Volume 20, Issue 1 (4-2023)
J Res Dev Nurs Midw 2023, 20(1): 20-23 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Yahyaei S, Khoddam H, Alinaghimaddah S, Modanloo M. Prevalence of alarm fatigue and its relevant factors in critical care nurses: A cross-sectional study. J Res Dev Nurs Midw 2023; 20 (1) :20-23
URL: http://nmj.goums.ac.ir/article-1-1437-en.html
URL: http://nmj.goums.ac.ir/article-1-1437-en.html
1- Critical Care Nursing, Golestan University of Medical Sciences, Gorgan, Iran
2- Golestan University of Medical Sciences
3- Department of Anesthesiology and Critical Care, School of Medicine, Golestan University of Medical Sciences, Gorgan, Iran
4- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,modanloo.mahnaz@gmail.com
2- Golestan University of Medical Sciences
3- Department of Anesthesiology and Critical Care, School of Medicine, Golestan University of Medical Sciences, Gorgan, Iran
4- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran ,
Full-Text [PDF 407 kb]
(3236 Downloads)
| Abstract (HTML) (4953 Views)
Full-Text: (1193 Views)
Introduction
On the one hand, the increasing number of patients in critical care units requires the use of advanced equipment such as ventilators, patient monitoring systems, and infusion pumps, and, on the other hand, the presence of a skilled care team with clinical knowledge and experience in working with such equipment (1, 2).
This equipment has audio and visual alarm systems that alert users to disturbances in patients’ physiological status, medical equipment and systems malfunctioning, or risks that threaten the patients (3, 4). According to reports from an American hospital, there are one million alarms per week and an average of 350 alarms per day for each patient admitted to critical care units (5, 6). While it is crucial to utilize a reliable, accurate, user-friendly, and cost-effective clinical warning system to provide efficient and high-quality care in critical care units (7), studies have found that 72-99% of alarms are false or clinically insignificant (3, 5, 8, 9). The phenomenon known as “Cry Wolf” is the most significant and common problem associated with false alarms, leading to distrust, inadequate response, and long-term neglect of alarms by nurses (10). The willingness of healthcare providers to respond to an alarm is directly proportional to their trust in the alarm system. In other words, if alarms are valid in 90% of cases, they respond to them about 90% of the time; however, if alarms are only valid in 10% of cases, their response rate drops to approximately 10% (4).
Increased exposure to false clinical alarms results in a complex and uncontrollable cognitive phenomenon known as alarm fatigue, which causes changes in human attention and cognition to adapt to the surrounding environment (11). Alarm fatigue occurs when healthcare providers, especially nurses, are exposed to numerous alarms of varying importance, leading to gradual desensitization and actions such as turning off the alarm system, delaying a response, or not responding (4, 8).
Alarm fatigue has become a growing epidemic, with false alarms estimated to have a prevalence of 72-99% (3, 4, 8), posing a significant risk to patient safety and life (12). The American Emergency Care Research Institute identifies alarm fatigue as one of the top 10 technology-based risks to patient safety (13). In the United States alone, hundreds of patients die yearly due to a lack of response or delayed response to alarms (4). Moreover, this phenomenon can lead to problems such as professional incompetence, job dissatisfaction, stress, irritability, tension headaches among nurses, jeopardizing patient safety and life, increased medical errors, and compromised quality of care and services for critically ill patients (4, 14, 15).
Reports indicate that improper adjustment of alarm parameters, lack of proportionality between alarm settings and clinical status and patient needs, the incorrect connection of electronic device probes to patients, personnel’s inability to identify the cause of alarms, inadequate training of nurses on monitoring and alarm systems, and malfunctioning alarm equipment are among the most common causes of alarm fatigue (5). Considering that addressing nurses’ alarm fatigue directly affects the quality of critical care and that its causes are preventable in many cases, the present study aims to determine the prevalence of alarm fatigue among nurses and its underlying factors in critical care units of hospitals in Golestan province.
Methods
The present cross-sectional study examined nurses working in all critical care units (ICUs, CCUs) of medical centers in Golestan province, northeast Iran in 2019. To this end, 308 eligible nurses were included in the study using the census method. The inclusion criteria were as follows: working in critical care units during the research, at least six months of work experience, no hearing problems, no history of crises, death of relatives, or divorce in the last six months.
The data collection tool included the nurses’ demographic and occupational information registration forms and the nurses’ alarm fatigue questionnaire. The demographic information registration form consisted of age, gender, marital status, place of residence, education level, and monthly income. The occupational information registration form also comprised the job status, clinical work experience, work experience in critical care units, type of shift work, type and rate of overtime, and type of unit. The 13-item nurses’ alarm fatigue questionnaire was designed by Torabzadeh et al. (16).
