Volume 21, Issue 2 (6-2024)
J Res Dev Nurs Midw 2024, 21(2): 16-21 |
Back to browse issues page
Ethics code: No. 615/HDDD-DHYD signed on July 7, 2022
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Nguyen N T, Lam Q M, Do H T. The effectiveness of warm perineal compresses during the second stage of labor on perineal trauma and labor pain: A Systematic Review. J Res Dev Nurs Midw 2024; 21 (2) :16-21
URL: http://nmj.goums.ac.ir/article-1-1627-en.html
URL: http://nmj.goums.ac.ir/article-1-1627-en.html
1- University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam
2- University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam ,minhquang0202@yahoo.com
2- University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam ,
Full-Text [PDF 610 kb]
(2111 Downloads)
| Abstract (HTML) (2953 Views)
Full-Text: (1071 Views)
Introduction
Childbirth is a physiological event that allows the fetus to be expelled from the mother's uterus and birth canal (1). The pain of childbirth is one of the most intense pains that women experience in their lifetime and is a common concern for first-time mothers (2-5). Effective pain control is critical for a satisfying childbirth experience (6). Pain that is not managed appropriately can adversely affect the woman and her fetus and can influence the labor and delivery experience (7). Pain relief gives women control and enables them to participate in the childbirth experience (8).
One of the common causes of pain during the second stage of labor is perineal injury (2,3,9). Perineal trauma is a common complication of childbirth, affecting approximately 53 to 79% of women and negatively affecting a woman's quality of life, including perineal pain, urinary incontinence, difficulty urinating, and sexual dysfunction (10,11). Perineal tears can range from first-degree to fourth-degree, with increasing severity. Most perineal tears are first- or second-degree tears, which involve the skin and muscles of the perineum. However, more severe perineal tears, such as third- and fourth-degree tears, can also occur. Third- and fourth-degree tears involve the anal sphincter and can cause significant pain and complications. A study conducted in England found that the prevalence of perineal tears among primiparous women (women who are giving birth for the first time) was 91.4%. At 8 weeks after birth, 22% of new mothers have reported continued perineal pain (12).
The World Health Organization recommends using warm perineal compresses during the second stage of labor to reduce the risk of perineal injuries (13). Warm compresses work by dilating blood vessels and improving blood supply to the perineum. This helps to reduce pain and inflammation and can also help to prevent tears. A study found that 80.4% of midwives and 79.7% of mothers agreed with the effectiveness of warm compresses on labor pain (14). Midwives also advised continuing to use warm perineal compresses for women who give birth (15). Warm perineal compresses are commonly suggested as a safe and effective way to reduce the risk of perineal injuries during childbirth as well as the risk of labor pain. However, it should be noted that the effectiveness of this method is not always found. A clinical experiment conducted among three groups of interventions: perineal warm compress, midwife massage with lubricant, and no intervention reported that the prevalence of perineal and vaginal injury did not differ substantially across groups (16).
Researchers have been tempted to investigate the use of warm perineal compresses during labor for pain management; a meta-analysis on this topic was published in 2019 with, however, a small number of seven articles included (17). Since there is not a solid confirmation of the effectiveness of this method yet, it is worth continuing to conduct systematic reviews using the updated database to provide a clearer view of the topic. This systematic review aimed to examine the effectiveness of warm perineal compresses during the second stage of labor on 1) perineal conditions (laceration, intact, suturing required, episiotomy, intensity of perineal trauma) after delivery and 2) the relief of labor pain, from which we were expected to provide reliable evidence to help make informed decisions about the use of warm perineal compresses during childbirth. Results from this study can also be considered a comparative reference for similar research in the future.
Methods
Study design:
The systematic review was conducted at the University of Medicine and Pharmacy at Ho Chi Minh City in June - July 2023 and included articles published from inception up to the present day (as of July 2023). The literature search was conducted using the following databases: PubMed, Google Scholar, and ScienceDirect.
Search strategy:
In PubMed, MeSH (medical subject headings) and other terms were used, and the search string was generated as follows: (randomized controlled trial OR RCT) AND (spontaneous vaginal delivery OR SVD OR vaginal delivery OR natural childbirth OR childbirth) AND (warm perineal compresses OR warm compresses OR perineal compresses OR heat compresses OR warm packs OR thermal compresses) AND (perineal trauma OR perineal tear OR perineal laceration OR perineal rupture) AND (second stage of labor OR SSL). In Google Scholar, the search string was: (“spontaneous vaginal delivery” OR “vaginal delivery” OR “natural childbirth OR childbirth”) AND (“warm perineal compresses” OR “warm compresses OR perineal compresses” OR “heat compresses” OR “warm packs” OR “thermal compresses”) AND (“perineal OR “perineum”) AND (“trauma OR tear OR “laceration” OR “rupture” OR “pain” OR “intact” OR “episiotomy”) AND (“second stage of labor” OR “uterine contractions”). In ScienceDirect, the search string was: ("randomized controlled trial") AND ("vaginal delivery" OR "natural childbirth") AND ("warm compress" OR "heat compress") AND ("trauma" OR "pain") AND ("second stage of labor" OR "uterine contractions").
