Volume 19, Issue 2 (9-2022)
J Res Dev Nurs Midw 2022, 19(2): 45-49 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
ŞAHİN E, YAZICI S. Effects of a Parenting Preparation Course on Preferred Mode of Delivery, Fear of Childbirth, and Perception of Traumatic Childbirth in Midwifery Students. J Res Dev Nurs Midw 2022; 19 (2) :45-49
URL: http://nmj.goums.ac.ir/article-1-1412-en.html
URL: http://nmj.goums.ac.ir/article-1-1412-en.html
1- Giresun University, Faculty of Health Sciences, Department of Midwifery Department, Giresun, Turkey , ezgishn90@gmail.com
2- Istanbul Health and Technology University, Faculty of Health Sciences, Nursing Department, Istanbul, Turkey
2- Istanbul Health and Technology University, Faculty of Health Sciences, Nursing Department, Istanbul, Turkey
Full-Text [PDF 631 kb]
(420 Downloads)
| Abstract (HTML) (1302 Views)
Full-Text: (22 Views)
Introduction
Pregnancy is a physiological process that imposes a great burden and considerable stress on the female body (1-2). Pregnancy causes many important anatomical, physiological, biochemical, and psychological changes (3) to protect the developing fetus, meet metabolic needs, prepare for the birth process, and protect the health of both mother and fetus (1, 4). Pregnancy is an important and pleasant experience for every couple. However, pregnancy, childbirth, and the postpartum period may cause anxiety and fear, especially in couples who will be parents for the first time. Incomplete or inaccurate information about this process can have negative consequences. Research has shown that negative life experiences are associated with an increased risk of premature birth, low birth weight, and emotional distress in mothers (3, 5-7). Parenting preparation courses provided to parents before pregnancy and childbirth help them adapt to the pregnancy process, manage labor pains, learn and use baby care, and improve breastfeeding and parenting skills (5, 8-10). Although the findings of studies on the effectiveness of antenatal classes in different countries have been inconsistent, it has been generally observed that childbirth preparation courses have a positive effect on reducing the anxiety and stress of mothers (11-17).
The fear of childbirth is experienced not only in pregnant women but also in young individuals who think about pregnancy in the future. Most studies on this topic have focused on pregnant women or women who have given birth. To the best of our knowledge, no study has investigated midwifery students' perceptions and fears about childbirth after a parenting preparation course and a society-specific scale. However, there are very few studies on the fear of labor and preferred mode of delivery among young women who may become mothers and benefit from maternal health services. In a study by Kapısız et al. (2017) (18), nursing students had fears about childbirth. Another study reported cesarean section as the method of choice for delivery, which was associated with the perception of a high risk of vaginal delivery and fear of birth (19). In a study by Stoll et al. (2014), nursing students had fear of childbirth, and nursing students who were solely exposed to information about childbirth from the media had a higher level of fear (20).
In a previous study, pre-university students saw birth as a normal event in life and described it as painful, frightening, stressful, and miraculous (21). In another study, one-seventh of female university students who did not give birth had a fear of childbirth, and one-fourth of them was severe. In another study, it was stated that those who preferred normal vaginal delivery had low levels of traumatic childbirth perceptions and state anxiety compared to those who preferred water birth or cesarean delivery (22, 23).
This study was conducted to examine the effects of a parenting preparation course, which is given to midwifery students during an education semester, on the mode of delivery, fear of childbirth, and traumatic birth perception. We also believe that midwifery students who graduate with positive perceptions of childbirth will help other women to have a positive perception of childbirth.
Methods
The research was conducted with a quasi-experimental, pretest-posttest design. The study population consisted of 47 students (aged 18 years and over) who took the parenting preparation course in the fall semester of the academic year 2020-2021. Given the small size of the study population, all 47 students who enrolled in this course were included in the study. Students took the parenthood preparation course, 2 hours a week, for 14 weeks. In this course, psychosocial preparation to become a parent, women's health problems that will affect parenting during the preconception period, common disorders during pregnancy and precautions to be taken, nutrition and exercises during pregnancy, pregnancy and sexual life, preparation for breastfeeding during pregnancy and birth, alternative birth method, and birth as well as topics titled “management of pain, preparation for the birth and postpartum period, and parenting, and birth preparation programs” were discussed.
Data were collected using a descriptive information form, the pre-pregnancy fear of birth scale (PFBS), and the perception of traumatic birth scale (PTBS). The descriptive information form consisted of questions on characteristics such as students' age, place of residence for the longest time, place of residence during education, the experience of presence in the delivery room, observing a normal delivery, and birth preferences.
