires. The questionnaires were self-administered, and research assistants were available to answer participants' questions. The sample size of 319 was determined using G*Power software (21). A power analysis was conducted to detect a medium effect size (f² = 0.15) with a power of 0.80 (1 - β), an alpha level of 0.05, and an estimated attrition rate of 10%. This resulted in a required sample size of approximately 290 participants. To account for the estimated attrition rate, we aimed to recruit 319 participants.
Demographic Information Form: A researcher-designed form was used to gather demographic information from participants. This form included items related to age, education level, infant gender, and employment status.
Edinburgh Postnatal Depression Scale (EPDS)
The Edinburgh Postnatal Depression Scale (EPDS), developed by Cox et al. (22), is a 10-item self-report questionnaire designed to assess depressive symptoms in postpartum women. Each item is rated on a four-point Likert scale ranging from 0 to 3, where 0 indicates the absence of the symptom, and 3 represents the most severe manifestation of the symptom. The specific response options for each item vary depending on the question. However, they generally reflect the increasing severity of the symptom (e.g., "Not at all," "Sometimes," "Quite often," "Very often"). The total EPDS score is calculated by summing the scores of all 10 items, resulting in a possible score range of 0 to 30. Higher scores indicate greater depressive symptom severity. The scale has demonstrated good reliability and validity in various studies, with a Cronbach's alpha of 0.83 reported by Mazhari and Nakhaee (23). In the present study, the internal consistency of the EPDS was found to be satisfactory, with a Cronbach's alpha of 0.79.
The Perceived Stress Scale (PSS)
The Perceived Stress Scale (PSS), developed by Cohen et al. (24), is a widely used 14-item self-report instrument designed to measure an individual's perception of stress during the past month. Participants rate each item on a 5-point Likert scale ranging from 0 ("Never") to 4 ("Very Often"), reflecting how often they felt or thought a certain way. The response options are: 0 = Never, 1 = Almost Never, 2 = Sometimes, 3 = Fairly Often, and 4 = Very Often. The total PSS score is calculated by summing the scores of the 14 items. Items 4, 5, 7, and 8 are reverse-scored before calculating the total score. This means that for these items, a response of 0 is recoded as 4, 1 as 3, 2 remains as 2, 3 as 1, and 4 as 0. The total PSS score can range from 0 to 56, with higher scores indicating greater perceived stress. The PSS has demonstrated robust psychometric properties across diverse populations. Cohen et al. (24) reported good internal consistency (Cronbach's alpha ranging from 0.84 to 0.86) and test-retest reliability. Subsequent studies have further supported the PSS's validity and reliability. For instance, Khalili et al. (25) reported a Cronbach's alpha coefficient of 0.72. In the present study, the internal consistency of the PSS was found to be satisfactory, with a Cronbach's alpha of 0.75.
The Marital Satisfaction Scale (MSS)
The Marital Satisfaction Scale (MSS) is a 35-item self-report measure designed to assess various aspects of marital quality, including satisfaction, communication, and conflict resolution. Participants respond to each item using a 5-point Likert scale ranging from 1 ("Strongly Disagree") to 5 ("Strongly Agree"). The response options are: 1 = Strongly Disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, and 5 = Strongly Agree. The total MSS score is calculated by summing the scores of all 35 items, resulting in a possible score range of 35 to 175. Higher scores indicate greater marital satisfaction. While the ENRICH MSS is a more comprehensive measure, evaluating a broader range of marital domains such as personality traits and financial management (26), the MSS provides a focused assessment of core marital satisfaction components. The Persian version of the MSS has demonstrated acceptable reliability. Arab Alidousti et al. (27) reported a Cronbach's alpha coefficient of 0.74. In the present study, the internal consistency of the MSS was found to be satisfactory, with a Cronbach's alpha of 0.77.