Selection criteria:
The titles and abstracts of all articles retrieved from the literature search were screened by two independent reviewers. Full-text articles were retrieved for those that met the following inclusion criteria: 1) Randomized controlled trials (RCTs) or quasi-RCTs; 2) The study population was women who were planning to give birth vaginally; 3) The intervention was the use of warm perineal compresses during the second stage of labor; 4) The outcomes included pain measurement and/or perineal trauma and/or other perineal status after delivery. Articles that were not published in English were excluded from the research. Microsoft Excel program was used to examine the outcome variables.
Data extraction:
Two independent reviewers extracted data from the included studies using a standardized data extraction form. The following data were extracted: 1) The study’s baseline characteristics: treatment for the control group, maternal mean age and age range, gestational mean age, and age range, 2) Pregnancy-related selection criteria, 3) Detailed information on the intervention method, 4) Outcomes: incidence of perineal laceration, intact perineum, perineum trauma required suturing, episiotomy, severity of perineum trauma (1st to 4th degree), pain score, intensity of pain by categorization (for example: mild, moderate, severe, very severe). The principal investigator made the final decision in cases of discrepancies or queries from reviewers.
Risk of bias assessment:
The risk of bias in the included studies was assessed using the Cochrane risk-of-bias tools for Systematic Reviews of Interventions. All studies were evaluated based on the following criteria: 1) random sequencing; 2) allocation masking (selection deviation); 3) blinding participants and staff (performance deviation); 4) blinding outcome evaluators (detection deviation); 5) incomplete outcome data (attrition deviation); 6) selective reporting of results (reporting bias); 7) other deviations. The reviews of authors’ judgments were categorized as “low risk”, “high risk”, or “unclear risk” of bias.
Reporting and ethical consideration:
The results of the systematic review were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Being designed as a systematic review extracting data from published articles, an ethical review for this study might be exempt. However, information about the ethical approval of the selected articles was reported as part of the quality assessment.
Results
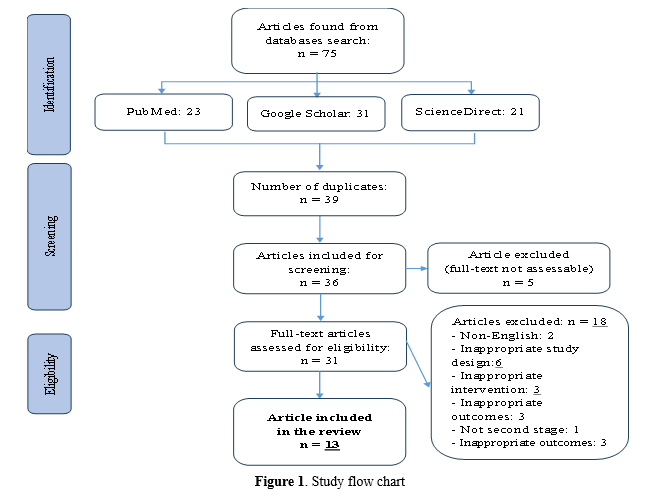
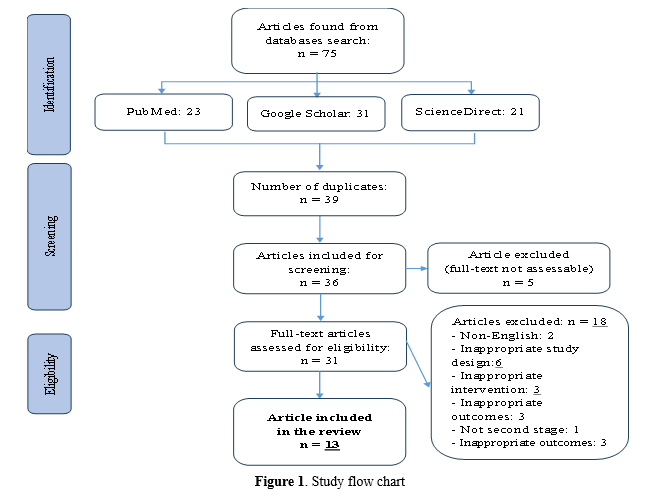
Thirteen trials, involving 2,907 participants, met the inclusion criteria for this systematic review (Figure 1). Most studies had a low risk of bias in random sequencing, allocation, selective reporting, and incomplete outcome data, according to the Cochrane Collaboration’s tool. The risk of the two blinding criteria was high due to the nature of the intervention (Figure 2).
Most studies were conducted in Asia, with a 1:1 ratio of intervention and control groups (15,18-25). In most studies, the control group received routine hospital care; one study compared the outcomes of the warm compress method with perineal massage therapy (24). The mean maternal age was approximately 25 years old in all studies, and the mean gestational age was 39 weeks. Seven of the selected studies provided ethical approval for their trials (15,19,22,23,26-28) (Table 1).
Pregnancy-related selection criteria were seen in most trials, but not all these criteria were required. The most common criteria were that the women were primiparous (giving birth for the first time), had a healthy term pregnancy, and were carrying a singleton baby with cephalic presentation (head down). Two studies limited the baby's birth weight to between 2,500 and 4,000 grams. Two studies did not report their pregnancy-related criteria (21,25) (Table 2).
 The application of warm compresses varied with each trial. Most studies used warm compresses made from clean washcloths immersed in warm water and applied to the perineal area (19,22-25,27). There was one study that sequentially applied warm packs and ice packs as their intervention (20) (Table 3).