The PFBS scale was developed by Stoll et al. in 2016 (24), and the validity and reliability of the Turkish version of the scale were confirmed by Uçar and Taşhan (2018) (25). The 10-item scale measures the pre-pregnancy fear of birth in young women and men. The answers are scored based on a 6-point Likert scale. The minimum and maximum overall scores are 10 and 60, respectively. A higher total score indicates a higher level of fear (25). In the present study, Cronbach's alpha value was found to be 0.92 in the pretest and 0.93 in the posttest.
The PTBS scale was developed by Yalnız et al. in 2016 to measure traumatic birth perception in women aged 18-40 years. The scale consists of 13 questions and a single subdimension (26). The answers are scored between 0-10 from nothing to the most severe. A higher overall score indicates a higher traumatic childbirth perception (26). In this study, Cronbach's alpha value of the scale was found to be 0.93 in the pretest and 0.94 in the posttest.
Data were entered into SPSS 22.0 software and then described using numbers and percentages. The normality of data was assessed by the Kolmogorov-Smirnov test. Paired sample t-test was used to evaluate intragroup differences between the mean scale scores of fear of childbirth and traumatic childbirth perception before and after the course. The Chi-square test was applied to evaluate the relationship between pre-course and post-course birth preferences. The Pearson correlation coefficient was also used to evaluate the relationship between the scales in the pretest and posttest. The results were evaluated at 95% confidence interval and a significance level of 0.05.
Results
The mean age of the students was 20.13±0.67 years. The majority of students had a nuclear family (72.3%), an income equivalent to expenses (68.1%), graduated from Anatolian-Science High School (66.0%), chosen the midwifery department willingly (78.7%), and heard a history of difficult birth from their relatives (55.3%). In addition, 31.9% of the subjects have been previously present in delivery rooms during internships (Table 1).
The frequency of students with a fear of childbirth decreased significantly from 74.5% in the pretest to 29.8% in the posttest (Table 2). While 21.3% of the students preferred vaginal delivery in the pretest, this rate increased to 53.2% in the posttest. The frequency of students who preferred cesarean section as the preferred method of delivery increased significantly from 6.4% to 46.8%. Moreover, the frequency of students who preferred vaginal delivery with epidural anesthesia increased from 4.9% to 10.6% after the intervention (Table 2).
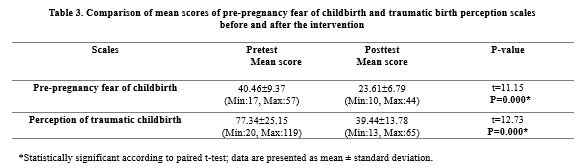
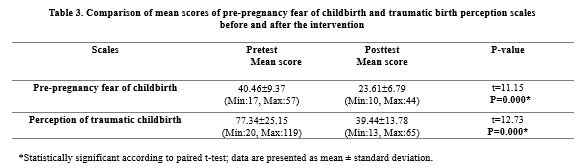
The mean score of the fear of childbirth scale decreased from 40.46±9.37 to 23.61±6.79 after the intervention (P=0.0001). The mean score of the perception of traumatic birth also decreased significantly from 77.34±25.15 in the pretest to 39.44±13.78 in the posttest (P=0.0001) (Table 3).
While it was determined that the students with high scores from PFBS and PTBS in the pre-test mostly preferred cesarean section and vaginal delivery with epidural-spinal anesthesia, it was observed that the number of students who preferred cesarean section and vaginal delivery with epidural-spinal anesthesia decreased in the post-test, and the mean scores of PFBS and PTBS also decreased statistically significantly (p<0.0001) (Table 4). There was also a strong positive correlation between PFBS and PTBS scores both in the pretest (r=0.716, P=0.0001) and posttest (r=0.716, P=0.0001).
Discussion
Prenatal parenting education is a vital part of prenatal care that is provided in many different environments all over the world (27). The purpose of such training is to develop and strengthen the ability of couples to make informed decisions appropriate to their situations (5). Along with this, the literature has defined several positive effects on maternal outcomes with better recognition of the onset of childbirth by prenatal education (5, 6). It has been demonstrated that midwifery students often have similar thoughts to the general population about the mode of child delivery before taking birth courses (28, 30). In the present study, after the parenting preparation course, the means scores of fear of childbirth and the traumatic childbirth perception decreased significantly. Moreover, the preferred mode of delivery of the students who may become expectant mothers in the future was affected by the preparation course.