The answers to this questionnaire were on a 5-point Likert scale (never, rarely, sometimes, often, and always with 0 to 4 points). The total number of points was 0-52 (a score of 0-7: no alarm fatigue, 8-20: low alarm fatigue, 21-32: moderate alarm fatigue, and 33-52: severe alarm fatigue). In order to collect data, permission was obtained to enter the research environment after the project was approved, the ethics committee granted permission, a letter of recommendation from the research deputy was obtained, and it was presented to the officials. Eligible nurses were included in the study. Furthermore, the researcher attended the research environment in three shifts (morning, afternoon, and evening) and provided necessary explanations to the nurses regarding the research objectives, voluntary participation in the study, information confidentiality, and questionnaire completion. The researcher obtained informed consent from the nurses to complete the questionnaires.
The researcher randomly entered the research environment for one hour in the morning, afternoon, or night shifts to record the source, number, and type of alarms when they were heard. The valid or false alarms were identified and recorded. After data collection, the frequency distribution, central and dispersion indices were utilized to describe the results. Chi-square and Fisher’s tests also analyzed the relationship between alarm fatigue levels and underlying factors. After confirming the normal distribution of alarm fatigue scores using the Kolmogorov-Smirnov test (P=0.67), the multiple linear regression test was utilized after examining and confirming the assumptions to analyze the relationship between the nurses’ alarm fatigue scores (dependent variable) and underlying factors, including the nurses’ demographic and professional characteristics (independent variable).
Demographic and clinical characteristics included age, gender, marital status, education level, place of residence, income level, job status, clinical work experience, work experience in critical care units, type of shift work, type of overtime, rate of overtime, and work unit. Data were analyzed using SPSS16 with a significance level 0.05 and a 95% confidence interval. The necessary sample size was estimated to ensure the adequacy of the study power to detect a statistically significant relationship between alarm fatigue and its relevant factors. Given the prevalence of 72-99% of alarm fatigue (3, 4, 8), the prevalence of 80% was used as the basis for determining the sample size in this study. The sample size was estimated to be 120 using the following formula, considering the Type I error of 5%, the precision of 8% (10% of the prevalence rate), and the probability of a 20% attrition.
Results
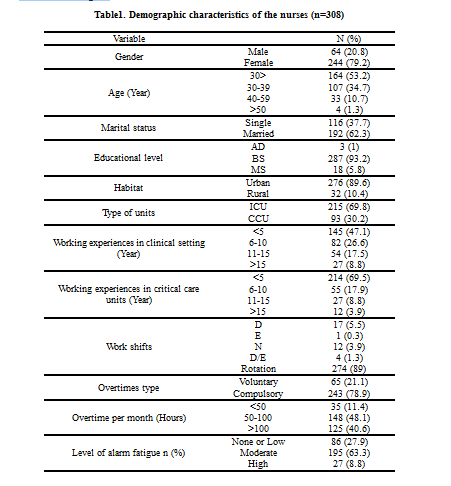
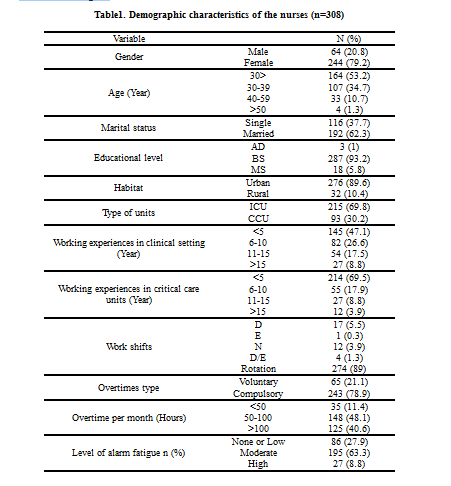
The mean age of the nurses was 30.7±6.54 years, and the majority (53.2%) were under 30 years old. Additionally, most of the nurses were female (79.2%), married (62.3%), residing in urban areas (89.6%), and held a bachelor’s degree in nursing (93.2%). Moreover, more than half of them (52.9%) had over five years of clinical work experience, and 30.5% had worked in critical care units for over five years. According to studies, most nurses (89%) worked rotational shifts and had mandatory overtime (78.9%). Furthermore, the average (standard deviation) of their overtime hours was 92.97 hours (32.54), with a significant portion (48.1%) working between 50-100 hours per month (Table 1).
Based on the findings, the mean score (standard deviation) for nurses’ alarm fatigue was 24.1 (6.52). Only a tiny percentage (1.9%, n=6) did not report any alarm fatigue. Of the remaining nurses, 26% experienced mild fatigue (n=132), 63.3% had moderate fatigue (n=161), and 8.8% exhibited severe fatigue (n=9). Those with moderate alarm fatigue were predominantly women (87.5%), working as compulsory medical service workers (35.9%) and holding a bachelor’s degree in nursing (93.3%). Additionally, 87.2% were rotational shift workers, 47.7% had less than five years of work experience in hospitals, with 71.8% had less than five years of experience in critical care units. Most (81.5%) were required to work mandatory overtime for 50-100 hours per month (45.1%).
