Volume 21, Issue 4 (12-2024)
J Res Dev Nurs Midw 2024, 21(4): 19-23 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Tahmasbi F, Yazdi K, Sadat Seyedghasemi N, Kolagari S. The relationship between informatics competency and clinical competency in nurses working in intensive care units: A Cross-sectional Study in Northeast Iran. J Res Dev Nurs Midw 2024; 21 (4) :19-23
URL: http://nmj.goums.ac.ir/article-1-1733-en.html
URL: http://nmj.goums.ac.ir/article-1-1733-en.html
1- School of Nursing and Midwifery, Golestan University of Medical Sciences, Gorgan, Iran
2- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3- School of Health, Golestan University of Medical Sciences, Gorgan, Iran
4- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,dr.kolagari@goums.ac.ir
2- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran
3- School of Health, Golestan University of Medical Sciences, Gorgan, Iran
4- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,
Full-Text [PDF 531 kb]
(694 Downloads)
| Abstract (HTML) (1672 Views)
Discussion
In this study, the distribution of the scores of the informatics and clinical competency variables and their subscales was optimal, but there was no statistical relationship between the two variables of informatics nursing competency and clinical nursing competency. In addition, among the demographic variables, only work experience showed a statistically significant relationship with clinical competency, while gender and interaction with HIS showed a statistically significant difference with informatics competency.
In the present study, there was no statistically significant uniform relationship between the nurses’ clinical competency and informatics competency. On the contrary, Ansari Jaberi et al.’s (16) research confirmed the correlation between nurses’ informatics competency and professional-clinical competency. Jung et al.’s (25) research also indicated a positive and strong relationship between nurses’ informatics competency and clinical performance, which is not in line with the results of the current study.
In investigating the concurrency of explanatory variables with the clinical competency of nurses, only the work experience variable showed a statistically significant difference. This finding is in line with Elhami et al.’s (26) study but not with studies conducted by Faraji et al. (27) and Mirlashari et al. (28).
The study findings demonstrated that the mean score of clinical competencies in the nurses was reported to be favorable, which is consistent with Qorbanzadeh et al. (29), who also reported a favorable mean score of clinical competencies among nurses. Other studies, such as those by Fotouhi et al. (30), Zakeri et al. (31), and Sasaki et al. (32), similarly indicated a favorable mean score of competencies among nurses. On the other hand, the clinical competency score was reported to be at an excellent level in Kolagari et al.’s (33) study and at an average level in Karami et al.’s (34) study. In Ghonem et al.’s (35) study, the mean competency scores on the total scale and in various dimensions were poor. It seems that differences in the correct distribution of clinical nursing forces, the continuous evaluation of clinical competencies, the implementation of educational programs to improve clinical competency, and variations in setting facilities are among the contributing factors.
Among the clinical competency dimensions, the highest mean belonged to the attitude and value dimension, and the lowest to the experience dimension. In line with the present study, Ghahrisarabi et al. (18) also reported the highest mean score for the attitude and value dimension and the lowest for the knowledge dimension, whereas in Kolagari et al.’s (33) study, the highest and lowest mean scores were observed in the knowledge and skill dimensions, respectively. It can be acknowledged that the attitude and value dimension of most nurses working in clinical settings is equally influenced by their discipline, lessons learned, and the knowledge upon which they base their care for patients at the bedside. The difference in clinical competency scores among the dimensions highlights the gap between theory and clinical practice. Nurses need more experience and skill to achieve competency, while knowledge and awareness serve as predisposing factors.
The results of the present study also demonstrated that the mean score of informatics competency was generally favorable, which is consistent with the findings of Ansari Jaberi et al.’s (16) research, showing favorable informatics competency scores among participants. Farokhzadian et al. (6) and Jung et al. also reported that participants’ mean IT competency scores were at a favorable level, aligning with the present study findings. On the contrary, Batran et al.’s (36) study revealed that participants’ mean informatics competency scores were not favorable. In this study, the highest and lowest mean scores of informatics competency were in the informatics skills and informatics knowledge dimensions, respectively. Similarly, Kleib et al.’s (9) study indicated that participants’ self-reported mean score for informatics skills was optimal, whereas in Khezri et al.’s (37) research, basic computer skills had the highest mean score among participants. Differences in the level of informatics competency among nurses and its components across various studies may stem from the health system’s emphasis on IT and its role in advancing medical science professions, including nursing.
In investigating the concurrency of explanatory variables with nurses’ informatics competency, only the interaction with HIS and gender variables showed a statistically significant difference. Regarding HIS, it was observed that increased interaction with HIS was associated with reduced informatics competency. Consistent with the findings of the current research, Khezri et al.’s (37) study demonstrated an inverse correlation between informatics competency scores and the amount of time spent interacting with the hospital’s HIS, indicating that greater time spent with HIS led to reduced informatics competency. However, studies by Kinnunen et al. (38), Farzandipour et al. (8), and Karim et al. (39) found no statistically significant difference between nurses’ informatics competency and interaction with HIS. It may be suggested that the HIS variable is not contradictory to the components of informatics competency and that working with HIS may not significantly influence these competency components.
Regarding the gender variable, the results revealed a statistically significant difference between the participants’ informatics competency and gender. On the contrary, the findings of Al-Hawamdih et al.’s (40) study indicated no statistically significant difference between participants’ informatics competency and gender.
This study also had several limitations that should be considered when interpreting the data, including the complexity of ICU conditions compared to other hospital wards, the lack of sufficient time to complete the questionnaires, and the use of self-report questionnaires for data collection.