Similar to our findings, Ryding et al. (2003) (28) and Karabulut et al. (2015) (30) reported that childbirth preparation training decreased the levels of fear related to childbirth. In our study, after the preparation course, there was an increased tendency towards vaginal delivery and alternative delivery and a decreased tendency towards cesarean section and vaginal delivery with epidural anesthesia. Previous studies in Turkey also showed that taking obstetrics classes increases the tendency toward vaginal delivery (31, 32-35). The fact that the students were studying in the field of health sciences could be a contributing factor in the tendency towards vaginal birth. Studies in other counties reported that 12.5-15.6% of the students preferred cesarean section over other modes of delivery (36-39). Students prefer cesarean section due to the fear of childbirth and low confidence in vaginal delivery. Educational strategies during university education can help reduce the fear of vaginal delivery and provide evidence-based information about different birth options.
Having evaluated the fear of childbirth and perception of traumatic childbirth among midwifery students, the mean score of fear of childbirth was 40.46 ±9.37 and the mean score of traumatic childbirth perception was 77.34±22.5 before the parenting preparation course. In a similar study by Güleç (2020) (40) on nursing and midwifery students, the mean score of fear of childbirth was 41.7±8.3 and the mean score of traumatic childbirth perception was 70.1±22.5 before taking the obstetrics and parenting preparation courses. This indicates the high level of fear of birth and perception of traumatic birth among midwifery and nursing students. In our study, the mean scores of traumatic childbirth perception and fear of childbirth were higher in students who preferred normal birth with epidural and cesarean section. Kapısız et al. (2017) (41) also stated that nursing students had fear of childbirth and a tendency towards cesarean section, especially due to the fear of pain related to natural childbirth. Similarly, Edmons et al. (2015) (37) stated that 61.4% of the students had fear of normal delivery. In a study by Hauck et al. (2016) (36) on Australian university students, 26.1% of the students had high fear of childbirth, and those with high scores of fear had 2.6 times more tendency for cesarean delivery. The fear of natural birth has been reported as the main reason for preferring cesarean section over natural delivery (42-45). Providing prenatal education about the benefits of normal vaginal delivery would encourage women to give normal vaginal delivery.
In the present study, the mean scores of fear of childbirth and perception of traumatic childbirth decreased significantly after the parenting preparation course, and the number of students who chose vaginal delivery and alternative birth methods increased. Other studies have also shown that childbirth preparation education is effective in reducing students' fear of childbirth and perception of traumatic childbirth. Mete et al. (2017) (46) reported that the number of women who preferred vaginal delivery with epidural anesthesia decreased after a training course, and the number of women who preferred spontaneous vaginal delivery increased. Another study reported that prenatal education helped reduce the fear of childbirth and negative thoughts about childbirth in pregnant women in the last trimester (47).
Study limitations
Since the research was conducted on a small group of people, the results of the study cannot be generalized. Furthermore, the subjects took various courses during the research and education process and may not have been able to focus much on this education.
Conclusion
Providing the parenting preparation course increased the tendency towards vaginal delivery and decreased the tendency towards cesarean section among midwifery students. Moreover, fear of
childbirth and perception of traumatic childbirth decreased after the course. Although the current high rate of cesarean section, providing prenatal education and parenting preparation courses to the young generation could shift preference toward normal delivery. In order to develop a positive attitude towards childbirth, it can be suggested to identify and eliminate the lack of knowledge and strengthen decision-making skills. It is also suggested to increase the awareness of women from all parts of society through visual media by preparing a public service announcement containing the benefits, risks, and indications of delivery methods.
Acknowledgements
We would like to thank all those who cooperated with us in conducting this study.
Funding source
Ethical statement
In order to conduct the research, approval was obtained from the scientific research ethics committee of the relevant University on 29.11.2021 with the decision number 10398. Verbal and written consent were obtained by explaining the purpose of the study to the students. The study was conducted in accordance with the Helsinki Declaration.
Conflict of interest
There are no conflicts of interest
Author contributions
All authors contributed to the study's conception and design. Material preparation, data collection, and analysis were performed by Ezgi ŞAHİN and Saadet YAZICI. The first draft of the manuscript was written by Ezgi ŞAHİN and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.



Pregnancy is a physiological process that imposes a great burden and considerable stress on the female body (1-2). Pregnancy causes many important anatomical, physiological, biochemical, and psychological changes (3) to protect the developing fetus, meet metabolic needs, prepare for the birth process, and protect the health of both mother and fetus (1, 4). Pregnancy is an important and pleasant experience for every couple. However, pregnancy, childbirth, and the postpartum period may cause anxiety and fear, especially in couples who will be parents for the first time. Incomplete or inaccurate information about this process can have negative consequences. Research has shown that negative life experiences are associated with an increased risk of premature birth, low birth weight, and emotional distress in mothers (3, 5-7). Parenting preparation courses provided to parents before pregnancy and childbirth help them adapt to the pregnancy process, manage labor pains, learn and use baby care, and improve breastfeeding and parenting skills (5, 8-10). Although the findings of studies on the effectiveness of antenatal classes in different countries have been inconsistent, it has been generally observed that childbirth preparation courses have a positive effect on reducing the anxiety and stress of mothers (11-17).