The sources of alarms in critical care units included cardiac monitoring devices, pulse oximeters, mechanical ventilators, infusion pumps, and air mattress pumps. Most false alarms were due to the disconnection of the pulse oximeter probe from the patient (59.45%). During the 60-hour observation period in critical care units, 7782 alarms were detected, of which 1902 (24.44%) were valid, and 5880 (75.55%) were false. The breakdown of alarms based on units showed 4841 false alarms and 1704 sound alarms in the ICU, and 1039 false alarms and 198 valid alarms in the CCU.
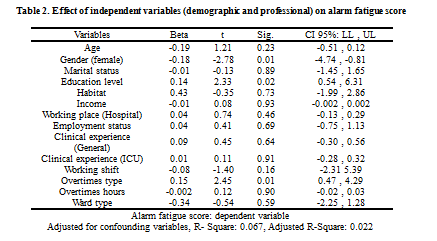
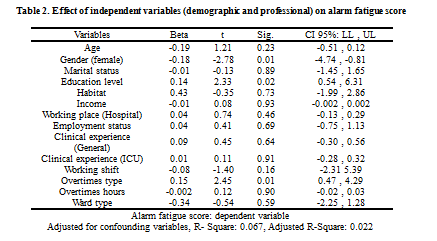
The multiple linear regression analysis examined the effects of various independent variables (including age, gender, marital status, education level, place of residence, income level, job status, clinical work experience, work experience in critical units, type of shift work, type and rate of overtime, and work unit) on the dependent variable, which was the alarm fatigue score. Firstly, the model indicated that the independent variables included had a significant effect (P=0.04) on the alarm fatigue score, with an adjusted R Square of 0.03. Secondly, among all the variables in the model, only gender (P=0.01), education level (P=0.02), and type of overtime (P=0.01) had statistically significant effects on the alarm fatigue score (Table 2). Furthermore, women had lower alarm fatigue scores and experienced less fatigue than men, while mandatory overtime was associated with a higher rate of alarm fatigue.
Discussion
According to the present study’s results, 63.3% of nurses have moderate alarm fatigue, and their gender, type of overtime, and education levels showed significant relationships with alarm fatigue scores (alarm fatigue intensity). These findings align with a study by Cho et al. (2016), who reported an average staff alarm fatigue score (of 24.3±4) out of 35, resulting from clinical alarms. Also, false alarms hindered proper decision-making in medical care (15). The present study differed from Cho’s study in two aspects. Firstly, the present study included a wider statistical population of nurses from critical care units across the entire province, which allowed for varying fatigue levels among nurses working in different communities. Secondly, the present study did not differentiate between shift work types for checking alarms. Although the type of shift work did not show a significant relationship with the level of alarm fatigue in this research, it was still examined.
A statistically significant relationship between nurses’ gender and alarm fatigue was observed in the present study. Men’s and women’s mental and intellectual behaviors inherently differ in certain aspects, and these differences, influenced by gender, can affect nurses’ alarm fatigue. Furthermore, the type of mandatory overtime for nurses showed a statistically significant relationship with alarm fatigue (P<0.05). Roger et al. (2004) reported that excessive overtime, particularly with 12-hour shifts, should be eliminated, and a culture should be established to recognize nurse fatigue as a risk (17). In a study by Funk (2014), approximately 80% of nurses with 11 years of clinical work experience reported disruptions in patient care due to alarm fatigue caused by many false alarms (18). However, in the present study, 51.9% of nurses with less than five years of clinical work experience in critical care units completed the questionnaires and exhibited moderate alarm fatigue. It is important to note that the present study evaluated only nurses working in critical care units (ICU, CCU), while the study mentioned above also included general nurses. Even though most of the research population was 30 years old, they still experienced alarm fatigue. Hensley (2016) reported a 78% impact on nurses’ alarm fatigue (19), which is consistent with the findings of this study, where nurses exhibited moderate alarm fatigue. Deb’s study (2014) indicated that both demographic characteristics and the type of shift work for nurses showed statistically significant relationships with alarm fatigue (P<0.05), and nurses experienced higher workloads and mental pressure during the day shift compared to the night shift. The type of shift work in Deb’s study was defined as 12 hours (20). The present research results align with Deb’s study in terms of gender being the only demographic characteristic of nurses that showed a statistically significant relationship with alarm fatigue. In contrast, no significant relationship was observed with the type of shift, as the shift work was defined as 12 hours. The present study examined the relationships between alarm fatigue and the three shifts (morning, afternoon, and evening), along with the number of alarms in all three shifts.