The application of warm compresses varied with each trial. Most studies used warm compresses made from clean washcloths immersed in warm water and applied to the perineal area (19,22-25,27). There was one study that sequentially applied warm packs and ice packs as their intervention (20) (Table 3).
The rates of intact perineum and episiotomy were the most reported outcomes. The rate of intact perineum was significantly higher in the warm compresses group than the control group in most trials (15,21,22,24,25,29). Two studies found no significant difference in the intact between the two groups (18,23).
There were eight studies that reported episiotomy outcomes, in which the rate of episiotomy was significantly lower in the warm compress group than the control group in three studies (18,22,29). The rate of perineal lacerations was reported in five trials, and there was a significant difference between the two groups in all of them (15,21,22,24,29). Four of these trials reported a lower rate of lacerations in the warm compresses group (15,21,24,29), while one reported the opposite result (22). One trial found a significantly lower rate of perineal injuries required suturing in the warm compresses group than the control group (29) (Table 4).
Table 5 shows the results of the severity of perineal trauma from the trials.
One trial reported a significantly higher rate of 3rd-4th level of trauma in the control group than in the intervention group; the p-value, however, was not shown (26). Another trial reported that the warm compresses group had a higher rate of 1st-level and lower rates of 2nd- and 3rd-level of trauma, but the differences were weakly significant (22).
Table 6 shows the pain scores reported in three trials (19,20,25). The pain scores in the warm compresses group were lower than those in the control group after the intervention was applied and after delivery (19,20,25). The differences were significant in two out of three trials (19,20).
Table 7 also shows that the pain severity was significantly different between the two groups. Specifically, the rate of severe pain or higher levels was reported to be lower in the warm compresses group than the control group in most of the selected trials (19,21,23,29).
Discussion
This systematic review of thirteen studies involving 2,907 participants was conducted to assess the effectiveness of warm perineal compresses during the second stage of labor on perineal conditions after delivery and labor-related pain. The included studies were conducted in eight countries, mostly in Asia and Africa. Among the studies, seven trials recommended the use of warm compresses for pain relief and perineal preservation during the second stage of labor, and five trials specifically stated that warm compresses were effective in decreasing perineal laceration and labor pain. However, one trial found that the use of warm compresses should be based on maternal comfort and other considerations, and another trial suggested that further research is needed on this topic (18,26).
Regarding the risk of bias, at least one criterion was rated as high risk or unsure in every trial. The blinding criteria seemed unable to be reached using this intervention. It can be concluded that warm perineal compresses are effective in reducing perineal laceration and labor pain, but the results should be interpreted with caution due to the risk of bias and the small number of studies included.
Intervention methodology and outcome measurement
The methodology of warm compress application varied across the studies, including the item used, the duration of application, the temperature, the location of application, and the time point of application. For measuring pain, most studies used a visual scale for pain, but the way pain results were classified varied from study to study. These differences can prevent making uniform judgments about the effectiveness of warm compresses on outcomes of interest. However, despite the methodological differences, most studies reported a good effect of warm compresses on one or more outcomes compared with control groups. This finding suggests that warm compresses may be an effective intervention for reducing perineal laceration and labor pain, but further research is needed to confirm these findings and standardize the interventions used.
Effect of warm compresses on labor pain
The evaluation of labor pain by scores and when grouping pain levels showed a clear effect of warm compresses on pain relief. In most of the studies, pain scores in the warm group were significantly lower than in the control group (19,20). Similar findings were observed in pain severity studies: the warm compresses group had the majority of mild or moderate pain, while the control group had a higher percentage of severe pain (19,21-23,29). This result is consistent with the mechanism of action of passive vasodilation measures, which improve blood supply and temporarily block pain signals from reaching the brain (30). The results suggest that warm compresses can be used to relieve pain during the second phase of labor.
Effectiveness of warm compresses on perineal injuries
Most studies showed that warm compresses were associated with lower rates of perineal laceration. However, in a trial conducted by Akbarzadeh, the author reported a higher rate of perineal laceration in the warm compresses group without a specific discussion for this result (15). In some cases, applying warm compresses to the perineum might soften the tissue and make it less resilient, potentially increasing the likelihood of tearing during childbirth. Moreover, the warm compress used in Akbarzadeh’s study was put in water at 70oC; this temperature was much higher than most studies (usually ranging from 45 to 59oC). In summary, most of the intact perineum outcomes reported by the trials supported the use of warm compresses, as they helped maintain the perineum’s integrity during the second stage of labor.
The rate of perineum trauma that required suturing did not differ between the warm compresses group and the control group. Results on episiotomy rates between the two groups were also inconsistent: three out of eight trials showed that the warm compresses group had a significantly lower rate of perineal tear than the control group (18,22,29); five did not find the difference between groups (20,23,24,26,27). Besides, evidence for the effectiveness of warm compresses in reducing the severity of perineal trauma was either weak or not significantly different between the intervention group and the control group. Besides the methods applied during the delivery stages, other factors might have played a larger role in determining the perineal trauma status. These could include the size and position of the baby, or the mother's anatomy. In summary, warm compresses have been shown to be effective in reducing perineal trauma that does not require suturing and without perineal tears. Considerations should be made before applying this intervention for the purpose of reducing perineal tears or episiotomies during labor.