The fear of childbirth is experienced not only in pregnant women but also in young individuals who think about pregnancy in the future. Most studies on this topic have focused on pregnant women or women who have given birth. To the best of our knowledge, no study has investigated midwifery students' perceptions and fears about childbirth after a parenting preparation course and a society-specific scale. However, there are very few studies on the fear of labor and preferred mode of delivery among young women who may become mothers and benefit from maternal health services. In a study by Kapısız et al. (2017) (18), nursing students had fears about childbirth. Another study reported cesarean section as the method of choice for delivery, which was associated with the perception of a high risk of vaginal delivery and fear of birth (19). In a study by Stoll et al. (2014), nursing students had fear of childbirth, and nursing students who were solely exposed to information about childbirth from the media had a higher level of fear (20).
In a previous study, pre-university students saw birth as a normal event in life and described it as painful, frightening, stressful, and miraculous (21). In another study, one-seventh of female university students who did not give birth had a fear of childbirth, and one-fourth of them was severe. In another study, it was stated that those who preferred normal vaginal delivery had low levels of traumatic childbirth perceptions and state anxiety compared to those who preferred water birth or cesarean delivery (22, 23).
This study was conducted to examine the effects of a parenting preparation course, which is given to midwifery students during an education semester, on the mode of delivery, fear of childbirth, and traumatic birth perception. We also believe that midwifery students who graduate with positive perceptions of childbirth will help other women to have a positive perception of childbirth.
Methods
The research was conducted with a quasi-experimental, pretest-posttest design. The study population consisted of 47 students (aged 18 years and over) who took the parenting preparation course in the fall semester of the academic year 2020-2021. Given the small size of the study population, all 47 students who enrolled in this course were included in the study. Students took the parenthood preparation course, 2 hours a week, for 14 weeks. In this course, psychosocial preparation to become a parent, women's health problems that will affect parenting during the preconception period, common disorders during pregnancy and precautions to be taken, nutrition and exercises during pregnancy, pregnancy and sexual life, preparation for breastfeeding during pregnancy and birth, alternative birth method, and birth as well as topics titled “management of pain, preparation for the birth and postpartum period, and parenting, and birth preparation programs” were discussed.
Data were collected using a descriptive information form, the pre-pregnancy fear of birth scale (PFBS), and the perception of traumatic birth scale (PTBS). The descriptive information form consisted of questions on characteristics such as students' age, place of residence for the longest time, place of residence during education, the experience of presence in the delivery room, observing a normal delivery, and birth preferences.
The PFBS scale was developed by Stoll et al. in 2016 (24), and the validity and reliability of the Turkish version of the scale were confirmed by Uçar and Taşhan (2018) (25). The 10-item scale measures the pre-pregnancy fear of birth in young women and men. The answers are scored based on a 6-point Likert scale. The minimum and maximum overall scores are 10 and 60, respectively. A higher total score indicates a higher level of fear (25). In the present study, Cronbach's alpha value was found to be 0.92 in the pretest and 0.93 in the posttest.
The PTBS scale was developed by Yalnız et al. in 2016 to measure traumatic birth perception in women aged 18-40 years. The scale consists of 13 questions and a single subdimension (26). The answers are scored between 0-10 from nothing to the most severe. A higher overall score indicates a higher traumatic childbirth perception (26). In this study, Cronbach's alpha value of the scale was found to be 0.93 in the pretest and 0.94 in the posttest.
Data were entered into SPSS 22.0 software and then described using numbers and percentages. The normality of data was assessed by the Kolmogorov-Smirnov test. Paired sample t-test was used to evaluate intragroup differences between the mean scale scores of fear of childbirth and traumatic childbirth perception before and after the course. The Chi-square test was applied to evaluate the relationship between pre-course and post-course birth preferences. The Pearson correlation coefficient was also used to evaluate the relationship between the scales in the pretest and posttest. The results were evaluated at 95% confidence interval and a significance level of 0.05.
Results
The mean age of the students was 20.13±0.67 years. The majority of students had a nuclear family (72.3%), an income equivalent to expenses (68.1%), graduated from Anatolian-Science High School (66.0%), chosen the midwifery department willingly (78.7%), and heard a history of difficult birth from their relatives (55.3%). In addition, 31.9% of the subjects have been previously present in delivery rooms during internships (Table 1).