Data analysis
Data were screened for quality and adherence to SEM assumptions, including assessments of missing data, outliers, and normality. Subsequent analyses were performed using IBM SPSS Statistics (version 26) and IBM SPSS Amos (version 26). Descriptive statistics (Frequencies and percentages for categorical variables; means and standard deviations for continuous variables) were calculated for all demographic variables. SEM was then employed to test the hypothesized direct and indirect relationships among the latent variables (Perceived stress, marital satisfaction, and PPD) and to evaluate the overall model fit. The following fit indices were examined: chi-square (χ²), Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Incremental Fit Index (IFI), Relative Fit Index (RFI), Normed Fit Index (NFI), and Root Mean Square Error of Approximation (RMSEA). Acceptable model fit was defined as CFI and TLI values greater than 0.90 (ideally > 0.95), IFI values greater than 0.90 (ideally > 0.95), RFI and NFI values greater than 0.90, and RMSEA values less than 0.08 (ideally < 0.06). Direct and indirect effects were estimated using maximum likelihood estimation. Bootstrapping with 5000 resamples was used to assess the mediating role of marital satisfaction and to obtain 95% confidence intervals for indirect effects. All statistical tests were conducted using a significance level of α = 0.05.
Results
This study involved 319 postpartum women aged 20-35 years. Regarding employment status, 88 participants (27.59%) were employed outside the home, and 231 (72.41%) were homemakers. Among the study participants, 195 individuals (61.13%) reported completing high school as their highest level of education, while 124 participants (38.87%) had attained a university degree. The sample was balanced regarding infant gender, with 156 (48.28%) having a baby girl and 165 (51.72%) having a baby boy.
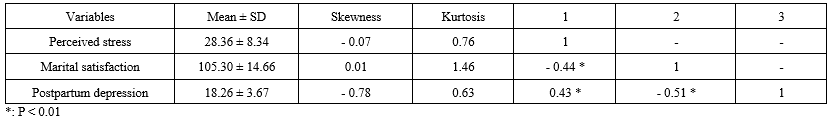
Descriptive statistics, including means, standard deviations, skewness, and kurtosis, are presented in Table 1. The mean scores for perceived stress, marital satisfaction, and PPD were 28.36, 105.30, and 18.26, respectively. The data for all variables were normally distributed, as indicated by skewness and kurtosis values within acceptable limits. Pearson correlation analysis revealed significant negative relationships between perceived stress and marital satisfaction (r = -0.44, P < 0.001) and between marital satisfaction and PPD (r = -0.51, P < 0.001). A significant positive relationship was found between perceived stress and PPD (r = 0.43, P < 0.001) (Table 1).
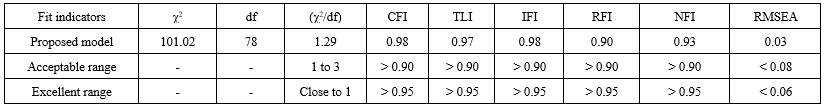
SEM was employed to evaluate the proposed model, which examined the relationships between perceived stress, marital satisfaction, and PPD. The model posited PPD as the outcome variable, perceived stress as the predictor variable, and marital satisfaction as a mediating variable. The model fit indices, including the CFI, TLI, and RMSEA, indicated a satisfactory fit between the model and the data (Table 2), as illustrated in Figure 2. The model suggests that higher perceived stress is associated with lower marital satisfaction and higher PPD, while higher marital satisfaction is associated with lower PPD.
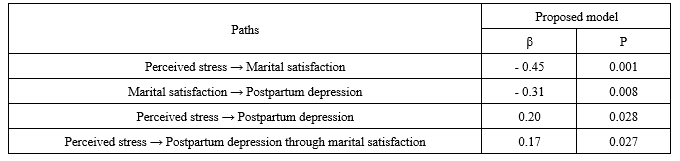
Table 3 presents the standardized path coefficients and significance levels for the direct and indirect effects within the proposed model. A significant negative direct effect was observed between perceived stress and marital satisfaction (β = -0.45, P < 0.001), indicating that as perceived stress increases, marital satisfaction decreases. Additionally, a significant negative direct effect was found between marital satisfaction and PPD (β = -0.31, P = 0.008), suggesting that higher levels of marital satisfaction are associated with lower levels of PPD. Furthermore, a significant positive direct effect was identified between perceived stress and PPD (β = 0.20, P = 0.028), indicating that increased perceived stress is linked to higher levels of PPD. Finally, a significant indirect effect of perceived stress on PPD through marital satisfaction was observed (β = 0.17, P = 0.027), suggesting that perceived stress indirectly influences PPD by negatively impacting marital satisfaction.