Limitations of the study
Quasi-experimental trials are included in this systematic review; they can introduce bias into the results. However, by carefully selecting trials and assessing the risk of bias in each study, such bias was minimized. Differences in the way the warm compresses were performed may also lead to heterogeneity and make it difficult to draw a uniform conclusion. However, the overall trend of the results among trials still supports the use of warm compresses in reducing labor pain and perineal trauma. Due to the lack of information from the selected trials, a meta-analysis was not performed in this review and may be considered in future research. This review excluded trials conducted in languages other than English; thus, a comprehensive approach to the topic may not be reached. It should also be noted that similar systematic reviews on the same topic have been conducted (17,31,32). However, with the addition of recently published trials, our review may provide more solid evidence for the effectiveness of warm compresses on pain and perineal outcomes during labor.
Conclusion
In conclusion, the use of warm compresses during the second stage of labor has been shown to be effective in lowering pain and perineal injuries without the need for suturing. Due to the mixed results found, considerations should be made before applying this method to reduce perineal tears or episiotomies during labor.
Acknowledgement
We thanked the University of Medicine and Pharmacy at Ho Chi Minh City for providing the funds for conducting this research.
Funding sources
The research received funding from the potential project of the University of Medicine and Pharmacy at Ho Chi Minh City digital contract 189/2021/HĐ - ĐHYD led by Dr. Nhan Thi Nguyen.
Ethical statement
Ethics Council in Biomedical Research, University of Medicine and Pharmacy at Ho Chi Minh City. No. 615/HDDD-DHYD signed on July 7, 2022.
Conflicts of interest
The authors declare that they have no competing interests.
Author contributions
All authors contributed to the writing of the manuscript and read and approved the final manuscript.
Childbirth is a physiological event that allows the fetus to be expelled from the mother's uterus and birth canal (1). The pain of childbirth is one of the most intense pains that women experience in their lifetime and is a common concern for first-time mothers (2-5). Effective pain control is critical for a satisfying childbirth experience (6). Pain that is not managed appropriately can adversely affect the woman and her fetus and can influence the labor and delivery experience (7). Pain relief gives women control and enables them to participate in the childbirth experience (8).
One of the common causes of pain during the second stage of labor is perineal injury (2,3,9). Perineal trauma is a common complication of childbirth, affecting approximately 53 to 79% of women and negatively affecting a woman's quality of life, including perineal pain, urinary incontinence, difficulty urinating, and sexual dysfunction (10,11). Perineal tears can range from first-degree to fourth-degree, with increasing severity. Most perineal tears are first- or second-degree tears, which involve the skin and muscles of the perineum. However, more severe perineal tears, such as third- and fourth-degree tears, can also occur. Third- and fourth-degree tears involve the anal sphincter and can cause significant pain and complications. A study conducted in England found that the prevalence of perineal tears among primiparous women (women who are giving birth for the first time) was 91.4%. At 8 weeks after birth, 22% of new mothers have reported continued perineal pain (12).
The World Health Organization recommends using warm perineal compresses during the second stage of labor to reduce the risk of perineal injuries (13). Warm compresses work by dilating blood vessels and improving blood supply to the perineum. This helps to reduce pain and inflammation and can also help to prevent tears. A study found that 80.4% of midwives and 79.7% of mothers agreed with the effectiveness of warm compresses on labor pain (14). Midwives also advised continuing to use warm perineal compresses for women who give birth (15). Warm perineal compresses are commonly suggested as a safe and effective way to reduce the risk of perineal injuries during childbirth as well as the risk of labor pain. However, it should be noted that the effectiveness of this method is not always found. A clinical experiment conducted among three groups of interventions: perineal warm compress, midwife massage with lubricant, and no intervention reported that the prevalence of perineal and vaginal injury did not differ substantially across groups (16).
Researchers have been tempted to investigate the use of warm perineal compresses during labor for pain management; a meta-analysis on this topic was published in 2019 with, however, a small number of seven articles included (17). Since there is not a solid confirmation of the effectiveness of this method yet, it is worth continuing to conduct systematic reviews using the updated database to provide a clearer view of the topic. This systematic review aimed to examine the effectiveness of warm perineal compresses during the second stage of labor on 1) perineal conditions (laceration, intact, suturing required, episiotomy, intensity of perineal trauma) after delivery and 2) the relief of labor pain, from which we were expected to provide reliable evidence to help make informed decisions about the use of warm perineal compresses during childbirth. Results from this study can also be considered a comparative reference for similar research in the future.
Methods
Study design:
The systematic review was conducted at the University of Medicine and Pharmacy at Ho Chi Minh City in June - July 2023 and included articles published from inception up to the present day (as of July 2023). The literature search was conducted using the following databases: PubMed, Google Scholar, and ScienceDirect.
Search strategy:
In PubMed, MeSH (medical subject headings) and other terms were used, and the search string was generated as follows: (randomized controlled trial OR RCT) AND (spontaneous vaginal delivery OR SVD OR vaginal delivery OR natural childbirth OR childbirth) AND (warm perineal compresses OR warm compresses OR perineal compresses OR heat compresses OR warm packs OR thermal compresses) AND (perineal trauma OR perineal tear OR perineal laceration OR perineal rupture) AND (second stage of labor OR SSL). In Google Scholar, the search string was: (“spontaneous vaginal delivery” OR “vaginal delivery” OR “natural childbirth OR childbirth”) AND (“warm perineal compresses” OR “warm compresses OR perineal compresses” OR “heat compresses” OR “warm packs” OR “thermal compresses”) AND (“perineal OR “perineum”) AND (“trauma OR tear OR “laceration” OR “rupture” OR “pain” OR “intact” OR “episiotomy”) AND (“second stage of labor” OR “uterine contractions”). In ScienceDirect, the search string was: ("randomized controlled trial") AND ("vaginal delivery" OR "natural childbirth") AND ("warm compress" OR "heat compress") AND ("trauma" OR "pain") AND ("second stage of labor" OR "uterine contractions").
Selection criteria:
The titles and abstracts of all articles retrieved from the literature search were screened by two independent reviewers. Full-text articles were retrieved for those that met the following inclusion criteria: 1) Randomized controlled trials (RCTs) or quasi-RCTs; 2) The study population was women who were planning to give birth vaginally; 3) The intervention was the use of warm perineal compresses during the second stage of labor; 4) The outcomes included pain measurement and/or perineal trauma and/or other perineal status after delivery. Articles that were not published in English were excluded from the research. Microsoft Excel program was used to examine the outcome variables.
Data extraction:
Two independent reviewers extracted data from the included studies using a standardized data extraction form. The following data were extracted: 1) The study’s baseline characteristics: treatment for the control group, maternal mean age and age range, gestational mean age, and age range, 2) Pregnancy-related selection criteria, 3) Detailed information on the intervention method, 4) Outcomes: incidence of perineal laceration, intact perineum, perineum trauma required suturing, episiotomy, severity of perineum trauma (1st to 4th degree), pain score, intensity of pain by categorization (for example: mild, moderate, severe, very severe). The principal investigator made the final decision in cases of discrepancies or queries from reviewers.
Risk of bias assessment:
The risk of bias in the included studies was assessed using the Cochrane risk-of-bias tools for Systematic Reviews of Interventions. All studies were evaluated based on the following criteria: 1) random sequencing; 2) allocation masking (selection deviation); 3) blinding participants and staff (performance deviation); 4) blinding outcome evaluators (detection deviation); 5) incomplete outcome data (attrition deviation); 6) selective reporting of results (reporting bias); 7) other deviations. The reviews of authors’ judgments were categorized as “low risk”, “high risk”, or “unclear risk” of bias.
Reporting and ethical consideration:
The results of the systematic review were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Being designed as a systematic review extracting data from published articles, an ethical review for this study might be exempt. However, information about the ethical approval of the selected articles was reported as part of the quality assessment.
Results
Thirteen trials, involving 2,907 participants, met the inclusion criteria for this systematic review (Figure 1). Most studies had a low risk of bias in random sequencing, allocation, selective reporting, and incomplete outcome data, according to the Cochrane Collaboration’s tool. The risk of the two blinding criteria was high due to the nature of the intervention (Figure 2).
Most studies were conducted in Asia, with a 1:1 ratio of intervention and control groups (15,18-25). In most studies, the control group received routine hospital care; one study compared the outcomes of the warm compress method with perineal massage therapy (24). The mean maternal age was approximately 25 years old in all studies, and the mean gestational age was 39 weeks. Seven of the selected studies provided ethical approval for their trials (15,19,22,23,26-28) (Table 1).
Pregnancy-related selection criteria were seen in most trials, but not all these criteria were required. The most common criteria were that the women were primiparous (giving birth for the first time), had a healthy term pregnancy, and were carrying a singleton baby with cephalic presentation (head down). Two studies limited the baby's birth weight to between 2,500 and 4,000 grams. Two studies did not report their pregnancy-related criteria (21,25) (Table 2).
 The application of warm compresses varied with each trial. Most studies used warm compresses made from clean washcloths immersed in warm water and applied to the perineal area (19,22-25,27). There was one study that sequentially applied warm packs and ice packs as their intervention (20) (Table 3).
The application of warm compresses varied with each trial. Most studies used warm compresses made from clean washcloths immersed in warm water and applied to the perineal area (19,22-25,27). There was one study that sequentially applied warm packs and ice packs as their intervention (20) (Table 3).The rates of intact perineum and episiotomy were the most reported outcomes. The rate of intact perineum was significantly higher in the warm compresses group than the control group in most trials (15,21,22,24,25,29). Two studies found no significant difference in the intact between the two groups (18,23).
There were eight studies that reported episiotomy outcomes, in which the rate of episiotomy was significantly lower in the warm compress group than the control group in three studies (18,22,29). The rate of perineal lacerations was reported in five trials, and there was a significant difference between the two groups in all of them (15,21,22,24,29). Four of these trials reported a lower rate of lacerations in the warm compresses group (15,21,24,29), while one reported the opposite result (22). One trial found a significantly lower rate of perineal injuries required suturing in the warm compresses group than the control group (29) (Table 4).
Table 5 shows the results of the severity of perineal trauma from the trials.
Table 1. Baseline characteristics of the selected articles (n = 13)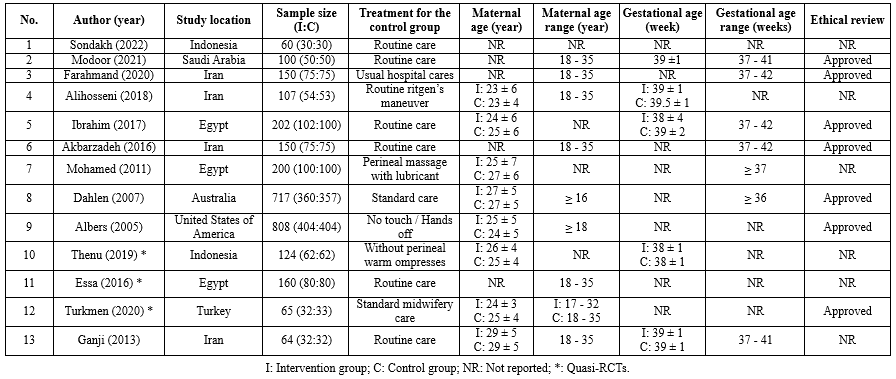 Table 2. Selection criteria of the selected articles (n = 13)  Table 3. Interventions of the selected articles (n = 13) .PNG) |
Table 6 shows the pain scores reported in three trials (19,20,25). The pain scores in the warm compresses group were lower than those in the control group after the intervention was applied and after delivery (19,20,25). The differences were significant in two out of three trials (19,20).
Table 7 also shows that the pain severity was significantly different between the two groups. Specifically, the rate of severe pain or higher levels was reported to be lower in the warm compresses group than the control group in most of the selected trials (19,21,23,29).
Table 4. Perineal outcomes of the selected articles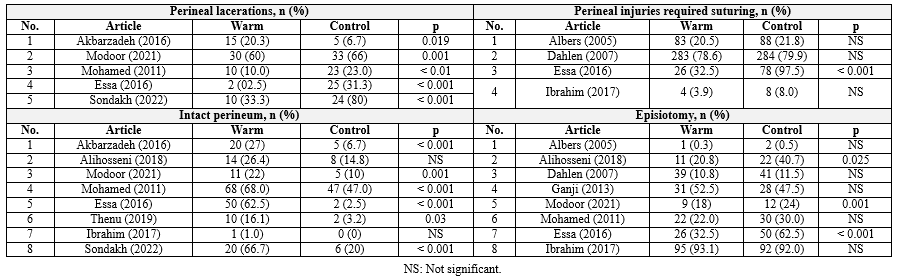 Table 5. Severity of perineal trauma in the selected articles (n = 4)  Table 6. Pain score outcomes of the selected articles (n = 3) 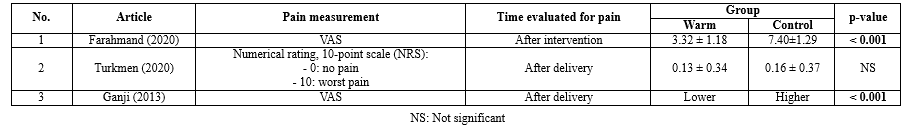 Table 7. Pain severity of the selected articles (n = 5)  |
Discussion
This systematic review of thirteen studies involving 2,907 participants was conducted to assess the effectiveness of warm perineal compresses during the second stage of labor on perineal conditions after delivery and labor-related pain. The included studies were conducted in eight countries, mostly in Asia and Africa. Among the studies, seven trials recommended the use of warm compresses for pain relief and perineal preservation during the second stage of labor, and five trials specifically stated that warm compresses were effective in decreasing perineal laceration and labor pain. However, one trial found that the use of warm compresses should be based on maternal comfort and other considerations, and another trial suggested that further research is needed on this topic (18,26).
Regarding the risk of bias, at least one criterion was rated as high risk or unsure in every trial. The blinding criteria seemed unable to be reached using this intervention. It can be concluded that warm perineal compresses are effective in reducing perineal laceration and labor pain, but the results should be interpreted with caution due to the risk of bias and the small number of studies included.
Intervention methodology and outcome measurement
The methodology of warm compress application varied across the studies, including the item used, the duration of application, the temperature, the location of application, and the time point of application. For measuring pain, most studies used a visual scale for pain, but the way pain results were classified varied from study to study. These differences can prevent making uniform judgments about the effectiveness of warm compresses on outcomes of interest. However, despite the methodological differences, most studies reported a good effect of warm compresses on one or more outcomes compared with control groups. This finding suggests that warm compresses may be an effective intervention for reducing perineal laceration and labor pain, but further research is needed to confirm these findings and standardize the interventions used.
Effect of warm compresses on labor pain
The evaluation of labor pain by scores and when grouping pain levels showed a clear effect of warm compresses on pain relief. In most of the studies, pain scores in the warm group were significantly lower than in the control group (19,20). Similar findings were observed in pain severity studies: the warm compresses group had the majority of mild or moderate pain, while the control group had a higher percentage of severe pain (19,21-23,29). This result is consistent with the mechanism of action of passive vasodilation measures, which improve blood supply and temporarily block pain signals from reaching the brain (30). The results suggest that warm compresses can be used to relieve pain during the second phase of labor.
Effectiveness of warm compresses on perineal injuries
Most studies showed that warm compresses were associated with lower rates of perineal laceration. However, in a trial conducted by Akbarzadeh, the author reported a higher rate of perineal laceration in the warm compresses group without a specific discussion for this result (15). In some cases, applying warm compresses to the perineum might soften the tissue and make it less resilient, potentially increasing the likelihood of tearing during childbirth. Moreover, the warm compress used in Akbarzadeh’s study was put in water at 70oC; this temperature was much higher than most studies (usually ranging from 45 to 59oC). In summary, most of the intact perineum outcomes reported by the trials supported the use of warm compresses, as they helped maintain the perineum’s integrity during the second stage of labor.
The rate of perineum trauma that required suturing did not differ between the warm compresses group and the control group. Results on episiotomy rates between the two groups were also inconsistent: three out of eight trials showed that the warm compresses group had a significantly lower rate of perineal tear than the control group (18,22,29); five did not find the difference between groups (20,23,24,26,27). Besides, evidence for the effectiveness of warm compresses in reducing the severity of perineal trauma was either weak or not significantly different between the intervention group and the control group. Besides the methods applied during the delivery stages, other factors might have played a larger role in determining the perineal trauma status. These could include the size and position of the baby, or the mother's anatomy. In summary, warm compresses have been shown to be effective in reducing perineal trauma that does not require suturing and without perineal tears. Considerations should be made before applying this intervention for the purpose of reducing perineal tears or episiotomies during labor.
Limitations of the study
Quasi-experimental trials are included in this systematic review; they can introduce bias into the results. However, by carefully selecting trials and assessing the risk of bias in each study, such bias was minimized. Differences in the way the warm compresses were performed may also lead to heterogeneity and make it difficult to draw a uniform conclusion. However, the overall trend of the results among trials still supports the use of warm compresses in reducing labor pain and perineal trauma. Due to the lack of information from the selected trials, a meta-analysis was not performed in this review and may be considered in future research. This review excluded trials conducted in languages other than English; thus, a comprehensive approach to the topic may not be reached. It should also be noted that similar systematic reviews on the same topic have been conducted (17,31,32). However, with the addition of recently published trials, our review may provide more solid evidence for the effectiveness of warm compresses on pain and perineal outcomes during labor.
Conclusion
In conclusion, the use of warm compresses during the second stage of labor has been shown to be effective in lowering pain and perineal injuries without the need for suturing. Due to the mixed results found, considerations should be made before applying this method to reduce perineal tears or episiotomies during labor.
Acknowledgement
We thanked the University of Medicine and Pharmacy at Ho Chi Minh City for providing the funds for conducting this research.
Funding sources
The research received funding from the potential project of the University of Medicine and Pharmacy at Ho Chi Minh City digital contract 189/2021/HĐ - ĐHYD led by Dr. Nhan Thi Nguyen.
Ethical statement
Ethics Council in Biomedical Research, University of Medicine and Pharmacy at Ho Chi Minh City. No. 615/HDDD-DHYD signed on July 7, 2022.
Conflicts of interest
The authors declare that they have no competing interests.
Author contributions
All authors contributed to the writing of the manuscript and read and approved the final manuscript.
Type of study: Review Article |
Subject:
Midwifery
References
1. Lowe NK. The pain and discomfort of labor and birth. J Obstet Gynecol Neonatal Nurs. 1996;25(1):82-92. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Whitburn LY, Jones LE , Davey MA, McDonald S. The nature of labour pain: An updated review of the literature. Women Birth. 2019;32(1):28-38. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Sng BL ,Sia ATH . Maintenance of epidural labour analgesia: The old, the new and the future. Best Pract Res Clin Anaesthesiol 2017;31(1):15-22. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Sheen K, Slade P. Examining the content and moderators of women's fears for giving birth: A meta-synthesis. J Clin Nurs. 2018;27(13-14):2523-35. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Fenwick J, Toohill J, Creedy DK, Smith J, Gamble J. Sources, responses and moderators of childbirth fear in Australian women: A qualitative investigation. Midwifery. 2015;31(1):239-46. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Klomp T, Jonge A, Hutton EK, Hers S, Lagro-Janssen ALM. Perceptions of labour pain management of Dutch primary care midwives: a focus group study. BMC Pregnancy Childbirth. 2016;16(1):6. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Arfaie K, Nahidi F, Simbar M, Bakhtiari M. The role of fear of childbirth in pregnancy related anxiety in Iranian women: a qualitative research. Electron physician. 2017;9(2):3733-40. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Boateng EA, Kumi LO, Diji AKA. Nurses and midwives' experiences of using non-pharmacological interventions for labour pain management: A qualitative study in Ghana. BMC Pregnancy Childbirth. 2019;19(1):168. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Davim RM, Torres Gde V, Melo ES. Non-pharmacological strategies on pain relief during labor: pre-testing of an instrument. Rev Lat Am Enfermagem. 2007;15(6):1150-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. American College of Obstetricians and Gynecologists' Committee on Practice Bulletins-Obstetrics. Practice Bulletin No. 165: Prevention and Management of Obstetric Lacerations at Vaginal Delivery. Obstetrics and gynecology. 2016;128(1):e1-e15. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Friedman AM, Ananth CV, Prendergast E, D'Alton ME, Wright JD. Evaluation of third-degree and fourth-degree laceration rates as quality indicators. Obstet Gynecol. 2015;125(4):927-37. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Smith LA, Price N, Simonite V, Burns EE. Incidence of and risk factors for perineal trauma: a prospective observational study. BMC Pregnancy Childbirth. 2013;13:59. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. World Health Organization. WHO recommendations: intrapartum care for a positive childbirth experience. World Health Organization. 2018. [View at Publisher] [Google Scholar]
14. Dahlen HG, Homer CS, Cooke M, Upton AM, Nunn RA, Brodrick BS. Soothing the ring of fire: Australian women's and midwives experiences of using perineal warm packs in the second stage of labor. Midwifery. 2009;25(2):e39-48. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Akbarzadeh M, Vaziri F, Farahmand M, Masoudi Z, Amooee S, Zare N. The Effect of Warm Compress Bistage Intervention on the Rate of Episiotomy, Perineal Trauma, and Postpartum Pain Intensity in Primiparous Women with Delayed Valsalva Maneuver Referring to the Selected Hospitals of Shiraz University of Medical Sciences in 2012-2013. Adv Skin Wound Care. 2016;29(2):79-84. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Albers LL, Borders N. Minimizing genital tract trauma and related pain following spontaneous vaginal birth. J Midwifery Womens Health. 2007;52(3):246-53. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Magoga G, Saccone G, Al-Kouatly HB, Dahlen GH, Thornton C, Akbarzadeh M, et al. Warm perineal compresses during the second stage of labor for reducing perineal trauma: A meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2019;240:93-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Alihosseni F, Abedi P, Afshary P, Haghighi MR, Hazeghi N. Investigating the Effect of Perineal Heating Pad on the Frequency of Episiotomies and Perineal Tears in Primiparous Females. Med Surg Nurs J. 2018;7(1):e82588. [View at Publisher] [DOI] [Google Scholar]
19. Farahmand M, Khooshab E, Hasanzadeh F, Sedigheh Amooee S, Akbarzadeh M. The Effect of Warm Compress Bi-stage on Pain Strength in Labor Stages and After Delivery. International Journal of Women's Health and Reproduction Sciences. 2020;8(1):46-52. [View at Publisher] [DOI] [Google Scholar]
20. Ganji Z, Shirvani MA, Rezaei-Abhari F, Danesh M. The effect of intermittent local heat and cold on labor pain and child birth outcome. Iran J Nurs Midwifery Res. 2013;18(4):298-303. [View at Publisher] [PMID] [Google Scholar]
21. Sondakh JJS. Warm Pad Reduces Anxiety, Somatic Pain, Strain Pain, Perineal Rupture and Post Partum Blood Volume in Normal Delivery (with Normal Baby Weight Range). Itnernational Journal of Innovative Science and Research Technology. 2022;3(10):571-9. [View at Publisher] [Google Scholar]
22. Modoor S, Fouly H, Rawas H. The effect of warm compresses on perineal tear and pain intensity during the second stage of labor: A randomized controlled trial. Belitung Nurs J. 2021;7(3):210-8. [View at paplisher] [DOI] [PMID] [Google Scholar]
23. Ibrahim HA, Elgzar WTI, Hassan HE. Effect of Warm Compresses Versus Lubricated Massage during the Second Stage of Labor on Perineal Outcomes among Primiparous Women. IOSR Journal of Nursing and Health Science. 2017;6(4):64-76. [View at paplisher] [DOI] [Google Scholar]
24. Mohamed ML, Mohamed SL, Gonied AS. Comparative Study between Two Perineal Management Techniques Used to Reduce Perineal Trauma during 2nd Stage of Labor. J Am Sci. 2011;7(11):228-32. [View at paplisher] [Google Scholar]
25. Thenu U, Irianta T, Madya F, Sunarno I, Lotisna D, Farid RB. Perineal Warm Compresses During the Second Stage of Labour Decrease Incidence and Degree of Perineal Laceration in Primiparous. Gynecol Reprod Health. 2019;3(2):1-6. [View at paplisher] [DOI] [Google Scholar]
26. Albers LL, Sedler KD, Bedrick EJ, Teaf D, Peralta P. Midwifery Care Measures in the Second Stage of Labor and Reduction of Genital Tract Trauma at Birth: A Randomized Trial. J Midwifery Womens Health. 2005;50(5):365-72. [View at paplisher] [DOI] [PMID] [Google Scholar]
27. Dahlen HG, Homer CSE, Cooke M, Upton AM, Rosalie Nunn R, Brodrick B. Perineal Outcomes and Maternal Comfort Related to the Application of Perineal Warm Packs in the Second Stage of Labor: A Randomized Controlled Trial. Birth. 2007;34(4):282-90. [View at paplisher] [DOI] [PMID] [Google Scholar]
28. Turkmen H, Oran NT. Massage and heat application on labor pain and comfort: A quasirandomized controlled experimental study. Explore (NY). 2021;17(5):438-45. [View at paplisher] [DOI] [PMID] [Google Scholar]
29. Essa RM, Ismail NIAA. Effect of second stage perineal warm compresses on perineal pain and outcome among primiparae. Journal of Nursing Education and Practice. 2016;6(4):48-58. [View at paplisher] [DOI] [Google Scholar]
30. Porth CM. Pathophysiology-Concepts of altered health states. 3rd ed. Philadelphia: JB Lippincott Company;2005. [View at paplisher] [Google Scholar]
31. Fadlalmola H, Abdelmalik MA, Masaad HKH, Abdalla AM, Mohammaed MO, Abbakr I, et al. Efficacy of warm compresses in preserving perineal integrity and decreasing pain during normal labor: A systematic review and meta-analysis. Afr J Reprod Health. 2023;27(4):96-123. [View at paplisher] [DOI] [PMID] [Google Scholar]
32. Aasheim V, Nilsen ABV, Reinar LM, Lukasse M. Perineal techniques during the second stage of labour for reducing perineal trauma. Cochrane Database Syst Rev. 2017;6(6):CD006672. [View at paplisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