The frequency of students with a fear of childbirth decreased significantly from 74.5% in the pretest to 29.8% in the posttest (Table 2). While 21.3% of the students preferred vaginal delivery in the pretest, this rate increased to 53.2% in the posttest. The frequency of students who preferred cesarean section as the preferred method of delivery increased significantly from 6.4% to 46.8%. Moreover, the frequency of students who preferred vaginal delivery with epidural anesthesia increased from 4.9% to 10.6% after the intervention (Table 2).
The mean score of the fear of childbirth scale decreased from 40.46±9.37 to 23.61±6.79 after the intervention (P=0.0001). The mean score of the perception of traumatic birth also decreased significantly from 77.34±25.15 in the pretest to 39.44±13.78 in the posttest (P=0.0001) (Table 3).
While it was determined that the students with high scores from PFBS and PTBS in the pre-test mostly preferred cesarean section and vaginal delivery with epidural-spinal anesthesia, it was observed that the number of students who preferred cesarean section and vaginal delivery with epidural-spinal anesthesia decreased in the post-test, and the mean scores of PFBS and PTBS also decreased statistically significantly (p<0.0001) (Table 4). There was also a strong positive correlation between PFBS and PTBS scores both in the pretest (r=0.716, P=0.0001) and posttest (r=0.716, P=0.0001).
Discussion
Prenatal parenting education is a vital part of prenatal care that is provided in many different environments all over the world (27). The purpose of such training is to develop and strengthen the ability of couples to make informed decisions appropriate to their situations (5). Along with this, the literature has defined several positive effects on maternal outcomes with better recognition of the onset of childbirth by prenatal education (5, 6). It has been demonstrated that midwifery students often have similar thoughts to the general population about the mode of child delivery before taking birth courses (28, 30). In the present study, after the parenting preparation course, the means scores of fear of childbirth and the traumatic childbirth perception decreased significantly. Moreover, the preferred mode of delivery of the students who may become expectant mothers in the future was affected by the preparation course.
Similar to our findings, Ryding et al. (2003) (28) and Karabulut et al. (2015) (30) reported that childbirth preparation training decreased the levels of fear related to childbirth. In our study, after the preparation course, there was an increased tendency towards vaginal delivery and alternative delivery and a decreased tendency towards cesarean section and vaginal delivery with epidural anesthesia. Previous studies in Turkey also showed that taking obstetrics classes increases the tendency toward vaginal delivery (31, 32-35). The fact that the students were studying in the field of health sciences could be a contributing factor in the tendency towards vaginal birth. Studies in other counties reported that 12.5-15.6% of the students preferred cesarean section over other modes of delivery (36-39). Students prefer cesarean section due to the fear of childbirth and low confidence in vaginal delivery. Educational strategies during university education can help reduce the fear of vaginal delivery and provide evidence-based information about different birth options.
Having evaluated the fear of childbirth and perception of traumatic childbirth among midwifery students, the mean score of fear of childbirth was 40.46 ±9.37 and the mean score of traumatic childbirth perception was 77.34±22.5 before the parenting preparation course. In a similar study by Güleç (2020) (40) on nursing and midwifery students, the mean score of fear of childbirth was 41.7±8.3 and the mean score of traumatic childbirth perception was 70.1±22.5 before taking the obstetrics and parenting preparation courses. This indicates the high level of fear of birth and perception of traumatic birth among midwifery and nursing students. In our study, the mean scores of traumatic childbirth perception and fear of childbirth were higher in students who preferred normal birth with epidural and cesarean section. Kapısız et al. (2017) (41) also stated that nursing students had fear of childbirth and a tendency towards cesarean section, especially due to the fear of pain related to natural childbirth. Similarly, Edmons et al. (2015) (37) stated that 61.4% of the students had fear of normal delivery. In a study by Hauck et al. (2016) (36) on Australian university students, 26.1% of the students had high fear of childbirth, and those with high scores of fear had 2.6 times more tendency for cesarean delivery. The fear of natural birth has been reported as the main reason for preferring cesarean section over natural delivery (42-45). Providing prenatal education about the benefits of normal vaginal delivery would encourage women to give normal vaginal delivery.
In the present study, the mean scores of fear of childbirth and perception of traumatic childbirth decreased significantly after the parenting preparation course, and the number of students who chose vaginal delivery and alternative birth methods increased. Other studies have also shown that childbirth preparation education is effective in reducing students' fear of childbirth and perception of traumatic childbirth. Mete et al. (2017) (46) reported that the number of women who preferred vaginal delivery with epidural anesthesia decreased after a training course, and the number of women who preferred spontaneous vaginal delivery increased. Another study reported that prenatal education helped reduce the fear of childbirth and negative thoughts about childbirth in pregnant women in the last trimester (47).
Study limitations
Since the research was conducted on a small group of people, the results of the study cannot be generalized. Furthermore, the subjects took various courses during the research and education process and may not have been able to focus much on this education.