Drew’s study (2014) also indicated the effect of an increase in false alarms on nurses’ alarm fatigue in the ICUs (21). The reason for selecting this unit by the author might be because the patients were routinely under continuous cardiac monitoring, and it was considered a part of the patient’s regular care. However, higher false alarms caused by the cardiac monitoring device were also standard. The result was inconsistent with the present study regarding the source of false alarms. The ICU and CCU were investigated in the present study because both were under continuous cardiac monitoring due to patients’ specific clinical status. However, false alarms caused by the disconnection of the pulse oximeter probe were also more common, and much attention was paid to the connections of chest leads for cardiac monitoring in both units. Cho’s study reported that the highest false alarms were related to the disconnection of chest leads of cardiac monitoring devices (15). Harris (2014) also reported the prevalence of false alarms due to cardiac monitoring devices. Such differences between the present study and the research mentioned above were probably owing to determinant factors in patients, such as age, cardiovascular diseases, respiratory problems, and mechanical ventilation (22). Sowan (2016) also considered the cardiac monitoring device and pulse oximeter effective in the prevalence of false alarms (23). Another Atzema (2006) study reported an increase in false alarms due to cardiac monitoring devices (24). This result was inconsistent with the present study as the research population only comprised cardiac patients. In Konkani’s study (2012), 78% of nurses reported that false alarms caused their distrust in sound alarms and led to an alternative reaction, such as deactivating them (25). The result was consistent with the present study due to the increased number of false alarms. Even though alarms are built to improve patient safety, a higher prevalence of false alarms and alarm fatigue may put patients at greater risk for injury (26).
A research limitation was the impossibility of examining the cause of false alarms. As there was no protocol to set alarms of devices according to the patient’s status to examine false alarms, and some critical care units or some shifts received the least number of alarms, there was a possibility that the nurses turned off the alarms, or medical devices and equipment were adjusted in a broader range to activate the alarm, which was not under the researcher’s control.
Conclusion
Based on the research results, most nurses suffer from moderate alarm fatigue; hence, it is suggested to adopt appropriate strategies to maintain patients’ health and safety. Improper adjustment of parameter ranges in devices with alarm systems and excessive use of monitoring systems without the real need of patients are important factors contributing to alarm fatigue. Teaching nurses about the proper use of alarm devices, employing suitable approaches for patient monitoring, and reducing the number of false alarms in the equipment may help alleviate the severity of alarm fatigue.
Acknowledgement
The present article is the result of the thesis for achieving master degree in critical care nursing. The authors would like to appreciate Research and Technology deputy of the Golestan University of Medical Sciences for their scientific and financial support of the project and all participated nurses in this research.
Funding source
This study was supported financially by the Golestan University of Medical Sciences.
Ethical statement
The study received approval from the Ethics Committee of Goletsan University of Medical Sciences (ethical approval code: IR.GOUMS.REC.1397.299), and participants were asked to read and sign the written consent before filling the questionnaire.
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this study.
Author contributions
All authors have active contribution in designing and conducting the study and also in preparing draft and final version of the manuscript for publication.
On the one hand, the increasing number of patients in critical care units requires the use of advanced equipment such as ventilators, patient monitoring systems, and infusion pumps, and, on the other hand, the presence of a skilled care team with clinical knowledge and experience in working with such equipment (1, 2).
This equipment has audio and visual alarm systems that alert users to disturbances in patients’ physiological status, medical equipment and systems malfunctioning, or risks that threaten the patients (3, 4). According to reports from an American hospital, there are one million alarms per week and an average of 350 alarms per day for each patient admitted to critical care units (5, 6). While it is crucial to utilize a reliable, accurate, user-friendly, and cost-effective clinical warning system to provide efficient and high-quality care in critical care units (7), studies have found that 72-99% of alarms are false or clinically insignificant (3, 5, 8, 9). The phenomenon known as “Cry Wolf” is the most significant and common problem associated with false alarms, leading to distrust, inadequate response, and long-term neglect of alarms by nurses (10). The willingness of healthcare providers to respond to an alarm is directly proportional to their trust in the alarm system. In other words, if alarms are valid in 90% of cases, they respond to them about 90% of the time; however, if alarms are only valid in 10% of cases, their response rate drops to approximately 10% (4).
Increased exposure to false clinical alarms results in a complex and uncontrollable cognitive phenomenon known as alarm fatigue, which causes changes in human attention and cognition to adapt to the surrounding environment (11). Alarm fatigue occurs when healthcare providers, especially nurses, are exposed to numerous alarms of varying importance, leading to gradual desensitization and actions such as turning off the alarm system, delaying a response, or not responding (4, 8).
Alarm fatigue has become a growing epidemic, with false alarms estimated to have a prevalence of 72-99% (3, 4, 8), posing a significant risk to patient safety and life (12). The American Emergency Care Research Institute identifies alarm fatigue as one of the top 10 technology-based risks to patient safety (13). In the United States alone, hundreds of patients die yearly due to a lack of response or delayed response to alarms (4). Moreover, this phenomenon can lead to problems such as professional incompetence, job dissatisfaction, stress, irritability, tension headaches among nurses, jeopardizing patient safety and life, increased medical errors, and compromised quality of care and services for critically ill patients (4, 14, 15).