Demographic Information Form: A researcher-designed form was used to gather demographic information from participants. This form included items related to age, education level, infant gender, and employment status.
Edinburgh Postnatal Depression Scale (EPDS)
The Edinburgh Postnatal Depression Scale (EPDS), developed by Cox et al. (22), is a 10-item self-report questionnaire designed to assess depressive symptoms in postpartum women. Each item is rated on a four-point Likert scale ranging from 0 to 3, where 0 indicates the absence of the symptom, and 3 represents the most severe manifestation of the symptom. The specific response options for each item vary depending on the question. However, they generally reflect the increasing severity of the symptom (e.g., "Not at all," "Sometimes," "Quite often," "Very often"). The total EPDS score is calculated by summing the scores of all 10 items, resulting in a possible score range of 0 to 30. Higher scores indicate greater depressive symptom severity. The scale has demonstrated good reliability and validity in various studies, with a Cronbach's alpha of 0.83 reported by Mazhari and Nakhaee (23). In the present study, the internal consistency of the EPDS was found to be satisfactory, with a Cronbach's alpha of 0.79.
The Perceived Stress Scale (PSS)
The Perceived Stress Scale (PSS), developed by Cohen et al. (24), is a widely used 14-item self-report instrument designed to measure an individual's perception of stress during the past month. Participants rate each item on a 5-point Likert scale ranging from 0 ("Never") to 4 ("Very Often"), reflecting how often they felt or thought a certain way. The response options are: 0 = Never, 1 = Almost Never, 2 = Sometimes, 3 = Fairly Often, and 4 = Very Often. The total PSS score is calculated by summing the scores of the 14 items. Items 4, 5, 7, and 8 are reverse-scored before calculating the total score. This means that for these items, a response of 0 is recoded as 4, 1 as 3, 2 remains as 2, 3 as 1, and 4 as 0. The total PSS score can range from 0 to 56, with higher scores indicating greater perceived stress. The PSS has demonstrated robust psychometric properties across diverse populations. Cohen et al. (24) reported good internal consistency (Cronbach's alpha ranging from 0.84 to 0.86) and test-retest reliability. Subsequent studies have further supported the PSS's validity and reliability. For instance, Khalili et al. (25) reported a Cronbach's alpha coefficient of 0.72. In the present study, the internal consistency of the PSS was found to be satisfactory, with a Cronbach's alpha of 0.75.
The Marital Satisfaction Scale (MSS)
The Marital Satisfaction Scale (MSS) is a 35-item self-report measure designed to assess various aspects of marital quality, including satisfaction, communication, and conflict resolution. Participants respond to each item using a 5-point Likert scale ranging from 1 ("Strongly Disagree") to 5 ("Strongly Agree"). The response options are: 1 = Strongly Disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, and 5 = Strongly Agree. The total MSS score is calculated by summing the scores of all 35 items, resulting in a possible score range of 35 to 175. Higher scores indicate greater marital satisfaction. While the ENRICH MSS is a more comprehensive measure, evaluating a broader range of marital domains such as personality traits and financial management (26), the MSS provides a focused assessment of core marital satisfaction components. The Persian version of the MSS has demonstrated acceptable reliability. Arab Alidousti et al. (27) reported a Cronbach's alpha coefficient of 0.74. In the present study, the internal consistency of the MSS was found to be satisfactory, with a Cronbach's alpha of 0.77.
Data analysis
Data were screened for quality and adherence to SEM assumptions, including assessments of missing data, outliers, and normality. Subsequent analyses were performed using IBM SPSS Statistics (version 26) and IBM SPSS Amos (version 26). Descriptive statistics (Frequencies and percentages for categorical variables; means and standard deviations for continuous variables) were calculated for all demographic variables. SEM was then employed to test the hypothesized direct and indirect relationships among the latent variables (Perceived stress, marital satisfaction, and PPD) and to evaluate the overall model fit. The following fit indices were examined: chi-square (χ²), Comparative Fit Index (CFI), Tucker-Lewis Index (TLI), Incremental Fit Index (IFI), Relative Fit Index (RFI), Normed Fit Index (NFI), and Root Mean Square Error of Approximation (RMSEA). Acceptable model fit was defined as CFI and TLI values greater than 0.90 (ideally > 0.95), IFI values greater than 0.90 (ideally > 0.95), RFI and NFI values greater than 0.90, and RMSEA values less than 0.08 (ideally < 0.06). Direct and indirect effects were estimated using maximum likelihood estimation. Bootstrapping with 5000 resamples was used to assess the mediating role of marital satisfaction and to obtain 95% confidence intervals for indirect effects. All statistical tests were conducted using a significance level of α = 0.05.