Conclusion
Providing the parenting preparation course increased the tendency towards vaginal delivery and decreased the tendency towards cesarean section among midwifery students. Moreover, fear of
childbirth and perception of traumatic childbirth decreased after the course. Although the current high rate of cesarean section, providing prenatal education and parenting preparation courses to the young generation could shift preference toward normal delivery. In order to develop a positive attitude towards childbirth, it can be suggested to identify and eliminate the lack of knowledge and strengthen decision-making skills. It is also suggested to increase the awareness of women from all parts of society through visual media by preparing a public service announcement containing the benefits, risks, and indications of delivery methods.
Acknowledgements
We would like to thank all those who cooperated with us in conducting this study.
Funding source
Ethical statement
In order to conduct the research, approval was obtained from the scientific research ethics committee of the relevant University on 29.11.2021 with the decision number 10398. Verbal and written consent were obtained by explaining the purpose of the study to the students. The study was conducted in accordance with the Helsinki Declaration.
Conflict of interest
There are no conflicts of interest
Author contributions
All authors contributed to the study's conception and design. Material preparation, data collection, and analysis were performed by Ezgi ŞAHİN and Saadet YAZICI. The first draft of the manuscript was written by Ezgi ŞAHİN and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.



Type of Study: Original Article |
Subject:
Midwifery
References
1. Coşkun AM. Kadın Sağlığı ve Hastalıkları Hemşireliği El Kitabı. İstanbul: Koç Üniversitesi Yayınları. 2016 [View at paplisher] [Google Scholar]
2. Taşkın, L. Doğum ve Kadın Sağlığı Hemşireliği, 13. Basım. Ankara: Akademisyen Kitabevi. 2016 [View at paplisher] [Google Scholar]
3. Facchinetti F, Ottolini F. Stress and preterm delivery. Journal of Psychosomatic Obstetrics & Gynecology. 2004;25(1):1-2. [View at paplisher] [DOI] [Google Scholar]
4. Ayhan A, Durukan T, Günalp S, Gürgan, T, Önderoğlu LS, Yaralı, H, Yüce K. Temel Kadın Hastalıkları ve Doğum Bilgisi. 2. Baskı, Ankara: Güneş Kitabevi. 2008 [View at paplisher] [Google Scholar]
5. Axelsen SF, Brixval CS, Due, Koushede V. Integrating couple relationship education in antenatal education-a study of perceived relevance among expectant Danish parents. Sexual & Reproductive Healthcare. 2014;5(4):174-175. [View at paplisher] [DOI] [Google Scholar]
6. Brixval CS, Axelsen SF, Lauemøller SG, Andersen SK, Due P, Koushede V. The effect of antenatal education in small classes on obstetric and psycho-social outcomes-a systematic review. Systematic reviews. 2015;4(1):1-9. [View at paplisher] [DOI] [Google Scholar]
7. Gökçe İsbir G, İnci F, Önal H, Yıldız PD. The effects of antenatal education on fear of childbirth, maternal self-efficacy and post-traumatic stress disorder (PTSD) symptoms following childbirth: an experimental study. Applied nursing research. 2016;32:227-232. [View at paplisher] [DOI] [Google Scholar]
8. El-Kurdy R, Hassan SI, Hassan NF, El-Nemer A. Antenatal education on childbirth self-efficacy for Egyptian primiparous women: A randomized control trial. IOSR Journal of Nursing and Health Science. 2017;6(4):15-23. [View at paplisher] [DOI] [Google Scholar]
9. Jaddoe VW. Antenatal education programmes: do they work?. Lancet (London, England). 2009;374(9693):863-864. [View at paplisher] [DOI] [Google Scholar]
10. Hatamleh R, Abujilban S, AbuAbed A, Abuhammad S. The effects of a childbirth preparation course on birth outcomes among nulliparous Jordanian women. Midwifery. 2019; 72:23-29. [View at paplisher] [DOI] [Google Scholar]
11. Bergström, M, Kieler H, Waldenström U. Effects of natural childbirth preparation versus standard antenatal education on epidural rates, experience of childbirth and parental stres in mothers and fathers: a randomised controlled multicentre trial. BJOG An International Journal of Obstetrics and Gynaecology. 2009;1167-1176 [View at paplisher] [DOI] [Google Scholar]