Conclusion
The findings showed that although the overall scores of informatics competency and clinical competence among the nurses were appropriate, there was no significant relationship or difference between the two variables. It seems that the importance of informatics competency, as one of the new dimensions of competence in the clinical setting, is still in its early stages, and more knowledge about it is needed. Therefore, it is recommended to emphasize the necessity of nurses’ skills and competence in the field of technology within the clinical setting. In addition, nurses should be motivated to improve professionally and acquire competency in new approaches by gaining updated knowledge.
Acknowledgement
This article has been extracted from a master’s thesis in intensive care nursing, supported by Golestan University of Medical Sciences. The researchers would like to thank the Research and Technology Department of Golestan University of Medical Sciences, as well as the dedicated and selfless nurses who assisted us despite their busy schedules.
Funding sources
This study was supported by the Deputy of Research and Technology at Golestan University of Medical Sciences.
Ethical statement
The present study was approved by the Ethics Committee of Golestan University of Medical Sciences, Gorgan, Iran (Code: IR.GOUMS.REC.1402.325). Written informed consent was obtained from the nurses participating in this research. In addition, the right to withdraw from the study and maintain the confidentiality of the data was ensured.
Conflicts of interest
None.
Author contributions
ShK designed the study, FT collected the data, and NGH analyzed and interpreted the data. ShK and KhY were major contributors to writing the manuscript. All authors read and approved the final manuscript.
Full-Text: (546 Views)
Introduction
At the beginning of the third millennium, information technology (IT), as the most important axis of transformation in the world, is considered, and in recent decades, it has also been welcomed in the health system (1). Due to the rapid growth of technology, informatics needs to further adapt to the needs of the health system (2).
According to Janson, by transforming data into required information, the influence of informatics leads to improved justice, safety, and quality in clinical nursing care (3). By using informatics skills and integrating them into clinical activities, nurses, as the most extensive care group in the health system, have gained new opportunities to help improve patient status (4). The World Health Organization (WHO) has regarded the use of informatics by nurses as a practical approach to reinforce nursing services and significantly improve health outcomes (5). The influence of informatics in nursing has culminated in nurses’ participation in implementing IT in clinical care (6). Nursing informatics organizations, such as the Australian Nursing Informatics Association, the Nursing Informatics Group in Brazil, the Nursing Professionals Group and the Computer Society in Britain, and the Switzerland Nursing Informatics, have also emphasized the use of technology and computers in nursing care provision (7). Nursing informatics is regarded as one of the principal professional competencies among nurses worldwide (8), and acquiring competencies in basic computer skills and informatics knowledge and skills elevates nurses’ clinical capabilities (9).
Nursing informatics competency is an acceptable level of knowledge, skill, and ability to perform specific informatics tasks and is an important ability of nurses (10).
The results of Farokhzadian et al.’s research (6) demonstrated that the highest nursing informatics competency was in the area of basic computer knowledge, while the lowest was in informatics skills (6). The findings of Kaihlanen et al.’s study also revealed that nurses’ mean scores of informatics competency were at a desirable level (11). Emphasizing that nurses work in complex settings where technology and functioning are constantly changing, more competencies are thus required to ensure that high-quality care is provided at the bedside (12,13).
Nursing clinical competency, by benefiting from knowledge, skills, experiences, attitudes, and values, as the ultimate goal of nursing education, focuses on the ability to apply nursing knowledge, communication and interpersonal skills, problem-solving, and advanced decision-making skills. Nurses’ awareness of their clinical competency status assists in maintaining care standards and encourages them to rethink and play a more active role in patient care (14). The use of informatics in nursing can accelerate the provision of clinical care (15). It also improves the quality of care and patient safety, reduces costs, facilitates information exchange between nurses and clients, and improves interpersonal relationships. In addition, it helps reinforce evidence-based performance, clinical decision-making, and achieving favorable results in nursing (16), particularly among nurses in intensive care units (ICUs), who require more competencies in providing services and caring for patients, in addition to higher vigilance (17). The results of Ghahrisarabi et al.’s study indicated that the clinical competency of ICU nurses was excellent (18).
In addition, the importance of nurses’ clinical competency in the patient recovery process (19) and providing safe and effective care in the clinical setting (19,20), as well as nurses’ informatics competency (17), can enhance organizational effectiveness by reducing costs, improving standards in patient care (21), better identifying patients, improving patient outcomes, managing patient information, and increasing satisfaction with nurses’ daily activities. IT, including nursing information systems, also improves clinical care planning, access to nursing documents and their readability, reduces duplicate documentation, facilitates the completion of nursing documents and medical examinations, and helps optimize nurses’ workflow (22). On the contrary, settings will be inefficient in the absence of clinical and technological competencies (8).
Accordingly, competency evaluation is essential not only to ensure the receipt of quality care but also to identify areas for improvement and determine nurses’ training needs (23). Meanwhile, in critical care nursing, clinical nurses are often unaware of new concepts that have entered the nursing literature. Due to a lack of knowledge and understanding, they continue to use only outdated nursing concepts. In fact, clinical nurses need to familiarize themselves with new concepts in nursing, understand their interrelationships, and strive to acquire the necessary competencies to improve the quality of nursing care.
Despite extensive research on these two concepts in other countries, few studies have been conducted in our country in this regard. Considering the role of nurses in providing high-quality care and the significance of applying IT to advance care goals, the present study aimed to determine the relationship between informatics competency and clinical competency in nurses working in ICUs.