Reports indicate that improper adjustment of alarm parameters, lack of proportionality between alarm settings and clinical status and patient needs, the incorrect connection of electronic device probes to patients, personnel’s inability to identify the cause of alarms, inadequate training of nurses on monitoring and alarm systems, and malfunctioning alarm equipment are among the most common causes of alarm fatigue (5). Considering that addressing nurses’ alarm fatigue directly affects the quality of critical care and that its causes are preventable in many cases, the present study aims to determine the prevalence of alarm fatigue among nurses and its underlying factors in critical care units of hospitals in Golestan province.
Methods
The present cross-sectional study examined nurses working in all critical care units (ICUs, CCUs) of medical centers in Golestan province, northeast Iran in 2019. To this end, 308 eligible nurses were included in the study using the census method. The inclusion criteria were as follows: working in critical care units during the research, at least six months of work experience, no hearing problems, no history of crises, death of relatives, or divorce in the last six months.
The data collection tool included the nurses’ demographic and occupational information registration forms and the nurses’ alarm fatigue questionnaire. The demographic information registration form consisted of age, gender, marital status, place of residence, education level, and monthly income. The occupational information registration form also comprised the job status, clinical work experience, work experience in critical care units, type of shift work, type and rate of overtime, and type of unit. The 13-item nurses’ alarm fatigue questionnaire was designed by Torabzadeh et al. (16).
The answers to this questionnaire were on a 5-point Likert scale (never, rarely, sometimes, often, and always with 0 to 4 points). The total number of points was 0-52 (a score of 0-7: no alarm fatigue, 8-20: low alarm fatigue, 21-32: moderate alarm fatigue, and 33-52: severe alarm fatigue). In order to collect data, permission was obtained to enter the research environment after the project was approved, the ethics committee granted permission, a letter of recommendation from the research deputy was obtained, and it was presented to the officials. Eligible nurses were included in the study. Furthermore, the researcher attended the research environment in three shifts (morning, afternoon, and evening) and provided necessary explanations to the nurses regarding the research objectives, voluntary participation in the study, information confidentiality, and questionnaire completion. The researcher obtained informed consent from the nurses to complete the questionnaires.
The researcher randomly entered the research environment for one hour in the morning, afternoon, or night shifts to record the source, number, and type of alarms when they were heard. The valid or false alarms were identified and recorded. After data collection, the frequency distribution, central and dispersion indices were utilized to describe the results. Chi-square and Fisher’s tests also analyzed the relationship between alarm fatigue levels and underlying factors. After confirming the normal distribution of alarm fatigue scores using the Kolmogorov-Smirnov test (P=0.67), the multiple linear regression test was utilized after examining and confirming the assumptions to analyze the relationship between the nurses’ alarm fatigue scores (dependent variable) and underlying factors, including the nurses’ demographic and professional characteristics (independent variable).
Demographic and clinical characteristics included age, gender, marital status, education level, place of residence, income level, job status, clinical work experience, work experience in critical care units, type of shift work, type of overtime, rate of overtime, and work unit. Data were analyzed using SPSS16 with a significance level 0.05 and a 95% confidence interval. The necessary sample size was estimated to ensure the adequacy of the study power to detect a statistically significant relationship between alarm fatigue and its relevant factors. Given the prevalence of 72-99% of alarm fatigue (3, 4, 8), the prevalence of 80% was used as the basis for determining the sample size in this study. The sample size was estimated to be 120 using the following formula, considering the Type I error of 5%, the precision of 8% (10% of the prevalence rate), and the probability of a 20% attrition.
Results
The mean age of the nurses was 30.7±6.54 years, and the majority (53.2%) were under 30 years old. Additionally, most of the nurses were female (79.2%), married (62.3%), residing in urban areas (89.6%), and held a bachelor’s degree in nursing (93.2%). Moreover, more than half of them (52.9%) had over five years of clinical work experience, and 30.5% had worked in critical care units for over five years. According to studies, most nurses (89%) worked rotational shifts and had mandatory overtime (78.9%). Furthermore, the average (standard deviation) of their overtime hours was 92.97 hours (32.54), with a significant portion (48.1%) working between 50-100 hours per month (Table 1).
Based on the findings, the mean score (standard deviation) for nurses’ alarm fatigue was 24.1 (6.52). Only a tiny percentage (1.9%, n=6) did not report any alarm fatigue. Of the remaining nurses, 26% experienced mild fatigue (n=132), 63.3% had moderate fatigue (n=161), and 8.8% exhibited severe fatigue (n=9). Those with moderate alarm fatigue were predominantly women (87.5%), working as compulsory medical service workers (35.9%) and holding a bachelor’s degree in nursing (93.3%). Additionally, 87.2% were rotational shift workers, 47.7% had less than five years of work experience in hospitals, with 71.8% had less than five years of experience in critical care units. Most (81.5%) were required to work mandatory overtime for 50-100 hours per month (45.1%).
The sources of alarms in critical care units included cardiac monitoring devices, pulse oximeters, mechanical ventilators, infusion pumps, and air mattress pumps. Most false alarms were due to the disconnection of the pulse oximeter probe from the patient (59.45%). During the 60-hour observation period in critical care units, 7782 alarms were detected, of which 1902 (24.44%) were valid, and 5880 (75.55%) were false. The breakdown of alarms based on units showed 4841 false alarms and 1704 sound alarms in the ICU, and 1039 false alarms and 198 valid alarms in the CCU.
The multiple linear regression analysis examined the effects of various independent variables (including age, gender, marital status, education level, place of residence, income level, job status, clinical work experience, work experience in critical units, type of shift work, type and rate of overtime, and work unit) on the dependent variable, which was the alarm fatigue score. Firstly, the model indicated that the independent variables included had a significant effect (P=0.04) on the alarm fatigue score, with an adjusted R Square of 0.03. Secondly, among all the variables in the model, only gender (P=0.01), education level (P=0.02), and type of overtime (P=0.01) had statistically significant effects on the alarm fatigue score (Table 2). Furthermore, women had lower alarm fatigue scores and experienced less fatigue than men, while mandatory overtime was associated with a higher rate of alarm fatigue.
Discussion
According to the present study’s results, 63.3% of nurses have moderate alarm fatigue, and their gender, type of overtime, and education levels showed significant relationships with alarm fatigue scores (alarm fatigue intensity). These findings align with a study by Cho et al. (2016), who reported an average staff alarm fatigue score (of 24.3±4) out of 35, resulting from clinical alarms. Also, false alarms hindered proper decision-making in medical care (15). The present study differed from Cho’s study in two aspects. Firstly, the present study included a wider statistical population of nurses from critical care units across the entire province, which allowed for varying fatigue levels among nurses working in different communities. Secondly, the present study did not differentiate between shift work types for checking alarms. Although the type of shift work did not show a significant relationship with the level of alarm fatigue in this research, it was still examined.
A statistically significant relationship between nurses’ gender and alarm fatigue was observed in the present study. Men’s and women’s mental and intellectual behaviors inherently differ in certain aspects, and these differences, influenced by gender, can affect nurses’ alarm fatigue. Furthermore, the type of mandatory overtime for nurses showed a statistically significant relationship with alarm fatigue (P<0.05). Roger et al. (2004) reported that excessive overtime, particularly with 12-hour shifts, should be eliminated, and a culture should be established to recognize nurse fatigue as a risk (17). In a study by Funk (2014), approximately 80% of nurses with 11 years of clinical work experience reported disruptions in patient care due to alarm fatigue caused by many false alarms (18). However, in the present study, 51.9% of nurses with less than five years of clinical work experience in critical care units completed the questionnaires and exhibited moderate alarm fatigue. It is important to note that the present study evaluated only nurses working in critical care units (ICU, CCU), while the study mentioned above also included general nurses. Even though most of the research population was 30 years old, they still experienced alarm fatigue. Hensley (2016) reported a 78% impact on nurses’ alarm fatigue (19), which is consistent with the findings of this study, where nurses exhibited moderate alarm fatigue. Deb’s study (2014) indicated that both demographic characteristics and the type of shift work for nurses showed statistically significant relationships with alarm fatigue (P<0.05), and nurses experienced higher workloads and mental pressure during the day shift compared to the night shift. The type of shift work in Deb’s study was defined as 12 hours (20). The present research results align with Deb’s study in terms of gender being the only demographic characteristic of nurses that showed a statistically significant relationship with alarm fatigue. In contrast, no significant relationship was observed with the type of shift, as the shift work was defined as 12 hours. The present study examined the relationships between alarm fatigue and the three shifts (morning, afternoon, and evening), along with the number of alarms in all three shifts.
Drew’s study (2014) also indicated the effect of an increase in false alarms on nurses’ alarm fatigue in the ICUs (21). The reason for selecting this unit by the author might be because the patients were routinely under continuous cardiac monitoring, and it was considered a part of the patient’s regular care. However, higher false alarms caused by the cardiac monitoring device were also standard. The result was inconsistent with the present study regarding the source of false alarms. The ICU and CCU were investigated in the present study because both were under continuous cardiac monitoring due to patients’ specific clinical status. However, false alarms caused by the disconnection of the pulse oximeter probe were also more common, and much attention was paid to the connections of chest leads for cardiac monitoring in both units. Cho’s study reported that the highest false alarms were related to the disconnection of chest leads of cardiac monitoring devices (15). Harris (2014) also reported the prevalence of false alarms due to cardiac monitoring devices. Such differences between the present study and the research mentioned above were probably owing to determinant factors in patients, such as age, cardiovascular diseases, respiratory problems, and mechanical ventilation (22). Sowan (2016) also considered the cardiac monitoring device and pulse oximeter effective in the prevalence of false alarms (23). Another Atzema (2006) study reported an increase in false alarms due to cardiac monitoring devices (24). This result was inconsistent with the present study as the research population only comprised cardiac patients. In Konkani’s study (2012), 78% of nurses reported that false alarms caused their distrust in sound alarms and led to an alternative reaction, such as deactivating them (25). The result was consistent with the present study due to the increased number of false alarms. Even though alarms are built to improve patient safety, a higher prevalence of false alarms and alarm fatigue may put patients at greater risk for injury (26).
A research limitation was the impossibility of examining the cause of false alarms. As there was no protocol to set alarms of devices according to the patient’s status to examine false alarms, and some critical care units or some shifts received the least number of alarms, there was a possibility that the nurses turned off the alarms, or medical devices and equipment were adjusted in a broader range to activate the alarm, which was not under the researcher’s control.
Conclusion
Based on the research results, most nurses suffer from moderate alarm fatigue; hence, it is suggested to adopt appropriate strategies to maintain patients’ health and safety. Improper adjustment of parameter ranges in devices with alarm systems and excessive use of monitoring systems without the real need of patients are important factors contributing to alarm fatigue. Teaching nurses about the proper use of alarm devices, employing suitable approaches for patient monitoring, and reducing the number of false alarms in the equipment may help alleviate the severity of alarm fatigue.
Acknowledgement
The present article is the result of the thesis for achieving master degree in critical care nursing. The authors would like to appreciate Research and Technology deputy of the Golestan University of Medical Sciences for their scientific and financial support of the project and all participated nurses in this research.
Funding source
This study was supported financially by the Golestan University of Medical Sciences.
Ethical statement
The study received approval from the Ethics Committee of Goletsan University of Medical Sciences (ethical approval code: IR.GOUMS.REC.1397.299), and participants were asked to read and sign the written consent before filling the questionnaire.
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this study.
Author contributions
All authors have active contribution in designing and conducting the study and also in preparing draft and final version of the manuscript for publication.
Type of study: Original Article |
Subject:
Nursing
References
1. Ruppel H, Funk M, Whittemore R, Wung S-F, Bonafide CP, Kennedy HP, et al. Critical care nurses' clinical reasoning about physiologic monitor alarm customisation: An interpretive descriptive study. J Clin Nurs. 2019;28(15-16):3033-41. [View at paplisher] [DOI] [PMID] [Google Scholar]
2. Movahedi A, Sadooghiasl A, Ahmadi F, Vaismoradi M. Smart care for dealing with nurses' alarm fatigue in the intensive care unit. Journal of nursing scholarship : an official publication of Sigma Theta Tau International Honor Society of Nursing. 2023; Online ahead of print. [View at paplisher] [DOI] [PMID] [Google Scholar]
3. Lewandowska K, Weisbrot M, Cieloszyk A, Mędrzycka-Dąbrowska W, Krupa S, Ozga D. Impact of Alarm Fatigue on the Work of Nurses in an Intensive Care Environment-A Systematic Review. International journal of environmental research and public health. 2020;22(17). [View at paplisher] [DOI] [PMID] [Google Scholar]
4. Bach TA, Berglund LM, Turk E. Managing alarm systems for quality and safety in the hospital setting. BMJ open quality. 2018;7(3):e000202. [DOI] [PMID] [Google Scholar]
5. Gaines K. Alarm fatigue is way too real (and scary) for nurses [Internet]. 2022. [View at paplisher]
6. Gaines K. Joint Commission Tackles Nurse Burnout in New Report [Internet]. 2019. [View at paplisher]
7. Zhao Y, Wan M, Liu H, Ma M. The current situation and influencing factors of the alarm fatigue of nurses' medical equipment in the intensive care unit based on intelligent medical care. Journal of Healthcare Engineering. 2021;2021. [View at paplisher] [DOI] [PMID] [Google Scholar]
8. Carelli L, Terzoni S, Destrebecq A, Formenti P, Soumahoro F, Esposito A, et al. Alarm fatigue in nurses working in intensive care units: A multicenter study Work. 2022;72:651-6. [View at paplisher] [DOI] [PMID] [Google Scholar]
9. Dee SA, Tucciarone J, Plotkin G, Mallilo C. Determining the impact of an alarm management program on alarm fatigue among ICU and Telemetry RNs: An evidence based research project. SAGE Open Nursing. 2022;8:23779608221098713. [View at paplisher] [DOI] [PMID] [Google Scholar]
10. Mastrogirolamo M, Gatta L, Bove D. Il" Cry-Wolf Effect". Gli infermieri ed i falsi allarmi in Terapia Intensiva. Scenario. 2022;39(2):35-40. [View at paplisher] [DOI] [Google Scholar]
11. Zhao Y, Wan M, Liu H, Ma M. The Current Situation and Influencing Factors of the Alarm Fatigue of Nurses' Medical Equipment in the Intensive Care Unit Based on Intelligent Medical Care. Journal of Healthcare Engineering. 2021;2021:9994303. [View at paplisher] [DOI] [PMID] [Google Scholar]
12. Wunderlich MM, Amende-Wolf S, Krampe H, Kruppa J, Spies C, Weiß B, et al. A Brief Questionnaire for Measuring Alarm Fatigue in Nurses and Physicians in Intensive Care Units. Research Square; 2023. [DOI] [Google Scholar]
13. Emergency Care Research Institute(ECRI). Special Report: Top 10 Patient Safety Concerns 2023. ECRI and the Institute for Safe Medication Practices (ISMP); 2023. [View at paplisher]
14. Shanmugham M, Strawderman L, Babski-Reeves K, Bian L. Alarm-Related Workload in Default and Modified Alarm Settings and the Relationship Between Alarm Workload, Alarm Response Rate, and Care Provider Experience: Quantification and Comparison Study JMIR human factors. 2018;5(4):e11704. [View at paplisher] [DOI] [PMID] [Google Scholar]
15. Cho OM, Kim H, Lee YW, Cho I. Clinical Alarms in Intensive Care Units: Perceived Obstacles of Alarm Management and Alarm Fatigue in Nurses. Healthc Inform Res. 2016;22(1):46-53. [View at paplisher] [DOI] [PMID] [Google Scholar]
16. Torabizadeh C, Yousefinya A, Zand F, Rakhshan M, Fararooei M. A nurses' alarm fatigue questionnaire: development and psychometric properties. J Clin Monit Comput. 2017;31(6):1305-12. [View at paplisher] [DOI] [PMID] [Google Scholar]
17. Rogers AE, Hwang W-T, Scott LD AL, Dinges DF. The working hours of hospital staff nurses and patient safety. Health affairs. 2004;23(4):202-12. [View at paplisher] [DOI] [PMID] [Google Scholar]
18. Funk M, Clark JT, Bauld TJ, Ott JC, Coss P. Attitudes and practices related to clinical alarms. Am J Crit Care. 2014;23(3):e9-18. [View at paplisher] [DOI] [PMID] [Google Scholar]
19. Hensley P. Reducing the Harm Associated with Clinical Alarm Systems: Meeting the Joint Commission National Patient Safety Goal. 06.01. 01 Performance Elements. 2016. [View at paplisher] [Google Scholar]
20. Deb S. Definition of alarm fatigue and its influence on staff performance. Bozeman, Montana: Montana State University-Bozeman, College of Engineering; 2014. [View at paplisher] [Google Scholar]
21. Drew BJ, Harris P, Zegre-Hemsey JK, Mammone T, Schindler D, Salas-Boni R, et al. Insights into the problem of alarm fatigue with physiologic monitor devices: a comprehensive observational study of consecutive intensive care unit patients. PLoS One. 2014;9(10):e110274. [View at paplisher] [DOI] [PMID] [Google Scholar]
22. Harris PR, Zègre-Hemsey JK, Mammone T, Schindler D, Hu X, Bai Y. Patient Characteristics Associated with False Arrhythmia Alarms in Intensive Care. Therapeutics and Clinical Risk Management. 2014; 13: 499-513. [View at paplisher] [DOI] [PMID] [Google Scholar]
23. Sowan AK, Gomez TM, Tarriela AF, Reed CC, Paper BM. Changes in Default Alarm Settings and Standard In-Service are Insufficient to Improve Alarm Fatigue in an Intensive Care Unit: A Pilot Project. JMIR Hum Factors. 2016;3(1):e1. [View at paplisher] [DOI] [PMID] [Google Scholar]
24. Atzema C, Schull MJ, Borgundvaag B, Slaughter GRD, Lee CK. ALARMED: Adverse events in Low-risk patients with chest pain Receiving continuous electrocardiographic Monitoring in the Emergency Department. A pilot study. Am J Emerg Med 2006;24(1):62-7. [View at paplisher] [DOI] [PMID] [Google Scholar]
25. Konkani A, Oakley B, Bauld TJ. Reducing hospital noise: a review of medical device alarm management Biomedical Instrumentation & Technology. 2012; 46(6):478-87. [View at paplisher] [DOI] [PMID] [Google Scholar]
26. Short K. Solving alarm fatigue with smartphone technology. Nursing2020 Critical Care. 2018;13(3):43-7. [View at paplisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