12. Feinberg, ME, Kan, ML. Establishing family foundations: intervention effects on coparenting, parent/infant well-being, and parent-child relations. Journal of family psychology : JFP : journal of the Division of Family Psychology of the American Psychological Association (Division 43). 2008; 22(2):253-263. [View at paplisher] [DOI] [Google Scholar]
13. Rossiter JC. The effect of a culture-specific education program to promote breastfeeding among Vietnamese women in Sydney. International journal of nursing studies. 1994; 31(4): 369-379. [View at paplisher] [DOI] [Google Scholar]
14. Werner A, Uldbjerg N, Zachariae R, Rosen G, Nohr EA. Self-hypnosis for coping with labour pain: a randomised controlled trial. BJOG : an international journal of obstetrics and gynaecology. 2013; 120(3): 346-353. [View at paplisher] [DOI] [Google Scholar]
15. Noel-Weiss J, Rupp A, Cragg B, Bassett V, Woodend AK. Randomized controlled trial to determine effects of prenatal breastfeeding workshop on maternal breastfeeding self-efficacy and breastfeeding duration. Journal of obstetric, gynecologic, and neonatal nursing. JOGNN. 2006; 35(5):616-624. [View at paplisher] [DOI] [Google Scholar]
16. Rouhe H, Salmela-Aro K, Toivanen R, Tokola M, Halmesmäki E, Saisto T. Obstetric outcome after intervention for severe fear of childbirth in nulliparous women - randomised trial. BJOG : an international journal of obstetrics and gynaecology. 2013; 120(1): 75-84. [View at paplisher] [DOI] [Google Scholar]
17. Lara MA, Navarro C, Navarrete L. Outcome results of a psycho-educational intervention in pregnancy to prevent PPD: a randomized control trial. Journal of affective disorders. 2010; 122(1-2): 109-117. [View at paplisher] [DOI] [Google Scholar]
18. Kapısız Ö, Karaca A, Süzer Özkan F, Gülen Savaş, H. Birth Perception of Nursing Students. Journal of Duzce University Institute of Health Sciences. 2019;7(3):156-160. [View at paplisher] [Google Scholar]
19. Weeks FH, Sadler M, Stoll K. Preference for caesarean attitudes toward birth in a Chilean sample of young adults. Women and birth : journal of the Australian College of Midwives. 2020;33(2):159-165. [View at paplisher] [DOI] [Google Scholar]
20. Stoll K, Hall W, Janssen P, Carty E. Why are young Canadians afraid of birth? A survey study of childbirth fear and birth preferences among Canadian University students. Midwifery. 2014;30(2):220-226. [View at paplisher] [DOI] [Google Scholar]
21. Saroli Palumbo C, Hsu R, Tomkinson J, Klein MC. Pre-University Students' Attitudes and Beliefs about Childbirth: Implications for Reproductive Health and Maternity Care. The Canadian Journal Of Midwifery Research And Practice. 2012;11(2):27-37. [View at paplisher] [Google Scholar]
22. Žigić Antić L, Nakić Radoš S, Jokić-Begić N. Are nonpregnant women afraid of childbirth? Prevalence and predictors of fear of childbirth in students. J Psychosom Obstet Gynaecol. 2019;40(3):226-231. doi: 10.1080/0167482X.2018.1470162. [View at paplisher] [DOI] [Google Scholar]
23. Aslantekin-Özçoban, F, Türkmen, H, Yalnız-Dilcen, H. Factors that affect the traumatic childbirth perceptions of midwifery and nursing students: The case of Turkey. European journal of midwifery. 2021;5:34. [View at paplisher] [DOI] [Google Scholar]
24. Stoll K, Hauck Y, Downe S, Edmonds J, Gross MM, Malott A, McNiven P, Swift E, Thomson G, Hall WA. Cross-cultural development and psychometric evaluation of a measure to assess fear of childbirth prior to pregnancy. Sexual & reproductive healthcare:official journal of the Swedish Association of Midwives. 2016;8:49-54. [View at paplisher] [DOI] [Google Scholar]
25. Uçar T, Taşhan ST. Turkish version of the pre-pregnancy fear of childbirth scale: a validity and reliability study for women and men. Acıbadem University Journal of Health Sciences .2018; 9(3):289-96. [View at paplisher] [Google Scholar]
26. Yalnız H, Canan F, Genç RE, Kuloğlu MM, Geçici Ö. Development of the traumatic birth perception scale. Turkish Journal of Medicine. 2016;8(3):81-88. [View at paplisher] [Google Scholar]
27. Adams, J, Lui, C. W, Sibbritt, D, Broom, A, Wardle, J, Homer C. Attitudes and referral practices of maternity care professionals with regard to complementary and alternative medicine: an integrative review. Journal of advanced nursing. 2011;67(3):472-483. [View at paplisher] [DOI] [Google Scholar]
28. Ryding EL, Persson A, Onell C, Kvist L. An evaluation of midwives' counseling of pregnant women in fear of childbirth. Acta Obstet Gynecol Scand. 2003;82(1):10-17. [View at paplisher] [DOI] [Google Scholar]
29. Hatamleh R, Abujilban S, Abuhammad S. The effects of a childbirth preparation course on birth outcomes among nulliparous Jordanian women. Midwifery. 2019;72:23-29. [View at paplisher] [DOI] [Google Scholar]
30. Karabulut Ö, Coşkuner Potur D, Doğan Merih Y, Cebeci Mutlu S, Demirci N. Does Antenatal Education Reduce Fear of Childbirth? International Nursing Review. 2015; 63(1):60-67. [View at paplisher] [DOI] [Google Scholar]
31. Aksu H, Özsoy S. Midwifery and Nursing students' birth preferences and influencing factors. Journal of Health Sciences. 2015;24:44-8. [View at paplisher] [Google Scholar]
32. Aydoğdu SGM, Uzun B, Özsoy Ü. Views of midwifery students on normal vaginal delivery. Andrology Bulletin. 2018;20:78−84. [View at paplisher] [Google Scholar]
33. Tektaş E, Bozkurt G, Ergin E, Sezgin S. Birth preferences of the students of the Faculty of Health Sciences and influencing factors. Çukurova Medical Journal. 2018;43 (Ek 1):63-69. [View at paplisher] [DOI] [Google Scholar]
34. Karaca PP, Koyuncu GR. Determining the thoughts of the students studying at the vocational school of health services about their birth type preferences. Journal of İnönü University Vocational School of Health Services. 2018;3(1):1-8. [View at paplisher] [Google Scholar]
35. Kadıoğlu M, Şahin N. University students' opinions, preferences and influencing factors on the way of birth. KASHED. 2019;5(2):43-69. [View at paplisher] [Google Scholar]
36. Hauck YL, Stoll KH, Hall WA, Downie J. Association between childbirth attitudes and fear on birth preferences of a future generation of Australian parents. Women Birth. 2016;29(6):511-17. [View at paplisher] [DOI] [Google Scholar]
37. Edmonds JK, Cwiertniewicz T, Stoll K. Childbirth education prior to pregnancy? Survey findings of childbirth preferences and attitudes among young women. Journal of Perinatal Education. 2015;24(2):93-101. [View at paplisher] [DOI] [Google Scholar]
38. Lampman C, Phelps A. College Students; Knowledge and Attitudes About Cesarean Birth. Birth. 1997;3:159-164. [View at paplisher] [DOI] [Google Scholar]
39. Gallagher F, Bell, Waddell G, Benoît A, Côté N. Requesting Cesareans without Medical Indications: An Option Being Considered by Young Canadian Women. Birth. 2012;39:39-47. [View at paplisher] [DOI] [Google Scholar]
40. Güleç D. The Effect of Birth and Parenthood Preparation Lesson on Fear of Birth and Perception of Traumatic Birth in Nursing Students. Journal of Higher Education and Science. 2020; 10(3): 423-428. [View at paplisher] [DOI] [Google Scholar]
41. Kapısız Ö, Karaca A, Özkan FS, Savaş HG. Birth perception of nursing students. Journal of Duzce University Institute of Health Sciences. 2017;(3): 156- 60. [View at paplisher] [Google Scholar]
42. Loke AY, Davies L, Li S. Factors influencing the decision that women make on their mode of delivery: the Health Belief Model. Loke et al. BMC Health Services Research 2015;15:27. [View at paplisher] [DOI] [Google Scholar]
43. Türkmen H, Yalniz Dilcen H, Akin B. The Effect of Labor Comfort on Traumatic Childbirth Perception, Post-Traumatic Stress Disorder, and Breastfeeding. Breastfeed Med. 2020;15(12):779-788. [View at paplisher] [DOI] [Google Scholar]
44. Ergöl Ş, Kürtüncü M. Factors affecting the cesarean section preferences of women in a university hospital. Journal of Hacettepe University Faculty of Nursing. 2014;26-34. [View at paplisher] [Google Scholar]
45. Gözükara F, Eroğlu K. Factors affecting the preferences of women who have given birth for the first time (primiparous). Hacettepe University Faculty of Health Sciences Journal of Nursing. 2008; 32-46. [View at paplisher] [Google Scholar]
46. Mete S, Cicek O, Alus Tokat M, Camlibel M, Uludag E. The effect of birth preparation classes on fear of birth, birth preference and birth readiness. Turkey Clinics J Nurs Sci. 2017; 9(3): 201-6. [View at paplisher] [DOI] [Google Scholar]
47. Subaşı B, Özcan H, Pekçetin S, Göker B, Tunç S, Budak B. The Effect of Birth Education on Birth Anxiety and Fear. Selcuk Medical Journal. 2013;29(4):165- 167. [View at paplisher] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