Methods
Study design
The present cross-sectional research was conducted on 135 nurses working in the ICUs at hospitals affiliated with Golestan University of Medical Sciences based on sampling and inclusion criteria. The sampling method was stratified with proportional allocation. To determine the sample size, Ansari Jaberi et al.’s (2022) study investigating the association between nurses’ informatics competency and professional competency was used (16). Given that in this study, the correlation coefficient between professional competency and informatics competency was estimated to be r = 0.3, the sample size was determined to be 113 people according to the following formula.

In the above formula, α, denoting Type I error, was considered to be 0.05, and β, denoting Type II error, was considered to be 0.1. Considering the non-inclusion criterion, the sample size was increased by approximately 20%, and the final sample size was estimated to be n = 135.
Study setting
The sampling method was stratified according to the number of nurses working in each hospital. Two hospitals were selected from Gorgan city (n = 57), two hospitals from Gonbad city (n = 37), and one hospital from each of the other seven cities in the province (n = 41).
Measurement tools
For data collection, three tools were used: a demographic form (Including age, gender, marital status, work experience in the ICU, education level, work experience, interaction with the hospital information system (HIS), informatics course, frequency of computer use, employment type, position, and ethnicity), the Intensive and Critical Care Nursing Competency Scale-1 (ICCN-CS-1), and the Nursing Informatics Competency Scale (NICS).
The ICCN-CS-1 was designed by Lakanmaa et al. in Finland and translated and culturally adapted by Shouryabi et al. (2017) at Shahid Beheshti University of Medical Sciences by performing face validity, content validity, and construct validity (24). This scale contains 80 statements in 4 dimensions: Knowledge (20 factors), skill (20 factors), attitude and value (20 factors), and experience (20 factors). Scoring was performed using a 5-point Likert scale ranging from very poor (1) to excellent (6). The range of the clinical competency score was from 80 to 400. Scores higher than the average denoted greater clinical competency. The scale’s reliability was reported by calculating the Cronbach’s alpha coefficient of α = 0.96 for the total scale and 0.93-0.96 for the dimensions.
In addition, the NICS was designed by Staggers et al. and translated and culturally adapted by Farzandipour et al. (2018) at Kashan University of Medical Sciences. This scale contained 38 statements in three dimensions: Computer skills (15 statements), informatics knowledge (13 statements), and informatics skills (10 statements). Scoring was performed using a 4-point Likert scale ranging from very low (1) to very high (5). Scores higher than the average denoted greater informatics competency. The range of the informatics competency score was from 38 to 152. The scale’s reliability was confirmed by an intraclass correlation coefficient (ICC) of 0.97 for the total scale and 0.95-0.99 for the dimensions (8).
With ethical approval code from the university’s Deputy of Research and Technology and according to the sampling framework, the researcher visited the ICU at hospitals affiliated with the university and explained the research objectives and information confidentiality to nurses meeting the inclusion criteria. After obtaining written consent, the researcher provided the questionnaires to them. Due to the conditions of some ICU nurses’ busy schedules and with prior coordination for entering the ICU, the nurses were given a week to ten days to fill out the questionnaires at their leisure.
The inclusion criteria for nurses included having at least a bachelor’s degree in nursing, having at least 6 months of work experience in the ICU, working in the ICU, current employment in the ICU, and willingness to participate in the research. The exclusion criterion included incomplete questionnaires (24).
Statistical methods
The data were then entered into SPSS version 21 (SPSS Inc., Chicago, IL, USA). Descriptive parameters such as mean, median, and standard deviation were used, and the Shapiro-Wilk test was applied to assess the normality of the data. Spearman's rank correlation coefficient, Mann-Whitney, and Kruskal-Wallis tests were used due to the non-normality of the data. Non-normal variables included clinical competency dimensions such as knowledge, skill, attitudes and values, experience, and total. Furthermore, multiple linear regression and generalized multiple linear regression models were used. The significance level of all statistical tests was set at 0.05. Standardized and unstandardized beta coefficients were estimated along with a 95% confidence interval.
Results
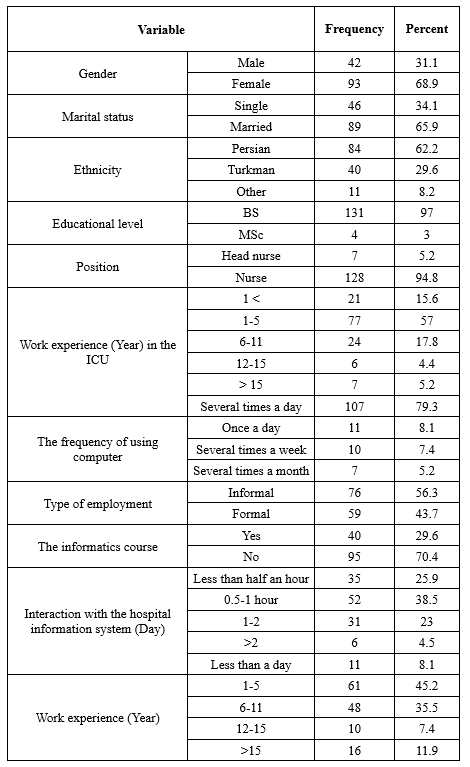
In the present study, 135 ICU nurses were included, with a mean age of 30.75 ± 5.91 years (Range: 20 to 48) and a median age of 30 years. The highest total mean score of clinical competencies in the nurses was 58.41 ± 8.80, with the lowest being 31.15 and the highest being 68.75, denoting a favorable competency. In addition, regarding the areas of clinical competency, the highest and lowest mean scores belonged to the dimensions of value and attitude and experience, respectively (Table 1).