Results
This study involved 319 postpartum women aged 20-35 years. Regarding employment status, 88 participants (27.59%) were employed outside the home, and 231 (72.41%) were homemakers. Among the study participants, 195 individuals (61.13%) reported completing high school as their highest level of education, while 124 participants (38.87%) had attained a university degree. The sample was balanced regarding infant gender, with 156 (48.28%) having a baby girl and 165 (51.72%) having a baby boy.
Descriptive statistics, including means, standard deviations, skewness, and kurtosis, are presented in Table 1. The mean scores for perceived stress, marital satisfaction, and PPD were 28.36, 105.30, and 18.26, respectively. The data for all variables were normally distributed, as indicated by skewness and kurtosis values within acceptable limits. Pearson correlation analysis revealed significant negative relationships between perceived stress and marital satisfaction (r = -0.44, P < 0.001) and between marital satisfaction and PPD (r = -0.51, P < 0.001). A significant positive relationship was found between perceived stress and PPD (r = 0.43, P < 0.001) (Table 1).
SEM was employed to evaluate the proposed model, which examined the relationships between perceived stress, marital satisfaction, and PPD. The model posited PPD as the outcome variable, perceived stress as the predictor variable, and marital satisfaction as a mediating variable. The model fit indices, including the CFI, TLI, and RMSEA, indicated a satisfactory fit between the model and the data (Table 2), as illustrated in Figure 2. The model suggests that higher perceived stress is associated with lower marital satisfaction and higher PPD, while higher marital satisfaction is associated with lower PPD.
Table 3 presents the standardized path coefficients and significance levels for the direct and indirect effects within the proposed model. A significant negative direct effect was observed between perceived stress and marital satisfaction (β = -0.45, P < 0.001), indicating that as perceived stress increases, marital satisfaction decreases. Additionally, a significant negative direct effect was found between marital satisfaction and PPD (β = -0.31, P = 0.008), suggesting that higher levels of marital satisfaction are associated with lower levels of PPD. Furthermore, a significant positive direct effect was identified between perceived stress and PPD (β = 0.20, P = 0.028), indicating that increased perceived stress is linked to higher levels of PPD. Finally, a significant indirect effect of perceived stress on PPD through marital satisfaction was observed (β = 0.17, P = 0.027), suggesting that perceived stress indirectly influences PPD by negatively impacting marital satisfaction.
Discussion
This study investigated the intricate relationship between perceived stress, marital satisfaction, and PPD among postpartum women, specifically focusing on the mediating role of marital satisfaction. The findings revealed significant associations, shedding light on the complex interplay of these factors during the transition to motherhood.
Consistent with previous research (28), a significant negative correlation was observed between perceived stress and marital satisfaction. As perceived stress increased, marital satisfaction decreased. This suggests that the stressors inherent in the pre- and postpartum periods can significantly erode marital quality. Factors such as disagreements regarding the child's gender, unintended pregnancies, conflicts with extended family, parenting stress, and hormonal fluctuations likely contribute to this decline. The assumption of maternal caregiving responsibilities can lead to caregiving stress and self-doubt. At the same time, discrepancies between expected and actual parental roles and spousal differences can further strain marital satisfaction (15). Moreover, the physiological, psychological, and social changes associated with pregnancy can heighten anxiety and distress, negatively impacting marital harmony (18). This underscores the critical role of perceived stress as a significant risk factor for diminished marital satisfaction.
Furthermore, a significant negative correlation was found between marital satisfaction and PPD, aligning with previous studies (29). Lower marital satisfaction was associated with increased PPD, highlighting the interconnectedness of partners' experiences during the transition to parenthood. This period often sees heightened marital conflict and dissatisfaction, particularly among first-time parents (30). Psychological disorders like depression or anxiety in either partner can exacerbate interpersonal conflict and negative emotions, further contributing to this association. The stressors mentioned earlier, including disagreements regarding the child's sex, unintended pregnancies, and parenting stress, can directly impact marital quality and satisfaction, ultimately influencing the risk of PPD.
The study also demonstrated a significant correlation between perceived stress and PPD, consistent with previous research (31,32). Stressful life events, parental stress, unintended pregnancy, and neonatal hospitalization were identified as contributing factors to PPD. The presence of various stressors, such as primiparity, childbirth complications, infant illness, and substance abuse, can lead to psychological distress and harm in mothers. Pregnancy itself is a significant life event requiring substantial adjustments, and the social and economic burden of unplanned pregnancies can exacerbate stress and psychological distress (31).
Crucially, the analysis of indirect effects revealed that perceived stress can influence PPD through the mediating role of marital satisfaction. Elevated perceived stress negatively impacts marital satisfaction, which in turn increases PPD. This aligns with prior research (33), indicating that stress can lead to decreased marital satisfaction, increased conflict, and subsequent PPD. Unchecked perceived stress, stemming from factors like the transition to parenthood, infant temperament incompatibility, and feelings of parental inadequacy, can become chronic and prolonged. The psychological burden imposed by psychosocial stressors during and after pregnancy can significantly contribute to PPD (33).
The demands of motherhood present a unique set of stressors, often evolving into long-term parenting-related challenges. Breastfeeding can be time-consuming, and inadequate infant care can exacerbate interparental conflict, increasing the risk of PPD (34). The multitude of changes accompanying pregnancy and the postpartum period can lead to heightened worry, anxiety, and distress, impacting marital satisfaction. As hypothesized, elevated perceived stress, coupled with diminished marital satisfaction, creates a context conducive to the development of PPD in mothers. This study underscores the importance of addressing perceived stress and marital satisfaction in interventions to prevent and mitigate PPD. Future research should explore how these factors interact and evaluate the effectiveness of targeted interventions to support postpartum women and their families.
This study has several notable strengths. The relatively large sample size enhances statistical power and the generalizability of the findings to similar populations. The use of validated instruments, including the EPDS and PSS, strengthens the reliability and validity of the measurements. Furthermore, applying structural equation modeling allowed for examining complex relationships among multiple variables, including the mediating role of marital satisfaction. This study contributes to the literature by providing empirical evidence for this mediation, a relationship that has not been extensively explored in this population.
However, several limitations should be acknowledged. Using a convenience sampling method limits the generalizability of the findings to other populations. The cross-sectional design of this study precludes definitive conclusions about causality. Longitudinal studies are needed to establish the temporal ordering of the observed relationships. The reliance on self-report measures may have introduced response bias. Finally, the sample consisted of postpartum women in Ahvaz, Iran, which may limit the generalizability of the findings to women in other cultural contexts.
Conclusion
This study confirms that perceived stress and marital satisfaction are crucial predictors of PPD. As predicted, high perceived stress reduces marital satisfaction, which in turn elevates the risk of PPD, illustrating an indirect pathway. Direct links between perceived stress and PPD and marital satisfaction and PPD emphasize the complex nature of PPD's development. These findings highlight the need for interventions addressing both perceived stress and marital satisfaction to prevent and mitigate PPD. Cognitive behavioral therapy can effectively reduce stress and improve coping. Couple-based therapies, like Emotionally Focused Therapy, can enhance marital communication and intimacy. Future research should explore the specific cognitive and behavioral processes mediating these relationships and use longitudinal studies to identify optimal intervention times. A deeper understanding will enable clinicians, particularly midwives and family nurses, to provide more effective support for the mental health of postpartum women.
Acknowledgement
The authors express their sincere gratitude to the women who generously participated in this research by completing the questionnaires.
Funding sources
No financial support was received for this article.
Ethical statement
All ethical principles in human research, in accordance with the Helsinki Declaration, were adhered to, including written informed consent, the right to confidentiality and the protection of individual identities of participants, voluntary participation, and the right to withdraw from the study. The Ethics Review Board of the Islamic Azad University, Ahvaz Branch, approved the present study under the following reference number: IR.IAU.AHVAZ.REC.1402.028.
Conflicts of interest
There was no conflict of interest to be declared.
Author contributions
BM: Study concept and design, data acquisition, analysis and interpretation of data, and statistical analysis. SB: Administrative, technical, and material support, study supervision. FN and ZDB: Critical revision of the manuscript for important intellectual content.
Type of study: Original Article |
Subject:
Midwifery
References
1. Hematian MN, Ghiasi M, Baharian S, Safaie S, Rahmanian M, Torabi S, et al. Reviewing the Anxiety in Pregnant Mothers with Fetuses Having Positive Cardiac Anomaly and Its Relation with Birth Outcomes. Journal of Obstetrics, Gynecology and Cancer Research. 2021;7(1):7-14. [View at Publisher] [DOI] [Google Scholar]
2. Alshikh Ahmad H, Alkhatib A, Luo J. Prevalence and risk factors of postpartum depression in the Middle East: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2021;21(1):542. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Kamkar M-Z, balajalini A, Zargarani F, Behnampour N. Postpartum Depression in Women with Normal Delivery and Cesarean Section Referring to Sayad Shirazi Hospital of Gorgan, Iran. J Res Dev Nurs Midw. 2019;16(1):51-8. [View at Publisher] [DOI] [Google Scholar]
4. Amer SA, Zaitoun NA, Abdelsalam HA, Abbas A, Ramadan MS, Ayal HM, et al. Exploring predictors and prevalence of postpartum depression among mothers: Multinational study. BMC Public Health. 2024;24(1):1308. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Alimoradi B, Nejat H. Early Maladaptive schemas and Premenstrual syndrome in mothers with postpartum depression. Preventive Care in Nursing and Midwifery Journal. 2018;8(1):43-8. [View at Publisher] [DOI] [Google Scholar]
6. Zhang Y, Liu X, Liu M, Li M, Chen P, Yan G, et al. Multidimensional influencing factors of postpartum depression based on the perspective of the entire reproductive cycle: evidence from western province of China. Soc Psychiatry Psychiatr Epidemiol. 2024;59(11):2041-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Özcan NK, Boyacıoğlu NE, Dinç H. Postpartum Depression Prevalence and Risk Factors in Turkey: A Systematic Review and Meta-Analysis. Arch Psychiatr Nurs. 2017;31(4):420-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Zhang S, Wang L, Yang T, Chen L, Qiu X, Wang T, et al. Maternal violence experiences and risk of postpartum depression: A meta-analysis of cohort studies. Eur Psychiatry. 2019;55:90-101. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Ďuríčeková B, Škodová Z, Bašková M. Risk factors associated with postpartum depression and PTSD after birth in a sample of Slovak women. Heliyon. 2023;10(1):e23560. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Wang D, Li YL, Qiu D, Xiao SY. Factors Influencing Paternal Postpartum Depression: A Systematic Review and Meta-Analysis. J Affect Disord. 2021;293:51-63. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Lee MS, Lee JJ, Park S, Kim S, Lee H. Is social support associated with postpartum depression, anxiety and perceived stress among Korean women within the first year postpartum? J Psychosom Obstet Gynaecol. 2023;44(1):2231629. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Murphy F, Nasa A, Cullinane D, Raajakesary K, Gazzaz A, Sooknarine V, et al. Childhood Trauma, the HPA Axis and Psychiatric Illnesses: A Targeted Literature Synthesis. Front Psychiatry. 2022;13:748372. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Lee MS, Lee JJ, Park S, Kim S, Lee H. Is social support associated with postpartum depression, anxiety and perceived stress among Korean women within the first year postpartum? Journal of Psychosomatic Obstetrics & Gynecology. 2023;44(1):2231629. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Yaqoob H, Ju X-D, Bibi M, Anwar S, Naz S. A systematic review of risk factors of postpartum depression. Evidence from Asian culture. Acta Psychol. 2024;249:104436. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Odinka JI, Nwoke M, Chukwuorji JC, Egbuagu K, Mefoh P, Odinka PC, et al. Post-partum depression, anxiety and marital satisfaction: A perspective from Southeastern Nigeria. S Afr J Psychiatr. 2018;24:1109. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Bogdan I, Turliuc MN, Candel OS. Transition to Parenthood and Marital Satisfaction: A Meta-Analysis. Front Psychol. 2022;13:901362. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Rauch-Anderegg V, Kuhn R, Milek A, Halford W, Bodenmann G. Relationship Behaviors across the Transition to Parenthood. Journal of Family Issues. 2019;41(4):483-506. [View at Publisher] [DOI] [Google Scholar]
18. Rashidi Fakari F, Doulabi MA, Mahmoodi Z. Predict marital satisfaction based on the variables of socioeconomic status (SES) and social support, mediated by mental health, in women of reproductive age: Path analysis model. Brain Behav. 2022;12(3):e2482. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Perry N, Johnson A, Hostinar C, Gunnar M. Parental emotional support and social buffering in previously institutionalized and typically developing children and adolescents. Dev Psychobiol. 2021;63(5):1167-76. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Hudson NW, Lucas RE, Donnellan MB. Are we happier with others? An investigation of the links between spending time with others and subjective well-being. J Pers Soc Psychol. 2020;119(3):672-94. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175-91. [View at Publisher] [DOI] [PMID] [Google Scholar]
22. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
23. Mazhari S, Nakhaee N. Validation of the Edinburgh Postnatal Depression Scale in an Iranian sample. Arch Womens Ment Health. 2007;10(6):293-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
24. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385-396. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Khalili R, Sirati Nir M, Ebadi A, Tavallai A, Habibi M. Validity and reliability of the Cohen 10-item Perceived Stress Scale in patients with chronic headache: Persian version. Asian J Psychiatr. 2017;26:136-140. [View at Publisher] [DOI] [PMID] [Google Scholar]
26. Olson DH, Fournier DG, Druckman JM. Counselor's manual for Prepare//Enrich (Rev. ed). Minneapolis. 1987. [View at Publisher] [Google Scholar]
27. Arab Alidousti A, Nakhaee N, Khanjani N. Reliability and Validity of the Persian versions of the ENRICH Marital Satisfaction (Brief version) and Kansas Marital Satisfaction Scales. Health and Development Journal. 2015;4(2):158-67. [View at Publisher] [Google Scholar]
28. Rabipoor S, Abedi M. Perceived Stress and Prenatal Distress during Pregnancy and its Related Factors. J Res Dev Nurs Midw. 2020;17(1):67-80. [View at Publisher] [DOI] [Google Scholar]
29. Kiani F, Khadivzadeh T, Sargolzaee MR, Behnam H. Relationship between Marital Satisfaction during Pregnancy and Postpartum Depression (PPD). The Iranian Journal of Obstetrics, Gynecology and Infertility. 2010;13(5):37-44. [View at Publisher] [DOI] [Google Scholar]
30. Qi W, Liu Y, Lv H, Ge J, Meng Y, Zhao N, et al. Effects of family relationship and social support on the mental health of Chinese postpartum women. BMC Pregnancy Childbirth. 2022;22(1):65. [View at Publisher] [DOI] [PMID] [Google Scholar]
31. Tasnim F, Abedin S, Rahman MM. Mediating role of perceived stress on the association between domestic violence and postpartum depression: cross-sectional study in Bangladesh. BJPsych Open. 2023;9(1):e16. [View at Publisher] [DOI] [PMID] [Google Scholar]
32. Leonard KS, Evans MB, Kjerulff KH, Symons Downs D. Postpartum Perceived Stress Explains the Association between Perceived Social Support and Depressive Symptoms. Women's Health Issues. 2020;30(4):231-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
33. Yoo H, Ahn S, Park S, Kim J, Oh J, Koh M. Factors influencing prenatal and postpartum depression in Korea: a prospective cohort study. Korean J Women Health Nurs. 2021;27(4):326-36. [View at Publisher] [DOI] [PMID] [Google Scholar]
34. Pope CJ, Mazmanian D. Breastfeeding and Postpartum Depression: An Overview and Methodological Recommendations for Future Research. Depress Res Treat. 2016;2016:4765310. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |