Volume 20, Issue 2 (10-2023)
J Res Dev Nurs Midw 2023, 20(2): 9-13 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Aydemir A, Esenkaya D. Frequency of urinary incontinence in women, risk factors, and effect of incontinence on quality of life: A cross-sectional study on the Turkish population. J Res Dev Nurs Midw 2023; 20 (2) :9-13
URL: http://nmj.goums.ac.ir/article-1-1571-en.html
URL: http://nmj.goums.ac.ir/article-1-1571-en.html
1- Nursing, Faculty of Health Sciences, Giresun University, Giresun, Türkiye , azizeaydemir@hotmail.com
2- Nursing, Yozgat Bozok University, Yozgat, Türkiye
2- Nursing, Yozgat Bozok University, Yozgat, Türkiye
Full-Text [PDF 447 kb]
(853 Downloads)
| Abstract (HTML) (1718 Views)
Full-Text: (294 Views)
Introduction
Involuntary urinary incontinence (UI), as defined by the International Continence Society, refers to a lower urinary system dysfunction that can be objectively demonstrated and leads to social and hygienic challenges. Urinary incontinence has a prevalence rate of 20%-30% among adults, affecting both genders, with a higher incidence in women (1). Urinary incontinence is a distressing condition (2).
It is documented that the frequency of UI tends to rise during pregnancy (3). Studies have shown that regular and gradual pelvic floor muscle training over a 3-month period can be beneficial in preventing UI (2). However, many women continue to believe that there is no solution to UI, exacerbating the severity of the problem and transforming it into a significant health issue.
Although UI is not life-threatening, it is a common health problem that impacts women's physical, social, work, and educational activities, ultimately reducing their overall quality of life (QOL). Urinary incontinence negatively affects various aspects of a woman's life and is often perceived as an embarrassing flaw, leading to psychosocial suffering. Women may experience feelings of inadequacy, incompleteness, and undesirability, coupled with a belief that their attractiveness and sexual confidence have diminished. The fear of inadequate hygiene further increases their sense of shame, resulting in social isolation. This distortion in body image frequently contributes to heightened anxiety and depression.
Early intervention is crucial to address the UI problem before it becomes chronic. However, women commonly refrain from discussing this issue, downplay its significance, or attribute it to aging, hindering early diagnosis (4). Identifying risk factors for UI development is a key objective in preventing this prevalent and distressing condition.
Some studies in the literature suggest that pregnancy, vaginal delivery, and the number of vaginal deliveries elevate the frequency of UI (5,6), while others emphasize that vaginal delivery poses a greater risk for UI compared to cesarean section delivery (6,7). This study aimed to determine the frequency of UI among women attending the Obstetrics Outpatient Clinic of a hospital, elucidate the connection between UI and factors such as delivery method, number of births, curettage, and miscarriage, and evaluate the impact of UI on QOL.
To achieve these goals, 2 measurement tools were used in the study. Both tools encompass inquiries about UI-related complaints and QOL. Unlike other scales, these instruments allow the evaluation of UI severity and its effect on QOL by analyzing participants' responses to questions regarding UI, daily life, and psychosocial aspects. The outcomes of this research may provide guidance to health care professionals, particularly those involved in preventive health care services. The identification of UI risk factors may enable the development of individualized care plans, enhancing the quality of care provided by nurses and midwives.
Methods
This analytical, cross-sectional study adhered to the principles of the Declaration of Helsinki. Approval for the study was obtained from the Yozgat Bozok University Ethics Committee (decision No. 34/17; decision date: 24.06.2022).
The research involved women over the age of 20 who were admitted to the Obstetrics Clinic of a hospital between June 21, 2022, and August 15, 2022, for reasons other than pregnancy. The research did not employ a sample selection process, and all eligible women who visited the outpatient clinic during the 2-month study period were included. A total of 300 volunteer women participated in the study. Data collection was performed in person by the researcher between 09:00 and 17:00 when the Gynecology and Obstetrics Polyclinic was actively operating. Data collection took place on Tuesdays, Wednesdays, and Thursdays and was conducted by the same researcher. Before initiating data collection, participants were informed about the study, and their written and verbal consent was obtained.
Exclusion criteria for the study included individuals under the age of 20, pregnant women, those who had experienced childbirth, miscarriage, or curettage within the past 6 months, individuals who had undergone hysterectomy or pelvic reconstruction surgeries such as colporrhaphy anterior/posterior, sacrospinous fixation, or sacral colpopexy, participants who were unwilling to continue participating in the research, those with spinal cord injuries, individuals with a history of cerebrovascular accidents, those afflicted with conditions causing neurogenic bladder dysfunction such as multiple sclerosis, and individuals diagnosed with diseases like dementia and Alzheimer disease that impact mental health.
Data collection tools
Data collection was carried out using the Descriptive Characteristics Form, consisting of questions about sociodemographic characteristics (eg, age, education level, etc), International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF), and Wagner QOL Scale.
Descriptive characteristics form
The Descriptive Characteristics Form, developed based on the literature, comprises 8 questions aimed at eliciting the descriptive characteristics of the participants, including body mass index (BMI), age, occupation, level of education, marital status, place of residence, presence of chronic illness, menstrual cycle, number of pregnancies, type of delivery (none, vaginal, cesarean section, Vaginal/cesarean section, miscarriage, curettage), and fecal incontinence.
International Consultation on Incontinence Questionnaire-Short Form
The ICIQ-SF was used to assess the severity and frequency of UI among the participants. The validity and reliability of the ICIQ-SF were confirmed by Çetinel et al (7). This questionnaire includes 3 aspects, addressing the frequency of UI, impact of UI on daily life, and situations that cause UI. It consists of a total of 6 questions. The first 2 questions inquire about the date of birth and gender. The third question assesses the frequency of UI, with a score ranging from 0 to 5. The fourth question examines the quantity of UI, with a score ranging from 0 to 6. The fourth factor is not scored, as it is used to determine the type of UI based on individual complaints. Higher scores indicate a lower QOL and increased severity of UI. The fifth question uses the Visual Analog Scale, ranging from 0 (not at all) to 10 (a great deal), to inquire how much UI affects individuals' daily lives. The maximum score achievable on the questionnaire is 21, with higher scores indicating a reduced QOL. In the Turkish population, Çetinel et al reported a Cronbach α value of 0.71 for the questionnaire. In this study, the Cronbach α value of the scale was determined to be 0.88 among the female participants.
Wagner QOL Scale
In this study, the impact of UI on the QOL was assessed using the Wagner QOL scale, which consists of 28 items evaluating UI, daily life, and psychosocial effects. These items are rated on a 4-point scale (0, no; 1, mild; 2, moderate; and 3, severe). A total score of 0 indicates no UI and no psychological impairment. Scores between 1-28, 29-56, and 57-84 indicate mild, moderate, and severe UI and psychological impairment, respectively (8). The scale used was adopted from the study of Karan et al (9). Its validity and reliability in Turkish were confirmed by Özerdoğan (10). In this study, the Cronbach α value of the scale was determined to be 0.98.
Data analysis
Power analysis was conducted using G*Power version 3.1.9.2, based on the results of the ICIQ-SF variables. A power of 90.74% was determined with an effect size of 0.86 and type I error of 0.05. In the analysis of the participants' sociodemographic characteristics, frequency, percentage, mean, and SD were calculated. For normally distributed data, an independent samples t test was used for 2 groups, and a 1-way analysis of variance (ANOVA) test was used for 3 or more groups as parametric tests. When the data were not normally distributed, the Mann-Whitney U test was used for 2 groups, and the Kruskal-Wallis test was used for 3 or more groups. To determine whether there was a statistically significant relationship between the variables, the Spearman correlation test was used. Logistic regression analysis was performed to assess the impact of potential risk factors for UI identified through this test. The results were analyzed using a 95% CI. All statistical analyses were conducted using SPSS version 25 (SPSS Inc, Chicago, IL, USA). P values less than 0.05 were considered statistically significant.
Results
The mean age of the participants was 41.2 ± 13.49 years, and they were
categorized as overweight based on their mean BMIs. Among the participants, 53.3% were housewives, and 31% were health workers. Regarding education, 42.3% of the participants were primary school graduates, while 37.3% were university graduates. Furthermore, 77.7% were married, and 48% live in a town. Approximately 50.7% of the participants reported having a regular menstrual cycle, 28.3% were in menopause, and 67% had chronic diseases. Concerning childbirth, 53.3% had only vaginal deliveries, 26% had never given birth, 14% had only undergone cesarean sections, and 6.7% had experienced both vaginal and cesarean section deliveries. Additionally, 6% reported fecal incontinence, while 48% had UI based on the ICIQ-SF score, and 62% had UI according to the QOL score. The mean scores for QOL and ICIQ-SF indicated that the participants experienced mild UI and psychosocial impairment (Table 1).
A significant finding is that participants with ideal body weight, bachelor degree, single marital status, no chronic diseases, regular menstrual cycle, and no fecal incontinence had lower ICIQ-SF scores than other groups (P = 0.000). Furthermore, women aged 20-29 had lower ICIQ-SF scores than all other age groups, and those aged 30-39 had lower ICIQ-SF scores than those aged 40-59 (P = 0.000). Another significant finding is that the ICIQ-SF scores were higher among housewives (P = 0.000) and those who live in villages (P = 0.011). Additionally, ICIQ-SF scores were lower among those who never had vaginal deliveries compared to those who had (P = 0.000; Table 1).
Comparison of some characteristics of women with UI (n = 156) and total ICIQ-SF Scores
The mean scores of ICIQ-SF and QOL for those with UI indicated that the participants experienced moderate UI and psychosocial impairment. The mean age of women with UI was 48.7 years, and they were categorized as obese based on their BMIs. Among the participants, 80.1% were housewives, and 16% were health workers. Additionally, 65.4% had primary school education, while 12.8% were university graduates. Most of the women with UI had not undergone cesarean sections, and 15.4% had not experienced vaginal deliveries. Among those who had vaginal deliveries, 8.4% had one, 15.9% had two, 34.8% had three, 22.7% had four, 8.4% had five, and 9.8% had six or more births. The highest frequency of UI was observed in women with natural childbirth, followed by those with cesarean section and women without childbirth. Furthermore, 38.5% of the participants had experienced at least 1 miscarriage, while 23.7% had undergone at least 1 curettage. Notably, 6% of the participants had both fecal incontinence and UI. The impact of UI on QOL was found to be mild in 19.2% of participants, moderate in 4%, severe in 32.7%, and very severe in 7.1% (Table 1).
Significantly, the ICIQ-SF total scores of overweight women with UI were lower than those of obese and extremely obese women, and the QOL total scores of women with an ideal weight were lower than those of obese and extremely obese women (P = 0.000). Another notable finding is that women aged 40-49 had higher ICIQ-SF total scores than other age groups (P = 0.000). Additionally, the ICIQ-SF total scores were lower among health care workers (P = 0.003), those with a university degree (P = 0.041), and those who did not have vaginal delivery (P = 0.034), experienced miscarriage (P = 0.000), or had curettage (P = 0.026) compared to other groups. It was observed that individuals with mild and moderate UI had lower QOL total scores than those with severe and very severe UI (P = 0.000). Furthermore, no relationship was found between ICIQ-SF total score and number of vaginal deliveries, undergoing cesarean section, and type of delivery, as well as between QOL total score and age, occupation, education level, vaginal delivery, number of vaginal deliveries, undergoing cesarean section, type of delivery, or experiencing a miscarriage, curettage, or fecal incontinence (P > 0.05; Table 1).
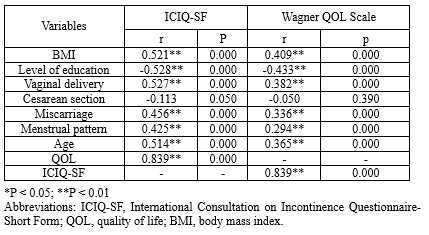
A very strong relationship was identified between the ICIQ-SF and the QOL scores. In terms of the ICIQ-SF score, a strong relationship was observed between UI severity, its impact on QOL, and factors such as BMI, education level, having a vaginal delivery, and age. Moreover, a moderate relationship was found between UI severity, its effect on QOL, and factors such as miscarriage and menstrual cycle. Conversely, no significant relationship was detected between UI severity, its influence on QOL, and having a cesarean section (P > 0.05). According to the QOL score, a moderate relationship was observed between UI severity, QOL, and factors such as education level, BMI, vaginal delivery, age, and miscarriage. A weaker relationship was noted between UI severity, QOL, and menstrual cycle, while no apparent relationship was found between UI severity, QOL, and having a cesarean section (P > 0.05; Table 2).
A logistic regression analysis was conducted to assess the effects of independent variables, including BMI, miscarriage, education level, and age, on the occurrence of UI in women. The analysis demonstrated that these independent variables—BMI, miscarriage, education level, and age—accounted for 52.2% of the variance in the UI variable (R2nagelkerke = 0.522). The odds of experiencing UI were found to be 3.1 times higher in women who had a history of miscarriage compared to those who did not. Additionally, women with a primary school education were 3.2 times more likely to develop UI than those with a high school or university education. Furthermore, older women were 1.0 times more likely to have UI than younger women (P < 0.05). Consequently, it can be concluded that the likelihood of UI is higher in women of older age, those with primary school education, and those who have experienced miscarriages (Table 3).
Involuntary urinary incontinence (UI), as defined by the International Continence Society, refers to a lower urinary system dysfunction that can be objectively demonstrated and leads to social and hygienic challenges. Urinary incontinence has a prevalence rate of 20%-30% among adults, affecting both genders, with a higher incidence in women (1). Urinary incontinence is a distressing condition (2).
It is documented that the frequency of UI tends to rise during pregnancy (3). Studies have shown that regular and gradual pelvic floor muscle training over a 3-month period can be beneficial in preventing UI (2). However, many women continue to believe that there is no solution to UI, exacerbating the severity of the problem and transforming it into a significant health issue.
Although UI is not life-threatening, it is a common health problem that impacts women's physical, social, work, and educational activities, ultimately reducing their overall quality of life (QOL). Urinary incontinence negatively affects various aspects of a woman's life and is often perceived as an embarrassing flaw, leading to psychosocial suffering. Women may experience feelings of inadequacy, incompleteness, and undesirability, coupled with a belief that their attractiveness and sexual confidence have diminished. The fear of inadequate hygiene further increases their sense of shame, resulting in social isolation. This distortion in body image frequently contributes to heightened anxiety and depression.
Early intervention is crucial to address the UI problem before it becomes chronic. However, women commonly refrain from discussing this issue, downplay its significance, or attribute it to aging, hindering early diagnosis (4). Identifying risk factors for UI development is a key objective in preventing this prevalent and distressing condition.
Some studies in the literature suggest that pregnancy, vaginal delivery, and the number of vaginal deliveries elevate the frequency of UI (5,6), while others emphasize that vaginal delivery poses a greater risk for UI compared to cesarean section delivery (6,7). This study aimed to determine the frequency of UI among women attending the Obstetrics Outpatient Clinic of a hospital, elucidate the connection between UI and factors such as delivery method, number of births, curettage, and miscarriage, and evaluate the impact of UI on QOL.
To achieve these goals, 2 measurement tools were used in the study. Both tools encompass inquiries about UI-related complaints and QOL. Unlike other scales, these instruments allow the evaluation of UI severity and its effect on QOL by analyzing participants' responses to questions regarding UI, daily life, and psychosocial aspects. The outcomes of this research may provide guidance to health care professionals, particularly those involved in preventive health care services. The identification of UI risk factors may enable the development of individualized care plans, enhancing the quality of care provided by nurses and midwives.
Methods
This analytical, cross-sectional study adhered to the principles of the Declaration of Helsinki. Approval for the study was obtained from the Yozgat Bozok University Ethics Committee (decision No. 34/17; decision date: 24.06.2022).
The research involved women over the age of 20 who were admitted to the Obstetrics Clinic of a hospital between June 21, 2022, and August 15, 2022, for reasons other than pregnancy. The research did not employ a sample selection process, and all eligible women who visited the outpatient clinic during the 2-month study period were included. A total of 300 volunteer women participated in the study. Data collection was performed in person by the researcher between 09:00 and 17:00 when the Gynecology and Obstetrics Polyclinic was actively operating. Data collection took place on Tuesdays, Wednesdays, and Thursdays and was conducted by the same researcher. Before initiating data collection, participants were informed about the study, and their written and verbal consent was obtained.
Exclusion criteria for the study included individuals under the age of 20, pregnant women, those who had experienced childbirth, miscarriage, or curettage within the past 6 months, individuals who had undergone hysterectomy or pelvic reconstruction surgeries such as colporrhaphy anterior/posterior, sacrospinous fixation, or sacral colpopexy, participants who were unwilling to continue participating in the research, those with spinal cord injuries, individuals with a history of cerebrovascular accidents, those afflicted with conditions causing neurogenic bladder dysfunction such as multiple sclerosis, and individuals diagnosed with diseases like dementia and Alzheimer disease that impact mental health.
Data collection tools
Data collection was carried out using the Descriptive Characteristics Form, consisting of questions about sociodemographic characteristics (eg, age, education level, etc), International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF), and Wagner QOL Scale.
Descriptive characteristics form
The Descriptive Characteristics Form, developed based on the literature, comprises 8 questions aimed at eliciting the descriptive characteristics of the participants, including body mass index (BMI), age, occupation, level of education, marital status, place of residence, presence of chronic illness, menstrual cycle, number of pregnancies, type of delivery (none, vaginal, cesarean section, Vaginal/cesarean section, miscarriage, curettage), and fecal incontinence.
International Consultation on Incontinence Questionnaire-Short Form
The ICIQ-SF was used to assess the severity and frequency of UI among the participants. The validity and reliability of the ICIQ-SF were confirmed by Çetinel et al (7). This questionnaire includes 3 aspects, addressing the frequency of UI, impact of UI on daily life, and situations that cause UI. It consists of a total of 6 questions. The first 2 questions inquire about the date of birth and gender. The third question assesses the frequency of UI, with a score ranging from 0 to 5. The fourth question examines the quantity of UI, with a score ranging from 0 to 6. The fourth factor is not scored, as it is used to determine the type of UI based on individual complaints. Higher scores indicate a lower QOL and increased severity of UI. The fifth question uses the Visual Analog Scale, ranging from 0 (not at all) to 10 (a great deal), to inquire how much UI affects individuals' daily lives. The maximum score achievable on the questionnaire is 21, with higher scores indicating a reduced QOL. In the Turkish population, Çetinel et al reported a Cronbach α value of 0.71 for the questionnaire. In this study, the Cronbach α value of the scale was determined to be 0.88 among the female participants.
Wagner QOL Scale
In this study, the impact of UI on the QOL was assessed using the Wagner QOL scale, which consists of 28 items evaluating UI, daily life, and psychosocial effects. These items are rated on a 4-point scale (0, no; 1, mild; 2, moderate; and 3, severe). A total score of 0 indicates no UI and no psychological impairment. Scores between 1-28, 29-56, and 57-84 indicate mild, moderate, and severe UI and psychological impairment, respectively (8). The scale used was adopted from the study of Karan et al (9). Its validity and reliability in Turkish were confirmed by Özerdoğan (10). In this study, the Cronbach α value of the scale was determined to be 0.98.
Data analysis
Power analysis was conducted using G*Power version 3.1.9.2, based on the results of the ICIQ-SF variables. A power of 90.74% was determined with an effect size of 0.86 and type I error of 0.05. In the analysis of the participants' sociodemographic characteristics, frequency, percentage, mean, and SD were calculated. For normally distributed data, an independent samples t test was used for 2 groups, and a 1-way analysis of variance (ANOVA) test was used for 3 or more groups as parametric tests. When the data were not normally distributed, the Mann-Whitney U test was used for 2 groups, and the Kruskal-Wallis test was used for 3 or more groups. To determine whether there was a statistically significant relationship between the variables, the Spearman correlation test was used. Logistic regression analysis was performed to assess the impact of potential risk factors for UI identified through this test. The results were analyzed using a 95% CI. All statistical analyses were conducted using SPSS version 25 (SPSS Inc, Chicago, IL, USA). P values less than 0.05 were considered statistically significant.
Results
The mean age of the participants was 41.2 ± 13.49 years, and they were
categorized as overweight based on their mean BMIs. Among the participants, 53.3% were housewives, and 31% were health workers. Regarding education, 42.3% of the participants were primary school graduates, while 37.3% were university graduates. Furthermore, 77.7% were married, and 48% live in a town. Approximately 50.7% of the participants reported having a regular menstrual cycle, 28.3% were in menopause, and 67% had chronic diseases. Concerning childbirth, 53.3% had only vaginal deliveries, 26% had never given birth, 14% had only undergone cesarean sections, and 6.7% had experienced both vaginal and cesarean section deliveries. Additionally, 6% reported fecal incontinence, while 48% had UI based on the ICIQ-SF score, and 62% had UI according to the QOL score. The mean scores for QOL and ICIQ-SF indicated that the participants experienced mild UI and psychosocial impairment (Table 1).
A significant finding is that participants with ideal body weight, bachelor degree, single marital status, no chronic diseases, regular menstrual cycle, and no fecal incontinence had lower ICIQ-SF scores than other groups (P = 0.000). Furthermore, women aged 20-29 had lower ICIQ-SF scores than all other age groups, and those aged 30-39 had lower ICIQ-SF scores than those aged 40-59 (P = 0.000). Another significant finding is that the ICIQ-SF scores were higher among housewives (P = 0.000) and those who live in villages (P = 0.011). Additionally, ICIQ-SF scores were lower among those who never had vaginal deliveries compared to those who had (P = 0.000; Table 1).
Comparison of some characteristics of women with UI (n = 156) and total ICIQ-SF Scores
The mean scores of ICIQ-SF and QOL for those with UI indicated that the participants experienced moderate UI and psychosocial impairment. The mean age of women with UI was 48.7 years, and they were categorized as obese based on their BMIs. Among the participants, 80.1% were housewives, and 16% were health workers. Additionally, 65.4% had primary school education, while 12.8% were university graduates. Most of the women with UI had not undergone cesarean sections, and 15.4% had not experienced vaginal deliveries. Among those who had vaginal deliveries, 8.4% had one, 15.9% had two, 34.8% had three, 22.7% had four, 8.4% had five, and 9.8% had six or more births. The highest frequency of UI was observed in women with natural childbirth, followed by those with cesarean section and women without childbirth. Furthermore, 38.5% of the participants had experienced at least 1 miscarriage, while 23.7% had undergone at least 1 curettage. Notably, 6% of the participants had both fecal incontinence and UI. The impact of UI on QOL was found to be mild in 19.2% of participants, moderate in 4%, severe in 32.7%, and very severe in 7.1% (Table 1).
Significantly, the ICIQ-SF total scores of overweight women with UI were lower than those of obese and extremely obese women, and the QOL total scores of women with an ideal weight were lower than those of obese and extremely obese women (P = 0.000). Another notable finding is that women aged 40-49 had higher ICIQ-SF total scores than other age groups (P = 0.000). Additionally, the ICIQ-SF total scores were lower among health care workers (P = 0.003), those with a university degree (P = 0.041), and those who did not have vaginal delivery (P = 0.034), experienced miscarriage (P = 0.000), or had curettage (P = 0.026) compared to other groups. It was observed that individuals with mild and moderate UI had lower QOL total scores than those with severe and very severe UI (P = 0.000). Furthermore, no relationship was found between ICIQ-SF total score and number of vaginal deliveries, undergoing cesarean section, and type of delivery, as well as between QOL total score and age, occupation, education level, vaginal delivery, number of vaginal deliveries, undergoing cesarean section, type of delivery, or experiencing a miscarriage, curettage, or fecal incontinence (P > 0.05; Table 1).
A very strong relationship was identified between the ICIQ-SF and the QOL scores. In terms of the ICIQ-SF score, a strong relationship was observed between UI severity, its impact on QOL, and factors such as BMI, education level, having a vaginal delivery, and age. Moreover, a moderate relationship was found between UI severity, its effect on QOL, and factors such as miscarriage and menstrual cycle. Conversely, no significant relationship was detected between UI severity, its influence on QOL, and having a cesarean section (P > 0.05). According to the QOL score, a moderate relationship was observed between UI severity, QOL, and factors such as education level, BMI, vaginal delivery, age, and miscarriage. A weaker relationship was noted between UI severity, QOL, and menstrual cycle, while no apparent relationship was found between UI severity, QOL, and having a cesarean section (P > 0.05; Table 2).
A logistic regression analysis was conducted to assess the effects of independent variables, including BMI, miscarriage, education level, and age, on the occurrence of UI in women. The analysis demonstrated that these independent variables—BMI, miscarriage, education level, and age—accounted for 52.2% of the variance in the UI variable (R2nagelkerke = 0.522). The odds of experiencing UI were found to be 3.1 times higher in women who had a history of miscarriage compared to those who did not. Additionally, women with a primary school education were 3.2 times more likely to develop UI than those with a high school or university education. Furthermore, older women were 1.0 times more likely to have UI than younger women (P < 0.05). Consequently, it can be concluded that the likelihood of UI is higher in women of older age, those with primary school education, and those who have experienced miscarriages (Table 3).
Table 1. Comparison of women's (n = 300) and women with urinary incontinence’s (n = 156) sociodemographic characteristics and ICIQ-SF total scores 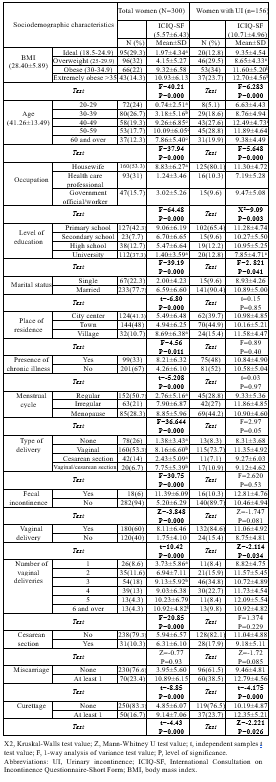 |
|
Table 2. The relationship between urinary incontinence and some characteristics of women (N = 300)
 |
|
Table 3. Logistic regression analysis of factors affecting the frequency of urinary incontinence in women (N = 300)
 |
Discussion
Urinary incontinence is a prevalent and significant health issue affecting women globally. This study aimed to investigate the frequency of UI, its risk factors, and its impact on QOL among women living in Yozgat Province, situated in the Central Anatolian region of Turkey, which has a larger rural population. The severity of UI and associated risks were analyzed based on the ICIQ-SF scores, while the assessment of QOL relied on the Wagner QOL Scale scores.
Frequency of UI in women
Among women aged 20 and older who sought care at the Training and Research Hospital Obstetrics and Gynecology outpatient clinic in Yozgat for reasons other than pregnancy follow-up, the prevalence of UI was 48% according to the ICIQ-SF and 62% according to the Wagner QOL Scale. Previous studies conducted in Turkey have reported UI frequency rates ranging from 21.3% to 86.7% among women (3,11). The frequency of UI reported worldwide in the last 5 years is 41.7% among women aged 20 and over in Singapore (6), 31.2% among women aged 20 and over in China (12), 45.1% among professional female athletes in Spain (13), 30.5% among women in Congo (14), 43% among Muslim women aged 18-75 in Israel (15), 63% among women aged 15-80 in Iran (16), and 41% among women over 65 years old in Uganda (17). Despite variations in geography, language, culture, customs, and traditions, UI remains a universal health concern for women. The literature suggests that differences in UI frequency among women are primarily attributed to distinct sociocultural, demographic, and economic factors associated with their respective regions.
Urinary incontinence risk factors in women
Urinary incontinence among women is a complex health issue influenced by multiple factors, as evidenced by studies conducted in the past decade. Demir et al identified risk factors for UI, including hypertension, diabetes mellitus, multiparity, higher BMI, and low education levels (18). Daneshpajooh et al found that age, higher BMI, pregnancy, diabetes, anxiety, and depression were associated with UI (5). Maroyi et al linked UI in postpartum women to a history of episiotomy and the delivery of large babies (14). Treister-Goltzman and Peleg reported a relationship between higher BMI and polygamy with severe and very severe UI (15). Yağmur and Gül highlighted the relationship between UI and factors such as age, education level, employment status, presence of chronic diseases, chronic constipation, history of difficult deliveries, and menopause (19). Luo et al, through multivariate logistic regression analysis, determined that older women with a history of vaginal delivery who were sexually active were more likely to experience UI (6).
Consistent with our results, previous studies have shown that UI is influenced by various factors, including age, polygamy, education level, employment status, obesity, number of births, episiotomy history, history of delivering large babies, menopause, anxiety, depression, constipation, history of difficult deliveries, vaginal delivery, sexual activity, and chronic diseases such as diabetes and hypertension. Our logistic regression analysis, which included BMI, miscarriage, education level, and age as variables, revealed that these factors accounted for 52.2% of the variance in UI frequency. Specifically, the analysis showed that a 1-unit increase in the miscarriage variable increased the likelihood of UI by 3.1 times, 1-unit increase in the primary school graduate variable increased the likelihood by 3.2 times, and 1-unit increase in the age variable increased the likelihood by 1.0 times. Therefore, it can be concluded that the probability of experiencing UI is higher among older women, those with primary school education, and those who have a history of miscarriages.
Our study highlights the significance of education once again. Educated women tend to play active roles in social and economic spheres, actively seeking early and efficient solutions to problems that might hinder their lifestyle. On the other hand, many uneducated women, particularly those living in rural areas, may avoid seeking treatment, regarding UI as a private matter and attributing it to the natural aging process. This tendency can lead to an increase in the severity of UI and a reduction in the overall QOL. Nearly half of the study participants were found to experience UI, possibly linked to the fact that 50% of them had only completed primary school education.
To the best of our knowledge, the finding that a 1-unit increase in the miscarriage variable increases the likelihood of UI by 3.1 times is a new finding in the literature. Existing research indicates that the frequency of UI is higher in women who have experienced miscarriages. However, it remains unclear whether UI serves as a predictor of the likelihood of miscarriage or if women who have experienced miscarriages face an increased risk of UI. Consequently, it is thought that comprehensive studies are necessary to elucidate the relationship between miscarriage and UI.
The effect of UI on women's QOL
Both measurement tools used in this research demonstrate that an increase in the severity of UI has a detrimental effect on the QOL. Yağmur and Gül found that UI moderately affected the QOL (19). Similarly, our study revealed that psychosocial impairment was moderate among women with UI. The moderate level of discomfort perceived by women with UI suggests that they may be relatively indifferent to this issue. This result might be influenced by the fact that 75% of the participants with UI in our study had either primary or secondary school education. It is conceivable that lower levels of education limit the search for solutions, and the belief that the problem is unsolvable strengthens the perception of destiny.
Numerous studies have consistently reported that higher BMI is associated with a higher frequency of UI and poor QOL (15,18,19). However, our study showed that the severity of UI in overweight women was less than that of obese and extremely obese women, and as a result, their QOL was affected less. This difference may be attributed to the fact that overweight women had lower intra-abdominal pressure than obese and extremely obese women, potentially resulting in a lower frequency of stress-type UI, which in turn could have a less significant impact on their QOL. Paradoxically, women with an ideal weight exhibited more severe UI and a lower QOL than obese women. This phenomenon could be explained by the negative impact of UI on body image among women with an ideal weight, potentially making them more vulnerable to the effects of UI on their overall well-being.
In light of our findings, it is evident that UI affects women across all age groups. However, the severity of the problem and its impact on QOL seem to be more pronounced in women aged 40-59. This observation is consistent with the majority of studies in the literature that emphasize the relationship between UI and age (3,6). While UI tends to peak in the age range of 40-49 years, it has been noted that the severity of UI decreases and QOL improves as age progresses, particularly in the age group of 60 and over. This shift may be attributed to the perception among women that UI is a natural consequence of aging, potentially reducing the psychological impact of UI on their overall QOL.
Limitations
This study has several limitations. First, it is a cross-sectional study conducted within a single health care facility involving a specific patient population, which could potentially limit the generalizability of the findings to broader populations. Second, as an outpatient clinic-based study, the characteristics of the study population may not fully represent the general population. The third limitation is that the presence of UI is based on subjective data collected using 2 scales, not objective methods. Lastly, the relatively small sample size may have limited the precision of some comparisons.
Conclusion
Miscarriage, aging, and low education levels are risk factors for UI. As the severity of UI increases, the QOL of affected individuals decreases. Early diagnosis is crucial, as the problem can be solved more quickly, and the QOL of women can be preserved. Health care professionals play a pivotal role in raising awareness among women about UI. Specifically, nurses and midwives can provide valuable discharge training for at-risk groups, and preventive health care providers can identify these groups early on to effectively address the problem. There is a pressing need for more effective policies to increase the education level of women. Moreover, practical solutions are required to enhance women's physical mobility. Collaborative efforts involving health authorities, local governments, and private enterprises can promote physical activity, potentially reducing a range of sedentary lifestyle-related issues, including UI, which, in turn, may contribute to cost savings in health care expenditures.
Acknowledgement
We would like to express our gratitude to Internal Medicine Specialist Dr Reşat Ferhan PAKİZ for his invaluable support and assistance throughout the research.
Funding sources
This study received no funding.
Ethical statement
The research received approval from the Yozgat Bozok University Ethics Committee (decision No. 34/17; decision date: 24.06.2022). The study adhered to the principles outlined in the Declaration of Helsinki. Participants were provided with a clear explanation of the study's purpose, and their informed verbal and written consent was obtained.
Conflicts of interest
The authors declare no conflicts of interest.
Author contributions
All listed authors meet the authorship criteria, and all authors are in agreement with the content of the manuscript.
Conceptualization: A.A. and D.E.
Research design: A.A. and D.E.
Data collection and processing: A.A. and D.E.
Analysis and interpretation: A.A.
Literature review: A.A. and D.E.
Original draft preparation: A.A.
Review and editing: A.A. and D.E.
Urinary incontinence is a prevalent and significant health issue affecting women globally. This study aimed to investigate the frequency of UI, its risk factors, and its impact on QOL among women living in Yozgat Province, situated in the Central Anatolian region of Turkey, which has a larger rural population. The severity of UI and associated risks were analyzed based on the ICIQ-SF scores, while the assessment of QOL relied on the Wagner QOL Scale scores.
Frequency of UI in women
Among women aged 20 and older who sought care at the Training and Research Hospital Obstetrics and Gynecology outpatient clinic in Yozgat for reasons other than pregnancy follow-up, the prevalence of UI was 48% according to the ICIQ-SF and 62% according to the Wagner QOL Scale. Previous studies conducted in Turkey have reported UI frequency rates ranging from 21.3% to 86.7% among women (3,11). The frequency of UI reported worldwide in the last 5 years is 41.7% among women aged 20 and over in Singapore (6), 31.2% among women aged 20 and over in China (12), 45.1% among professional female athletes in Spain (13), 30.5% among women in Congo (14), 43% among Muslim women aged 18-75 in Israel (15), 63% among women aged 15-80 in Iran (16), and 41% among women over 65 years old in Uganda (17). Despite variations in geography, language, culture, customs, and traditions, UI remains a universal health concern for women. The literature suggests that differences in UI frequency among women are primarily attributed to distinct sociocultural, demographic, and economic factors associated with their respective regions.
Urinary incontinence risk factors in women
Urinary incontinence among women is a complex health issue influenced by multiple factors, as evidenced by studies conducted in the past decade. Demir et al identified risk factors for UI, including hypertension, diabetes mellitus, multiparity, higher BMI, and low education levels (18). Daneshpajooh et al found that age, higher BMI, pregnancy, diabetes, anxiety, and depression were associated with UI (5). Maroyi et al linked UI in postpartum women to a history of episiotomy and the delivery of large babies (14). Treister-Goltzman and Peleg reported a relationship between higher BMI and polygamy with severe and very severe UI (15). Yağmur and Gül highlighted the relationship between UI and factors such as age, education level, employment status, presence of chronic diseases, chronic constipation, history of difficult deliveries, and menopause (19). Luo et al, through multivariate logistic regression analysis, determined that older women with a history of vaginal delivery who were sexually active were more likely to experience UI (6).
Consistent with our results, previous studies have shown that UI is influenced by various factors, including age, polygamy, education level, employment status, obesity, number of births, episiotomy history, history of delivering large babies, menopause, anxiety, depression, constipation, history of difficult deliveries, vaginal delivery, sexual activity, and chronic diseases such as diabetes and hypertension. Our logistic regression analysis, which included BMI, miscarriage, education level, and age as variables, revealed that these factors accounted for 52.2% of the variance in UI frequency. Specifically, the analysis showed that a 1-unit increase in the miscarriage variable increased the likelihood of UI by 3.1 times, 1-unit increase in the primary school graduate variable increased the likelihood by 3.2 times, and 1-unit increase in the age variable increased the likelihood by 1.0 times. Therefore, it can be concluded that the probability of experiencing UI is higher among older women, those with primary school education, and those who have a history of miscarriages.
Our study highlights the significance of education once again. Educated women tend to play active roles in social and economic spheres, actively seeking early and efficient solutions to problems that might hinder their lifestyle. On the other hand, many uneducated women, particularly those living in rural areas, may avoid seeking treatment, regarding UI as a private matter and attributing it to the natural aging process. This tendency can lead to an increase in the severity of UI and a reduction in the overall QOL. Nearly half of the study participants were found to experience UI, possibly linked to the fact that 50% of them had only completed primary school education.
To the best of our knowledge, the finding that a 1-unit increase in the miscarriage variable increases the likelihood of UI by 3.1 times is a new finding in the literature. Existing research indicates that the frequency of UI is higher in women who have experienced miscarriages. However, it remains unclear whether UI serves as a predictor of the likelihood of miscarriage or if women who have experienced miscarriages face an increased risk of UI. Consequently, it is thought that comprehensive studies are necessary to elucidate the relationship between miscarriage and UI.
The effect of UI on women's QOL
Both measurement tools used in this research demonstrate that an increase in the severity of UI has a detrimental effect on the QOL. Yağmur and Gül found that UI moderately affected the QOL (19). Similarly, our study revealed that psychosocial impairment was moderate among women with UI. The moderate level of discomfort perceived by women with UI suggests that they may be relatively indifferent to this issue. This result might be influenced by the fact that 75% of the participants with UI in our study had either primary or secondary school education. It is conceivable that lower levels of education limit the search for solutions, and the belief that the problem is unsolvable strengthens the perception of destiny.
Numerous studies have consistently reported that higher BMI is associated with a higher frequency of UI and poor QOL (15,18,19). However, our study showed that the severity of UI in overweight women was less than that of obese and extremely obese women, and as a result, their QOL was affected less. This difference may be attributed to the fact that overweight women had lower intra-abdominal pressure than obese and extremely obese women, potentially resulting in a lower frequency of stress-type UI, which in turn could have a less significant impact on their QOL. Paradoxically, women with an ideal weight exhibited more severe UI and a lower QOL than obese women. This phenomenon could be explained by the negative impact of UI on body image among women with an ideal weight, potentially making them more vulnerable to the effects of UI on their overall well-being.
In light of our findings, it is evident that UI affects women across all age groups. However, the severity of the problem and its impact on QOL seem to be more pronounced in women aged 40-59. This observation is consistent with the majority of studies in the literature that emphasize the relationship between UI and age (3,6). While UI tends to peak in the age range of 40-49 years, it has been noted that the severity of UI decreases and QOL improves as age progresses, particularly in the age group of 60 and over. This shift may be attributed to the perception among women that UI is a natural consequence of aging, potentially reducing the psychological impact of UI on their overall QOL.
Limitations
This study has several limitations. First, it is a cross-sectional study conducted within a single health care facility involving a specific patient population, which could potentially limit the generalizability of the findings to broader populations. Second, as an outpatient clinic-based study, the characteristics of the study population may not fully represent the general population. The third limitation is that the presence of UI is based on subjective data collected using 2 scales, not objective methods. Lastly, the relatively small sample size may have limited the precision of some comparisons.
Conclusion
Miscarriage, aging, and low education levels are risk factors for UI. As the severity of UI increases, the QOL of affected individuals decreases. Early diagnosis is crucial, as the problem can be solved more quickly, and the QOL of women can be preserved. Health care professionals play a pivotal role in raising awareness among women about UI. Specifically, nurses and midwives can provide valuable discharge training for at-risk groups, and preventive health care providers can identify these groups early on to effectively address the problem. There is a pressing need for more effective policies to increase the education level of women. Moreover, practical solutions are required to enhance women's physical mobility. Collaborative efforts involving health authorities, local governments, and private enterprises can promote physical activity, potentially reducing a range of sedentary lifestyle-related issues, including UI, which, in turn, may contribute to cost savings in health care expenditures.
Acknowledgement
We would like to express our gratitude to Internal Medicine Specialist Dr Reşat Ferhan PAKİZ for his invaluable support and assistance throughout the research.
Funding sources
This study received no funding.
Ethical statement
The research received approval from the Yozgat Bozok University Ethics Committee (decision No. 34/17; decision date: 24.06.2022). The study adhered to the principles outlined in the Declaration of Helsinki. Participants were provided with a clear explanation of the study's purpose, and their informed verbal and written consent was obtained.
Conflicts of interest
The authors declare no conflicts of interest.
Author contributions
All listed authors meet the authorship criteria, and all authors are in agreement with the content of the manuscript.
Conceptualization: A.A. and D.E.
Research design: A.A. and D.E.
Data collection and processing: A.A. and D.E.
Analysis and interpretation: A.A.
Literature review: A.A. and D.E.
Original draft preparation: A.A.
Review and editing: A.A. and D.E.
Type of study: Original Article |
Subject:
Midwifery
References
1. Whiting D, Shane AI, Pope R, Payne S, Venn S. Female urinary incontinence in sub‐Saharan Africa. BJU Int. 2022;130(5):543-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Hagen S, Elders A, Stratton S, Sergenson N, Bugge C, Dean S. et al. Effectiveness of pelvic floor muscle training with and without electromyographic biofeedback for urinary incontinence in women: multicentre randomised controlled trial. BMJ. 2020;371. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Akkus Y, Pinar G. Evaluation of the prevalence, type, severity, and risk factors of urinary incontinence and its impact on quality of life among women in Turkey. Int Urogynecol J. 2016;27(6):887-93. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Şimşek Ş, Yağcı N. Investigation of urinary incontinence prevalance and pelvic floor dysfunction awareness in healthcare professionals. Journal of Adnan Menderes University Health Sciences Faculty. 2022;6(1):77-84. [View at Publisher] [DOI] [Google Scholar]
5. Daneshpajooh A, Naghibzadeh‐Tahami A, Najafipour H, Mirzaei M. Prevalence and risk factors of urinary incontinence among Iranian women. Neurourology and Urodynamics, 2021;40(2):642-52. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Luo R, Dai W, Tay LH, Ng FC, Koh LT. Urinary incontinence in female outpatients in Singapore. Int Urogynecol J. 2018;29(4):579-84. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Çetinel B, Özkan B, Can G, Oscan B. The validation study of ICIQ-SF Turkish version. Turk J Urol. 2004;30:332-8. [View at Publisher] [Google Scholar]
8. Wagner TH, Patrick DL, Bavendam TG, Martin ML, Buesching DP. Quality of life of persons with urinary incontinence: development of a new measure. Urology. 1996;47(1):67-71. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Karan A, Aksaç B, Ayyıldız H, Işıkoğlu M, Yalçın O, Eskiyurt N. Quality of life and its relation with objective assessment parameters in urinary incontinent patients. Turkish J Geriatr. 2000;3(3):102-6. [View at Publisher] [Google Scholar]
10. Yılmaz E, Muslu A, Özcan E. Quality of life at women with urinary inkontinence. ERÜ Sağlık Bilimleri Fakültesi Dergisi. 2014;2(2):1-14. [View at Publisher] [Google Scholar]
11. Durukan H, Tok E, Tok D, Aytan H. Self-Perceived frequency of urinary incontinence by women and distribution of incontinence types according to age-groups in target population of Mersin. Medical Bulletin of Zeynep Kamil. 2015;46(1):1-5. [View at Publisher] [DOI] [Google Scholar]
12. Xie X, Chen Y, Khan A, Long T, Li S, Xie M. Risk factors for urinary incontinence in Chinese women: a cross-sectional survey. Female Pelvic Med Reconstr Surg. 2021;27(6):377-81. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Rodríguez-López ES, Calvo-Moreno SO, Basas-García Á, Gut- ierrez-Ortega F, Guodemar-Pérez J, Acevedo-Gómez MB. Prevalence of urinary incontinence among elite athletes of both sexes. J Sci Med Sport. 2021;24(4):338-44. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Maroyi R, Mwambali N, Moureau MK, Keyser LE, McKinney JL, Brown HW, et al. Prevalence of urinary incontinence in pregnant and postpartum women in the Democratic Republic of Congo. Int Urogynecol J. 2021;32(7):1883-8. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Treister-Goltzman Y, Peleg R. Urinary incontinence among Muslim women in Israel: risk factors and help-seeking behavior. Int Urogynecol J. 2018;29(4):539-46. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Daneshpajooh A, Naghibzadeh‐Tahami A, Najafipour H, Mirzaei M. Prevalence and risk factors of urinary incontinence among Iranian women. Neurourol Urodyn. 2021;40(2):642-52. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Mutungi T, Spitzer R, Origa M, Kayondo M, Kyakuhaire M, Nyiramugisha J. Prevalence of urogynaecology symptoms in a rural population in western-Uganda. J Obstet Gynaecol Can. 2019;41(5):727. [View at Publisher] [DOI] [Google Scholar]
18. Demir Ö, Sen V, Irer B, Bozkurt O, Esen A. Prevalence and possible risk factors for urinary incontinence: A cohort study in the city of Izmir. Urol Int. 2017;99(1):84-90. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Yağmur Y, Gül S. Urinary incontinence in women aged 40 and older: Its prevalence, risk factors, and effect on quality of life. Niger J Clin Pract. 2021;24(2):186-92. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