At the beginning of the third millennium, information technology (IT), as the most important axis of transformation in the world, is considered, and in recent decades, it has also been welcomed in the health system (1). Due to the rapid growth of technology, informatics needs to further adapt to the needs of the health system (2).
According to Janson, by transforming data into required information, the influence of informatics leads to improved justice, safety, and quality in clinical nursing care (3). By using informatics skills and integrating them into clinical activities, nurses, as the most extensive care group in the health system, have gained new opportunities to help improve patient status (4). The World Health Organization (WHO) has regarded the use of informatics by nurses as a practical approach to reinforce nursing services and significantly improve health outcomes (5). The influence of informatics in nursing has culminated in nurses’ participation in implementing IT in clinical care (6). Nursing informatics organizations, such as the Australian Nursing Informatics Association, the Nursing Informatics Group in Brazil, the Nursing Professionals Group and the Computer Society in Britain, and the Switzerland Nursing Informatics, have also emphasized the use of technology and computers in nursing care provision (7). Nursing informatics is regarded as one of the principal professional competencies among nurses worldwide (8), and acquiring competencies in basic computer skills and informatics knowledge and skills elevates nurses’ clinical capabilities (9).
Nursing informatics competency is an acceptable level of knowledge, skill, and ability to perform specific informatics tasks and is an important ability of nurses (10).
The results of Farokhzadian et al.’s research (6) demonstrated that the highest nursing informatics competency was in the area of basic computer knowledge, while the lowest was in informatics skills (6). The findings of Kaihlanen et al.’s study also revealed that nurses’ mean scores of informatics competency were at a desirable level (11). Emphasizing that nurses work in complex settings where technology and functioning are constantly changing, more competencies are thus required to ensure that high-quality care is provided at the bedside (12,13).
Nursing clinical competency, by benefiting from knowledge, skills, experiences, attitudes, and values, as the ultimate goal of nursing education, focuses on the ability to apply nursing knowledge, communication and interpersonal skills, problem-solving, and advanced decision-making skills. Nurses’ awareness of their clinical competency status assists in maintaining care standards and encourages them to rethink and play a more active role in patient care (14). The use of informatics in nursing can accelerate the provision of clinical care (15). It also improves the quality of care and patient safety, reduces costs, facilitates information exchange between nurses and clients, and improves interpersonal relationships. In addition, it helps reinforce evidence-based performance, clinical decision-making, and achieving favorable results in nursing (16), particularly among nurses in intensive care units (ICUs), who require more competencies in providing services and caring for patients, in addition to higher vigilance (17). The results of Ghahrisarabi et al.’s study indicated that the clinical competency of ICU nurses was excellent (18).
In addition, the importance of nurses’ clinical competency in the patient recovery process (19) and providing safe and effective care in the clinical setting (19,20), as well as nurses’ informatics competency (17), can enhance organizational effectiveness by reducing costs, improving standards in patient care (21), better identifying patients, improving patient outcomes, managing patient information, and increasing satisfaction with nurses’ daily activities. IT, including nursing information systems, also improves clinical care planning, access to nursing documents and their readability, reduces duplicate documentation, facilitates the completion of nursing documents and medical examinations, and helps optimize nurses’ workflow (22). On the contrary, settings will be inefficient in the absence of clinical and technological competencies (8).
Accordingly, competency evaluation is essential not only to ensure the receipt of quality care but also to identify areas for improvement and determine nurses’ training needs (23). Meanwhile, in critical care nursing, clinical nurses are often unaware of new concepts that have entered the nursing literature. Due to a lack of knowledge and understanding, they continue to use only outdated nursing concepts. In fact, clinical nurses need to familiarize themselves with new concepts in nursing, understand their interrelationships, and strive to acquire the necessary competencies to improve the quality of nursing care.
Despite extensive research on these two concepts in other countries, few studies have been conducted in our country in this regard. Considering the role of nurses in providing high-quality care and the significance of applying IT to advance care goals, the present study aimed to determine the relationship between informatics competency and clinical competency in nurses working in ICUs.
Methods
Study design
The present cross-sectional research was conducted on 135 nurses working in the ICUs at hospitals affiliated with Golestan University of Medical Sciences based on sampling and inclusion criteria. The sampling method was stratified with proportional allocation. To determine the sample size, Ansari Jaberi et al.’s (2022) study investigating the association between nurses’ informatics competency and professional competency was used (16). Given that in this study, the correlation coefficient between professional competency and informatics competency was estimated to be r = 0.3, the sample size was determined to be 113 people according to the following formula.

In the above formula, α, denoting Type I error, was considered to be 0.05, and β, denoting Type II error, was considered to be 0.1. Considering the non-inclusion criterion, the sample size was increased by approximately 20%, and the final sample size was estimated to be n = 135.
Study setting
The sampling method was stratified according to the number of nurses working in each hospital. Two hospitals were selected from Gorgan city (n = 57), two hospitals from Gonbad city (n = 37), and one hospital from each of the other seven cities in the province (n = 41).
Measurement tools
For data collection, three tools were used: a demographic form (Including age, gender, marital status, work experience in the ICU, education level, work experience, interaction with the hospital information system (HIS), informatics course, frequency of computer use, employment type, position, and ethnicity), the Intensive and Critical Care Nursing Competency Scale-1 (ICCN-CS-1), and the Nursing Informatics Competency Scale (NICS).
The ICCN-CS-1 was designed by Lakanmaa et al. in Finland and translated and culturally adapted by Shouryabi et al. (2017) at Shahid Beheshti University of Medical Sciences by performing face validity, content validity, and construct validity (24). This scale contains 80 statements in 4 dimensions: Knowledge (20 factors), skill (20 factors), attitude and value (20 factors), and experience (20 factors). Scoring was performed using a 5-point Likert scale ranging from very poor (1) to excellent (6). The range of the clinical competency score was from 80 to 400. Scores higher than the average denoted greater clinical competency. The scale’s reliability was reported by calculating the Cronbach’s alpha coefficient of α = 0.96 for the total scale and 0.93-0.96 for the dimensions.
In addition, the NICS was designed by Staggers et al. and translated and culturally adapted by Farzandipour et al. (2018) at Kashan University of Medical Sciences. This scale contained 38 statements in three dimensions: Computer skills (15 statements), informatics knowledge (13 statements), and informatics skills (10 statements). Scoring was performed using a 4-point Likert scale ranging from very low (1) to very high (5). Scores higher than the average denoted greater informatics competency. The range of the informatics competency score was from 38 to 152. The scale’s reliability was confirmed by an intraclass correlation coefficient (ICC) of 0.97 for the total scale and 0.95-0.99 for the dimensions (8).
With ethical approval code from the university’s Deputy of Research and Technology and according to the sampling framework, the researcher visited the ICU at hospitals affiliated with the university and explained the research objectives and information confidentiality to nurses meeting the inclusion criteria. After obtaining written consent, the researcher provided the questionnaires to them. Due to the conditions of some ICU nurses’ busy schedules and with prior coordination for entering the ICU, the nurses were given a week to ten days to fill out the questionnaires at their leisure.
The inclusion criteria for nurses included having at least a bachelor’s degree in nursing, having at least 6 months of work experience in the ICU, working in the ICU, current employment in the ICU, and willingness to participate in the research. The exclusion criterion included incomplete questionnaires (24).
Statistical methods
The data were then entered into SPSS version 21 (SPSS Inc., Chicago, IL, USA). Descriptive parameters such as mean, median, and standard deviation were used, and the Shapiro-Wilk test was applied to assess the normality of the data. Spearman's rank correlation coefficient, Mann-Whitney, and Kruskal-Wallis tests were used due to the non-normality of the data. Non-normal variables included clinical competency dimensions such as knowledge, skill, attitudes and values, experience, and total. Furthermore, multiple linear regression and generalized multiple linear regression models were used. The significance level of all statistical tests was set at 0.05. Standardized and unstandardized beta coefficients were estimated along with a 95% confidence interval.
Results
In the present study, 135 ICU nurses were included, with a mean age of 30.75 ± 5.91 years (Range: 20 to 48) and a median age of 30 years. The highest total mean score of clinical competencies in the nurses was 58.41 ± 8.80, with the lowest being 31.15 and the highest being 68.75, denoting a favorable competency. In addition, regarding the areas of clinical competency, the highest and lowest mean scores belonged to the dimensions of value and attitude and experience, respectively (Table 1).
Moreover, the total mean score of informatics competency in the research units was 45.67 ± 18.88, with the lowest being 0 and the highest being 92.98, denoting a favorable competency. Concerning the dimensions of informatics competency, the highest and lowest mean scores belonged to the dimensions of informatics skills and informatics knowledge, respectively (Table 2).
In investigating the relationship between clinical competency and informatics competency, Spearman’s test results indicated no statistically significant association between clinical competency and informatics competency (r = 0.07, P = 0.42).
In investigating the simultaneous effects of explanatory variables on clinical competency, generalized multiple linear regression was used because the assumptions of the linear regression model were not met. Among the variables, only work experience in the ICU had a statistically significant relationship with clinical competency (β = 0.30, p = 0.02) (Table 3).
In investigating the simultaneous effects of explanatory variables on informatics competency, after ensuring the regression model assumptions by conducting multiple linear regression, only gender (β = -12.93, P = 0.001) and duration of using HIS in the ICU (β = -6.22, P = 0.008) indicated a statistically significant association with informatics competency (Table 4).
In investigating the relationship between clinical competency and informatics competency, Spearman’s test results indicated no statistically significant association between clinical competency and informatics competency (r = 0.07, P = 0.42).
In investigating the simultaneous effects of explanatory variables on clinical competency, generalized multiple linear regression was used because the assumptions of the linear regression model were not met. Among the variables, only work experience in the ICU had a statistically significant relationship with clinical competency (β = 0.30, p = 0.02) (Table 3).
In investigating the simultaneous effects of explanatory variables on informatics competency, after ensuring the regression model assumptions by conducting multiple linear regression, only gender (β = -12.93, P = 0.001) and duration of using HIS in the ICU (β = -6.22, P = 0.008) indicated a statistically significant association with informatics competency (Table 4).
|
Table 2. The distribution of clinical competency and informatics competency scores and their dimensions for ICU nurses
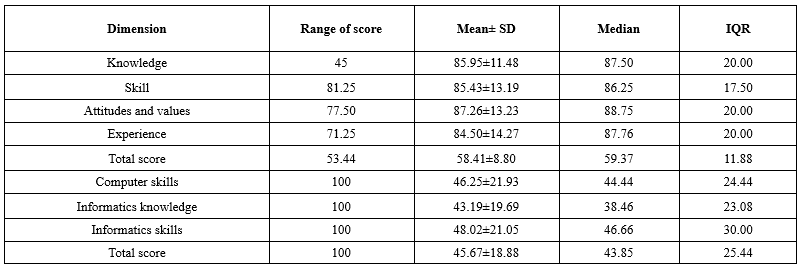 Table 3. The simultaneous effects of all explanatory variables on the clinical competency of ICU nurses .PNG) Table 4. The simultaneous effects of all explanatory variables on the informatics competency of ICU nurses .PNG) |
Discussion
In this study, the distribution of the scores of the informatics and clinical competency variables and their subscales was optimal, but there was no statistical relationship between the two variables of informatics nursing competency and clinical nursing competency. In addition, among the demographic variables, only work experience showed a statistically significant relationship with clinical competency, while gender and interaction with HIS showed a statistically significant difference with informatics competency.
In the present study, there was no statistically significant uniform relationship between the nurses’ clinical competency and informatics competency. On the contrary, Ansari Jaberi et al.’s (16) research confirmed the correlation between nurses’ informatics competency and professional-clinical competency. Jung et al.’s (25) research also indicated a positive and strong relationship between nurses’ informatics competency and clinical performance, which is not in line with the results of the current study.
In investigating the concurrency of explanatory variables with the clinical competency of nurses, only the work experience variable showed a statistically significant difference. This finding is in line with Elhami et al.’s (26) study but not with studies conducted by Faraji et al. (27) and Mirlashari et al. (28).
The study findings demonstrated that the mean score of clinical competencies in the nurses was reported to be favorable, which is consistent with Qorbanzadeh et al. (29), who also reported a favorable mean score of clinical competencies among nurses. Other studies, such as those by Fotouhi et al. (30), Zakeri et al. (31), and Sasaki et al. (32), similarly indicated a favorable mean score of competencies among nurses. On the other hand, the clinical competency score was reported to be at an excellent level in Kolagari et al.’s (33) study and at an average level in Karami et al.’s (34) study. In Ghonem et al.’s (35) study, the mean competency scores on the total scale and in various dimensions were poor. It seems that differences in the correct distribution of clinical nursing forces, the continuous evaluation of clinical competencies, the implementation of educational programs to improve clinical competency, and variations in setting facilities are among the contributing factors.
Among the clinical competency dimensions, the highest mean belonged to the attitude and value dimension, and the lowest to the experience dimension. In line with the present study, Ghahrisarabi et al. (18) also reported the highest mean score for the attitude and value dimension and the lowest for the knowledge dimension, whereas in Kolagari et al.’s (33) study, the highest and lowest mean scores were observed in the knowledge and skill dimensions, respectively. It can be acknowledged that the attitude and value dimension of most nurses working in clinical settings is equally influenced by their discipline, lessons learned, and the knowledge upon which they base their care for patients at the bedside. The difference in clinical competency scores among the dimensions highlights the gap between theory and clinical practice. Nurses need more experience and skill to achieve competency, while knowledge and awareness serve as predisposing factors.
The results of the present study also demonstrated that the mean score of informatics competency was generally favorable, which is consistent with the findings of Ansari Jaberi et al.’s (16) research, showing favorable informatics competency scores among participants. Farokhzadian et al. (6) and Jung et al. also reported that participants’ mean IT competency scores were at a favorable level, aligning with the present study findings. On the contrary, Batran et al.’s (36) study revealed that participants’ mean informatics competency scores were not favorable. In this study, the highest and lowest mean scores of informatics competency were in the informatics skills and informatics knowledge dimensions, respectively. Similarly, Kleib et al.’s (9) study indicated that participants’ self-reported mean score for informatics skills was optimal, whereas in Khezri et al.’s (37) research, basic computer skills had the highest mean score among participants. Differences in the level of informatics competency among nurses and its components across various studies may stem from the health system’s emphasis on IT and its role in advancing medical science professions, including nursing.
In investigating the concurrency of explanatory variables with nurses’ informatics competency, only the interaction with HIS and gender variables showed a statistically significant difference. Regarding HIS, it was observed that increased interaction with HIS was associated with reduced informatics competency. Consistent with the findings of the current research, Khezri et al.’s (37) study demonstrated an inverse correlation between informatics competency scores and the amount of time spent interacting with the hospital’s HIS, indicating that greater time spent with HIS led to reduced informatics competency. However, studies by Kinnunen et al. (38), Farzandipour et al. (8), and Karim et al. (39) found no statistically significant difference between nurses’ informatics competency and interaction with HIS. It may be suggested that the HIS variable is not contradictory to the components of informatics competency and that working with HIS may not significantly influence these competency components.
Regarding the gender variable, the results revealed a statistically significant difference between the participants’ informatics competency and gender. On the contrary, the findings of Al-Hawamdih et al.’s (40) study indicated no statistically significant difference between participants’ informatics competency and gender.
This study also had several limitations that should be considered when interpreting the data, including the complexity of ICU conditions compared to other hospital wards, the lack of sufficient time to complete the questionnaires, and the use of self-report questionnaires for data collection.
Conclusion
The findings showed that although the overall scores of informatics competency and clinical competence among the nurses were appropriate, there was no significant relationship or difference between the two variables. It seems that the importance of informatics competency, as one of the new dimensions of competence in the clinical setting, is still in its early stages, and more knowledge about it is needed. Therefore, it is recommended to emphasize the necessity of nurses’ skills and competence in the field of technology within the clinical setting. In addition, nurses should be motivated to improve professionally and acquire competency in new approaches by gaining updated knowledge.
Acknowledgement
This article has been extracted from a master’s thesis in intensive care nursing, supported by Golestan University of Medical Sciences. The researchers would like to thank the Research and Technology Department of Golestan University of Medical Sciences, as well as the dedicated and selfless nurses who assisted us despite their busy schedules.
Funding sources
This study was supported by the Deputy of Research and Technology at Golestan University of Medical Sciences.
Ethical statement
The present study was approved by the Ethics Committee of Golestan University of Medical Sciences, Gorgan, Iran (Code: IR.GOUMS.REC.1402.325). Written informed consent was obtained from the nurses participating in this research. In addition, the right to withdraw from the study and maintain the confidentiality of the data was ensured.
Conflicts of interest
None.
Author contributions
ShK designed the study, FT collected the data, and NGH analyzed and interpreted the data. ShK and KhY were major contributors to writing the manuscript. All authors read and approved the final manuscript.
Type of study: Original Article |
Subject:
Nursing
References
1. Sadeghi R, Yaghmayi F. Informatics applying in nursing; education, research and care. Educ Strategy Med Sci. 2012;5(3):199-206. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. von Gerich H, Alhuwail D, Badger MK, Block LJ, Eler GJ, Georgsson M, et al. Future Needs in Nursing Informatics-Preliminary Findings from the Global Nursing Informatics Survey. Stud Health Technol Inform. 2024;315:337-41. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Johnson CB. Nurse informaticists' role in promoting health equity. Nursing. 2024;54(5):38-44. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Guo J, Liu J, Liu C, Wang Y, Xu X, Chen Y. Nursing informatics competency and its associated factors among palliative care nurses: an online survey in mainland China. BMC Nurs. 2024;23(1):157. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. World Health Organization. Draft global strategy on digital health 2020-2025. 2021. [View at Publisher]
6. Farokhzadian J, Khajouei R, Hasman A, Ahmadian L. Nurses' experiences and viewpoints about the benefits of adopting information technology in health care: a qualitative study in Iran. BMC Med Inform Decis Mak. 2020;20(1):240. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Rouleau G, Gagnon MP, Côté J, Payne-Gagnon J, Hudson E, Dubois CA. Impact of information and communication technologies on nursing care: results of an overview of systematic reviews. J Med Internet Res. 2017;19(4):e122. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Farzandipour M, Mohamadian H, Akbari H, Safari S, Sharif R. Designing a national model for assessment of nursing informatics competency. BMC Med Inform Decis Mak. 2021;21(1):35. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Kleib M, Nagle LM, Furlong KE, Paul P, Wisnesky UD, Ali S. Are future nurses ready for digital health?: informatics competency baseline assessment. Nurse Educ. 2022;47(5):E98-E104. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Kamel Abdel-Razik M, Gad AEFA, Farouk Kamel F, Abd Alla Saleh H .Efficacy of Guidance Program about Informatics Competencies for Staff Nurses and its Effect on Patients Safety. Journal of Nursing Science Benha University. 2024;5(1):659-677. [View at Publisher] [DOI] [Google Scholar]
11. Kaihlanen A-M, Gluschkoff K, Kinnunen U-M, Saranto K, Ahonen O, Heponiemi T. Nursing informatics competences of Finnish registered nurses after national educational initiatives: A cross-sectional study. Nurse Educ Today. 2021;106:105060. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Nafar L, Negarandeh R, sarkani N , Nikpema N. Cultural competence and its related factors in health care workers working in comprehensive health centers affiliated to Tehran University of Medical Sciences. HAYAT. 2022;28(1):59-71. [View at Publisher] [Google Scholar]
13. Negarandeh R, Pedram Razi SH, Khosravinezhad M . The effect of using the services of nurses with clinical competence on the safety and satisfaction of nursing services in patients admitted to the emergency department. HAYAT. 2013;19(1):64-53. [View at Publisher]
14. Monshizadeh A, Nasiriani K, Khodayarian M, Shakerfar H, Fallahfaragheh A. The effect of Multidimensional Orientation Program on the Clinical Competence of Beginner Nurses Working in Intensive Care Units: a Quasi-Experimental Study. Journal of Health and Care. 2023;24(4):298-309. [View at Publisher] [DOI] [Google Scholar]
15. le Roux L, Bimerew M, Chipps J. A survey of nurse informatics competencies of professional nurses in clinical practice public hospitals in South Africa. International Journal of Africa Nursing Sciences. 2024;21:100783. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Ansari Jaberi A, Sahebi Z, Riahi Paghaleh Z, Ansari Jaberi K, Negahban Bonabi T. Can Nurses' Informatics Competency Predict Their Professional Competency? J Occup Health Epidemiol. 2022;11(1):41-7. [View at Publisher] [DOI] [Google Scholar]
17. Zareshahi M, Mirzaei S, Nasiriani K. Nursing informatics competencies in critical care unit. Health Informatics J. 2022;28(1):14604582221083843. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Ghahrisarabi A, Shouryabi A, Anboohi S, Nasiri M, Rassouli M. Clinical and Professional Competence of Practicing Nurses in intensive critical care units. Research Journal of Medical Sciences. 2016;10(4):406-11. [View at Publisher] [DOI] [Google Scholar]
19. Najafi B, Nakhaei M, Vagharseyyedin SA. Clinical competence of nurses: a systematic review study. Quarterly Journal of Nursing Management. 2022;11(1):1-9. [View at Publisher]
20. Bijan B, Rezaei J, Ashtarian H, Hashemian AH, Azami H. The relationship between clinical competence and organizational commitment and factors affecting it in nurses working in Intensive Care units of Kermanshah public hospitals. Avicenna J Nurs Midwifery Care. 2024;32(1):29-38. [View at Publisher] [DOI] [Google Scholar]
21. Najafi Ghezeljeh T, Samadi Beiram Z, Omrani S, Haghani S. Evaluating the effectiveness of electronic learning on patient safety competency of nurses in intensive care unit: A quasi-experimental study. Iran J Nurs. 2022;35(136):162-77. [View at Publisher] [DOI] [Google Scholar]
22. Varzeshnejad M, Namnabati M, Taleghani F. A Successful Step towards Application of Informatics in Nursing in Iran. Journal of Health and Biomedical Informatics. 2017;4(2):71-83. [View at Publisher] [Google Scholar]
23. Imani B, Vanaki Z, Mohamdkhan Kermanshahi S, Karampourian A. Karampourian, The correlation between nurses' clinical competency and emotional intelligence in nurses of health care units in hamadan university of medical sciences hospitals. Quarterly Journal of Nursing Management. 2018;7(3):27-34. [View at Publisher] [Google Scholar]
24. Shouryabi AA, Ghahrisarabi A, Anboohi SZ, Nasiri M, Rassouli M. Psychometric properties of the Persian version of the Intensive and Critical Care Nursing Competence Scale version-1 (ICCN-CS-1). Electron Physician. 2017;9(11):5785-92. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Jung IO, Han JH. The effect of emotional labor, nursing informatics competency and nursing service environment on nursing performance of convalescent hospital nurse. Journal of the Korea Academia-Industrial Cooperation Society. 2020;21(10):334-44. [View at Publisher] [DOI] [Google Scholar]
26. Elhami S, Ban M, Mousaviasl S, Zahedi A. Self-evaluation of nurses clinical competency based on Benner theory. World Family Medicine. 2018;16(3):191-7. [View at Publisher] [DOI] [Google Scholar]
27. Faraji A, Karimi M, Azizi SM, Janatolmakan M, Khatony A. Evaluation of clinical competence and its related factors among ICU nurses in Kermanshah-Iran: A cross-sectional study. Int J Nurs Sci. 2019;6(4):421-5. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Mirlashari J, Qommi R, Nariman S, Bahrani N, Begjani J. Clinical competence and its related factors of nurses in neonatal intensive care units. J Caring Sci. 2016;5(4):317-24. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Ghorbanzadeh K, Sadeghi H, Nasiri K, Jafari M, Eghbali M, Asvar R. Investigating the Relationship between Clinical Competence and Nurses' Job Satisfaction. Journal of Health and Care. 2022;24(1):7-16. [View at Publisher] [DOI] [Google Scholar]
30. Fotohi P, Olyaie N, Salehi K. The dimensions of clinical competence of nurses working in critical care units and their relation with the underlying factors. Quarterly Journal of Nursing Management. 2019;8(2):1-9. [View at Publisher] [Google Scholar]
31. Zakeri MA, Bazmandegan G, Ganjeh H, Zakeri M, Mollaahmadi S, Anbariyan A, et al. Is nurses' clinical competence associated with their compassion satisfaction, burnout and secondary traumatic stress? A cross‐sectional study. Nurs Open. 2020;8(1):354-63. [View at Publisher] [DOI] [PMID] [Google Scholar]
32. Sasaki S, Fukada M, Okuda R, Fujihara Y. Impact of organization and career commitment on clinical nursing competency. Yonago Acta Med. 2019;62(2):221-231. [View at Publisher] [DOI] [PMID] [Google Scholar]
33. Kolagari Sh, Najafi M, Brojerdi M, Modanloo M. Clinical competency of nurses working at Intensive Care Units and its associated factors. J Res Dev Nurs Midw. 2023;20(2):50-3. [View at Publisher] [DOI] [PMID] [Google Scholar]
34. Karami A, Farokhzadian J, Foroughameri G. Nurses' professional competency and organizational commitment: Is it important for human resource management? PloS One. 2017;12(11):e0187863. [View at Publisher] [DOI] [PMID] [Google Scholar]
35. Ghonem NME-S, Ibrahim FFE, Ahmed Abd elrahman RM. Information Technology: Nurses' Attitudes towards the Use of Computer and Their Informatics Competences in Nursing Practice. Assiut Scientific Nursing Journal. 2023;11(34):89-97. [View at Publisher] [DOI] [Google Scholar]
36. Batran A, Al-Humran SM, Malak MZ, Ayed A. The relationship between nursing informatics competency and clinical decision-making among nurses in West Bank, Palestine. Comput Inform Nurs. 2022;40(8):547-53. [View at Publisher] [DOI] [PMID] [Google Scholar]
37. Khezri H, Abdekhoda M. Assessing nurses' informatics competency and identifying its related factors. J Res Nurs. 2019;24(7):529-38. [View at Publisher] [DOI] [PMID] [Google Scholar]
38. Kinnunen U-M, Kuusisto A, Koponen S, Ahonen O, Kaihlanen A-M, Hassinen T, et al. Nurses' Informatics Competency Assessment of Health Information System Usage: A Cross-sectional Survey. Comput Inform Nurs. 2023;41(11):869-76. [View at Publisher] [DOI] [PMID] [Google Scholar]
39. Karim J, Veni SV, Hamzah A, Adlan N, Mat R. Nursing Informatics Competency among Nurses at a Teaching Hospital in Malaysia. Education in Medicine Journal. 2024;16(Supp1):55. [View at Publisher] [DOI] [Google Scholar]
40. Al-Hawamdih S, Ahmad MM. Examining the relationship between nursing informatics competency and the quality of information processing. Comput Inform Nurs. 2018;36(3):154-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |