Volume 20, Issue 2 (10-2023)
J Res Dev Nurs Midw 2023, 20(2): 1-4 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
omidi A, Rajabalipour M, arab S, Mokhtari Sorkhan T. Assessment of the I-PASS program on nursing shift handover in CCU and ICU wards: The use of a new approach in the nursing profession. J Res Dev Nurs Midw 2023; 20 (2) :1-4
URL: http://nmj.goums.ac.ir/article-1-1379-en.html
URL: http://nmj.goums.ac.ir/article-1-1379-en.html
1- School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
2- Department of Health Education and Promotion, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
3- Student Research Committee, School of Nursing and Midwifery, Bam University of Medical Sciences, Bam, Iran.
4- Nursing & Midwifery Faculty, Bam University of Medical Sciences, Bam, Iran. ,arianmokhtari2@gmail.com
2- Department of Health Education and Promotion, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
3- Student Research Committee, School of Nursing and Midwifery, Bam University of Medical Sciences, Bam, Iran.
4- Nursing & Midwifery Faculty, Bam University of Medical Sciences, Bam, Iran. ,
Full-Text [PDF 511 kb]
(1944 Downloads)
| Abstract (HTML) (2236 Views)
Full-Text: (417 Views)
Introduction
Shift handover is one of the critical tasks and major challenges among health care workers (HCWs) in hospitals. It is estimated that approximately 70% of serious adverse events in hospitals can be attributed to communication problems related to shift handover during shift changes. Hence, shift handover has been considered an influential and fundamental factor in patient safety (1-3), which can lead to different unforeseen events during shift changes among HCWs (4). However, the most common events are the omission of important information and incorrect transfer of information during shift changes (5-7). Frequent changes in shift schedules increase the likelihood of errors during shift changes, which can lead to significant issues for patients and subsequent events. Studies have shown that poor communication among HCWs is the principal cause of two-thirds of sensitive events in patients' security and safety, which may lead to approximately 80% of serious medical errors (4). In the SBAR (situation-background-assessment-recommendation) technique, important items (such as resuscitation status and pending test results) are handed over with low frequency, posing a potential limitation to the effectiveness of this method (8). Accordingly, these errors and associated consequences have become more apparent in recent years, drawing significant attention to this issue (9, 10). In addition, due to staff shortages and high workload of HCWs in some hospitals, especially during the COVID-19 pandemic, the care process often occurs without understanding patients' conditions, studying their history, and routine treatment measurements in hospital wards (1).
The Patient Safety Monitoring Committee analyzed more than 3000 events related to shift handover from 1995 to 2005. The findings identified poor communication as the leading cause of medical errors, with approximately 50% of the communication weaknesses occurring during shift changes (11). Therefore, the lack of good communication during shift changes and patient handovers can be identified as one of the primary challenges that HCWs face in health centers (12). Many HCWs use the SBAR technique. Although this technique has been used by nurses, physicians, and other HCWs, it is only effective when time is limited and may not be beneficial and useful for patients who have complicated diagnoses or special conditions (4). Accordingly, a new program called I-PASS (illness severity, patient summary, action list, situation awareness and contingency planning, and synthesis by receiver) has been developed as an evidence-based patient delivery program to improve communication among HCWs in hospitals. This program is an organized framework to establish effective communication among HCWs during shift changes (13) and reduce medical errors (12, 14, 15). A review of similar studies showed that the I-PASS program could be a useful and effective method in the management of shift handover (4, 13, 16). A study showed that 81% to 96% of participants agree and strongly agree with the use of the I-PASS program (17). Another study showed that the I-PASS program could decrease the rate of medical errors from 33.8% to 18.3% and adverse events from 3.3% to 1.5% (18). In addition, the implementation of the I-PASS program in children’s care services in North America was associated with improved communication and reduced medical errors and adverse events in preventive medical treatment decisions (19). Also, a study indicated that the I-PASS program led to a 23% reduction in medical errors and a 30% reduction in adverse events among patients (it reduced medical error rates from 1349 to 981 events) (20). The occurrence of side effects in preventive treatment decisions decreased from 261 to 173 cases, serious errors decreased from 1088 to 808, and medication errors decreased from 660 to 580 items in 9 studied hospitals before and after the application of the I-PASS program, respectively (20).
Few studies have been conducted on nursing shift handover methods and programs in Iran (1, 2). Due to the sensitive and specific conditions of patients in critical care unit (CCU) and intensive care unit (ICU) wards, it is necessary for nurses to deliver a large amount of useful information to the next shift in a short time. If the important clinical information of the patients is forgotten during shift changes, irreparable damages will occur. Also, the application of the I-PASS program and its impact on nurses' workflow in different hospital wards have not been evaluated sufficiently
Methods
Design and participants
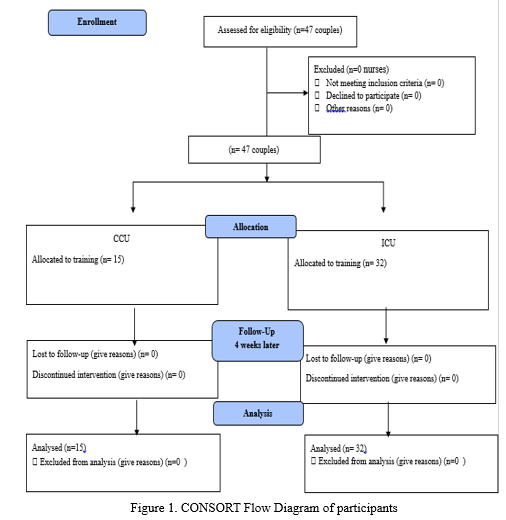
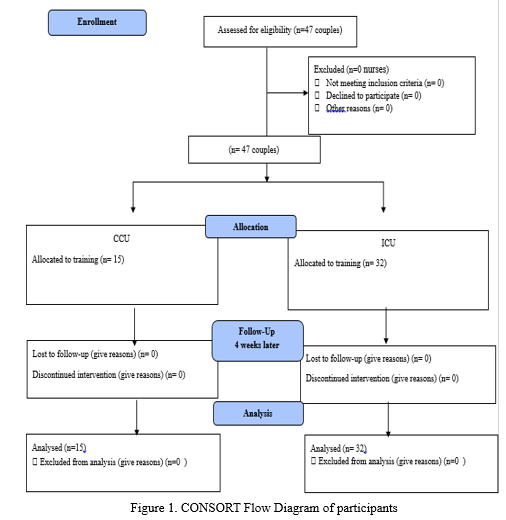
This study used a quasi-experimental design with a before-and-after method (without a control group) to assess the effect of the I-PASS program on nurses after the program implementation. It was performed during shift changes in CCU and ICU wards in Pasteur Hospital in Bam City in southeastern Iran from January to March 2021. Inclusion criteria were working in ICU and CCU wards and willingness to participate in the study. The exclusion criterion was the person's absence in the program sessions. Before implementing the I-PASS program, the common method (SBAR method) was used for shift handover in the target wards. Before starting the monitoring, pretest forms were distributed among all participants to collect pretest data. Then, the intervention was implemented to use the I-PASS program. After teaching the program, posttest data were collected. Due to the total number of nurses and availability conditions, the sample size was selected by the census method. Finally, 47 nurses (32 nurses in the ICU and 15 nurses in the CCU) were enrolled in the study, and the effects of the I-PASS program in handover were evaluated.
Instrument
The I-PASS Handoff Assessment Tool (as a data collection instrument) was translated from English into Persian. This tool has 20 specific items for the assessment of the I-PASS program. It was first used in a study conducted in the United States and Canada in 2014 to assess the effect of the I-PASS program on promoting patient safety (3). The reliability and validity of this tool were confirmed in another study by Starmer et al (4). First, a request was sent via email to the designer of the I-PASS Handoff Assessment Tool, and the objectives of the study were explained to obtain translation permission. Then, the forward-only translation method was used to translate the assessment tool by 2 multilingual translators. They were proficient in English, but their native language was Persian. They had no prior knowledge or familiarity with the assessment tool. One of the translators was responsible for translating the forms from English to Persian, while the other translator reviewed and approved the translation. After confirming the forward translation, 10 nursing experts with master and PhD degrees identified and eliminated incomprehensible, inappropriate, non-specialized components of the assessment tool. Finally, to ensure the standardization of the tool, the translations were combined, and a single version that included 20 items was created. The items used in the Persian version were not significantly different from the original one, and no change occurred in any item. The face validity of the assessment tool was assessed and confirmed by the target group. Next, the validity of 20 items was examined by 10 nursing professors, and the content validity index (CVI) and content validity ratio (CVR) were found to be equal to 0.6-1. The checklist was also completed by 21 nurses before and after the intervention to determine its reliability and internal stability. Eventually, the Cronbach α coefficient was found to be equal to 0.80, confirming the checklist reliability. Demographic variables include age, gender, educational degree, ward, and shift time. This assessment tool included 20 items that were assessed using a 5-point Likert scale from 1 (complete disagreement) to 5 (complete agreement).
The I-PASS program was taught to nurses based on 5 principles. The first principle is “illness severity”; in this principle, the nurse must be aware of the severity of the patient's illness and inform the next nurse. Under this principle, there are 3 situations: (i) The client's condition is relatively good and recovering, (ii) the client's condition is relatively bad and needs more care, and (iii) the client's condition is bad and in an emergency situation. The second principle is “patient summary”; in this principle, the nurse is informed about the patient's illness and things such as the reason for admission, initial symptoms, patient information, changes in the diagnosis and treatment plan, initial weight and changes in the patient's weight, etc. The third principle is “action list”; in this principle, the nurse understands the tasks that have to do in his/her shift, and in addition to planning and scheduling, program priorities should be taken into consideration. The responsibility of the next shift nurse should be fully stated, and the list of tasks performed should be specified. In addition, the nurse must be aware of the documentation of the heart and respiratory conditions and necessary instructions for the care of the patient (such as diet) and perform the necessary actions during his/her shift. The fourth principle is “situation awareness and contingency planning”; in this principle, the nurse must be aware of important events, such as the patient’s dangerous diseases (such as AIDS, hepatitis, etc). The fifth principle is “synthesis by receiver,” which includes giving the next nurse the opportunity to ask questions and summarize the contents expressed by the nurse from the previous shift.
The pretest was performed among 47 nurses. Before implementing the program, all participants in both ICU and CCU wards completed the Persian version of the I-PASS Handoff Assessment Tool through self-report. They were provided with comprehensive explanations regarding the objectives, work process, and confidentiality policy. All nurses voluntarily participated in this research. They received shift-handover training based on the I-PASS program for 4 weeks. Training courses were organized with the support of ward supervisors and held once a week for 4 weeks. Each session lasted for 45 minutes, providing participants with the necessary instruction and guidance on the I-PASS program. Due to the COVID-19 pandemic, the valid and reliable instrument items for assessing I-PASS were remotely explained to the participants by the researcher using Adobe Connect software. In addition, during the program implementation, nurses were asked to use the Persian version of I-PASS assessment tool during their shift work in CCU and ICU wards. After 4 weeks, in the posttest, forms were again completed by all nurses, and the data were collected for final analysis. In other words, the SBAR method, which is one of the most common methods, was routinely used. Before implementing the I-PASS program, the pretest data were collected, and I-PASS scores were evaluated to measure the participants' familiarity with this program. Then, the I-PASS program was implemented for 4 weeks, and after the end of this period, the posttest data were collected and compared with the pretest data (CONSORT [Consolidated Standards of Reporting Trials] diagram) (Figure 1).
Data analysis
Data analysis was performed using SPSS version 25 (SPSS Inc, Chicago, IL, USA) and mean and SD to determine demographical factors and variable frequencies. The chi-square test and independent t test were also used for the assessment of significance and correlation between before and after training scores. In addition, the paired t test was used to compare the mean score of nursing shift handover before and after training in each ward. P values less than 0.05 were considered statistically significant.
Shift handover is one of the critical tasks and major challenges among health care workers (HCWs) in hospitals. It is estimated that approximately 70% of serious adverse events in hospitals can be attributed to communication problems related to shift handover during shift changes. Hence, shift handover has been considered an influential and fundamental factor in patient safety (1-3), which can lead to different unforeseen events during shift changes among HCWs (4). However, the most common events are the omission of important information and incorrect transfer of information during shift changes (5-7). Frequent changes in shift schedules increase the likelihood of errors during shift changes, which can lead to significant issues for patients and subsequent events. Studies have shown that poor communication among HCWs is the principal cause of two-thirds of sensitive events in patients' security and safety, which may lead to approximately 80% of serious medical errors (4). In the SBAR (situation-background-assessment-recommendation) technique, important items (such as resuscitation status and pending test results) are handed over with low frequency, posing a potential limitation to the effectiveness of this method (8). Accordingly, these errors and associated consequences have become more apparent in recent years, drawing significant attention to this issue (9, 10). In addition, due to staff shortages and high workload of HCWs in some hospitals, especially during the COVID-19 pandemic, the care process often occurs without understanding patients' conditions, studying their history, and routine treatment measurements in hospital wards (1).
The Patient Safety Monitoring Committee analyzed more than 3000 events related to shift handover from 1995 to 2005. The findings identified poor communication as the leading cause of medical errors, with approximately 50% of the communication weaknesses occurring during shift changes (11). Therefore, the lack of good communication during shift changes and patient handovers can be identified as one of the primary challenges that HCWs face in health centers (12). Many HCWs use the SBAR technique. Although this technique has been used by nurses, physicians, and other HCWs, it is only effective when time is limited and may not be beneficial and useful for patients who have complicated diagnoses or special conditions (4). Accordingly, a new program called I-PASS (illness severity, patient summary, action list, situation awareness and contingency planning, and synthesis by receiver) has been developed as an evidence-based patient delivery program to improve communication among HCWs in hospitals. This program is an organized framework to establish effective communication among HCWs during shift changes (13) and reduce medical errors (12, 14, 15). A review of similar studies showed that the I-PASS program could be a useful and effective method in the management of shift handover (4, 13, 16). A study showed that 81% to 96% of participants agree and strongly agree with the use of the I-PASS program (17). Another study showed that the I-PASS program could decrease the rate of medical errors from 33.8% to 18.3% and adverse events from 3.3% to 1.5% (18). In addition, the implementation of the I-PASS program in children’s care services in North America was associated with improved communication and reduced medical errors and adverse events in preventive medical treatment decisions (19). Also, a study indicated that the I-PASS program led to a 23% reduction in medical errors and a 30% reduction in adverse events among patients (it reduced medical error rates from 1349 to 981 events) (20). The occurrence of side effects in preventive treatment decisions decreased from 261 to 173 cases, serious errors decreased from 1088 to 808, and medication errors decreased from 660 to 580 items in 9 studied hospitals before and after the application of the I-PASS program, respectively (20).
Few studies have been conducted on nursing shift handover methods and programs in Iran (1, 2). Due to the sensitive and specific conditions of patients in critical care unit (CCU) and intensive care unit (ICU) wards, it is necessary for nurses to deliver a large amount of useful information to the next shift in a short time. If the important clinical information of the patients is forgotten during shift changes, irreparable damages will occur. Also, the application of the I-PASS program and its impact on nurses' workflow in different hospital wards have not been evaluated sufficiently
Methods
Design and participants
This study used a quasi-experimental design with a before-and-after method (without a control group) to assess the effect of the I-PASS program on nurses after the program implementation. It was performed during shift changes in CCU and ICU wards in Pasteur Hospital in Bam City in southeastern Iran from January to March 2021. Inclusion criteria were working in ICU and CCU wards and willingness to participate in the study. The exclusion criterion was the person's absence in the program sessions. Before implementing the I-PASS program, the common method (SBAR method) was used for shift handover in the target wards. Before starting the monitoring, pretest forms were distributed among all participants to collect pretest data. Then, the intervention was implemented to use the I-PASS program. After teaching the program, posttest data were collected. Due to the total number of nurses and availability conditions, the sample size was selected by the census method. Finally, 47 nurses (32 nurses in the ICU and 15 nurses in the CCU) were enrolled in the study, and the effects of the I-PASS program in handover were evaluated.
Instrument
The I-PASS Handoff Assessment Tool (as a data collection instrument) was translated from English into Persian. This tool has 20 specific items for the assessment of the I-PASS program. It was first used in a study conducted in the United States and Canada in 2014 to assess the effect of the I-PASS program on promoting patient safety (3). The reliability and validity of this tool were confirmed in another study by Starmer et al (4). First, a request was sent via email to the designer of the I-PASS Handoff Assessment Tool, and the objectives of the study were explained to obtain translation permission. Then, the forward-only translation method was used to translate the assessment tool by 2 multilingual translators. They were proficient in English, but their native language was Persian. They had no prior knowledge or familiarity with the assessment tool. One of the translators was responsible for translating the forms from English to Persian, while the other translator reviewed and approved the translation. After confirming the forward translation, 10 nursing experts with master and PhD degrees identified and eliminated incomprehensible, inappropriate, non-specialized components of the assessment tool. Finally, to ensure the standardization of the tool, the translations were combined, and a single version that included 20 items was created. The items used in the Persian version were not significantly different from the original one, and no change occurred in any item. The face validity of the assessment tool was assessed and confirmed by the target group. Next, the validity of 20 items was examined by 10 nursing professors, and the content validity index (CVI) and content validity ratio (CVR) were found to be equal to 0.6-1. The checklist was also completed by 21 nurses before and after the intervention to determine its reliability and internal stability. Eventually, the Cronbach α coefficient was found to be equal to 0.80, confirming the checklist reliability. Demographic variables include age, gender, educational degree, ward, and shift time. This assessment tool included 20 items that were assessed using a 5-point Likert scale from 1 (complete disagreement) to 5 (complete agreement).
The I-PASS program was taught to nurses based on 5 principles. The first principle is “illness severity”; in this principle, the nurse must be aware of the severity of the patient's illness and inform the next nurse. Under this principle, there are 3 situations: (i) The client's condition is relatively good and recovering, (ii) the client's condition is relatively bad and needs more care, and (iii) the client's condition is bad and in an emergency situation. The second principle is “patient summary”; in this principle, the nurse is informed about the patient's illness and things such as the reason for admission, initial symptoms, patient information, changes in the diagnosis and treatment plan, initial weight and changes in the patient's weight, etc. The third principle is “action list”; in this principle, the nurse understands the tasks that have to do in his/her shift, and in addition to planning and scheduling, program priorities should be taken into consideration. The responsibility of the next shift nurse should be fully stated, and the list of tasks performed should be specified. In addition, the nurse must be aware of the documentation of the heart and respiratory conditions and necessary instructions for the care of the patient (such as diet) and perform the necessary actions during his/her shift. The fourth principle is “situation awareness and contingency planning”; in this principle, the nurse must be aware of important events, such as the patient’s dangerous diseases (such as AIDS, hepatitis, etc). The fifth principle is “synthesis by receiver,” which includes giving the next nurse the opportunity to ask questions and summarize the contents expressed by the nurse from the previous shift.
The pretest was performed among 47 nurses. Before implementing the program, all participants in both ICU and CCU wards completed the Persian version of the I-PASS Handoff Assessment Tool through self-report. They were provided with comprehensive explanations regarding the objectives, work process, and confidentiality policy. All nurses voluntarily participated in this research. They received shift-handover training based on the I-PASS program for 4 weeks. Training courses were organized with the support of ward supervisors and held once a week for 4 weeks. Each session lasted for 45 minutes, providing participants with the necessary instruction and guidance on the I-PASS program. Due to the COVID-19 pandemic, the valid and reliable instrument items for assessing I-PASS were remotely explained to the participants by the researcher using Adobe Connect software. In addition, during the program implementation, nurses were asked to use the Persian version of I-PASS assessment tool during their shift work in CCU and ICU wards. After 4 weeks, in the posttest, forms were again completed by all nurses, and the data were collected for final analysis. In other words, the SBAR method, which is one of the most common methods, was routinely used. Before implementing the I-PASS program, the pretest data were collected, and I-PASS scores were evaluated to measure the participants' familiarity with this program. Then, the I-PASS program was implemented for 4 weeks, and after the end of this period, the posttest data were collected and compared with the pretest data (CONSORT [Consolidated Standards of Reporting Trials] diagram) (Figure 1).
Data analysis
Data analysis was performed using SPSS version 25 (SPSS Inc, Chicago, IL, USA) and mean and SD to determine demographical factors and variable frequencies. The chi-square test and independent t test were also used for the assessment of significance and correlation between before and after training scores. In addition, the paired t test was used to compare the mean score of nursing shift handover before and after training in each ward. P values less than 0.05 were considered statistically significant.
Results
In this study, 89.4% of participants (42 nurses) were female, and 68.1% (32 nurses) worked in the ICU ward. The mean age of nurses was 33.25 ± 5.00 years, and the mean year of their work experience was 8.08 ± 5.27 years. There were no significant differences between sex, age, and work experiences with the mean scores of nursing shift handover (P > 0.05).
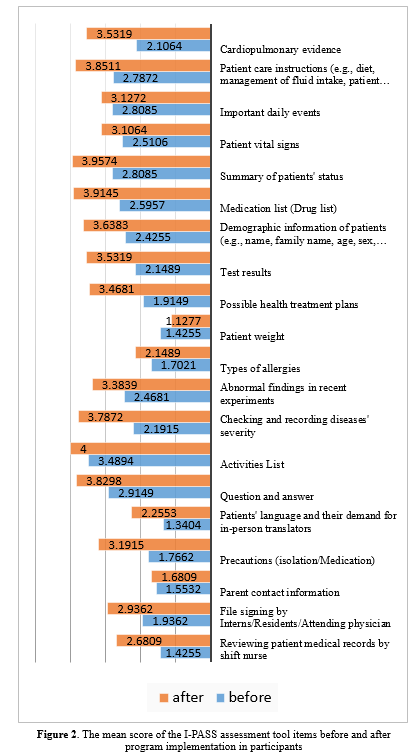
There was a significant difference between the mean scores of nursing shift handover before and after the program implementation in the CCU ward from 1.88 ± 0.32 to 3.62 ± 0.98 (P = 0.018) and in the ICU ward from 2.37 ± 0.84 to 2.93 ± 0.35 (P = 0.013). Also, the mean score of the CCU was higher than that of the ICU (P = 0.01) after the program implementation. The scores of the I-PASS program were measured before and after the implementation (Tables 1 and 2).
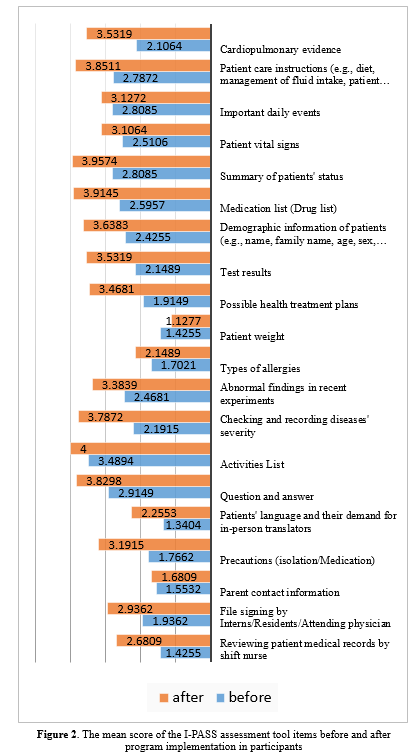
Figure 2 illustrates the data for assessment tool items before and after training for both the CCU and ICU wards. There was a significant difference between the mean scores of nursing shift handover before and after training in both the CCU and ICU wards (2.21 ± 0.75 and 3.15 ± 0.69).
Discussion
The results indicated no significant associations between demographic variables and the mean scores of nursing shift handover after training. In explaining this result, it can be assumed that the I-PASS program is a novel technique globally, and it has not been researched and practiced in Iran so far. Therefore, nurses and health care providers need more practice to perform this program; in addition, promoting its application requires special educational measures and time spent on training. The results showed a significant correlation between ward and the mean scores of nursing shift handover after training; thus, the mean score of nursing shift handover was higher in the CCU than in the ICU. According to Starmer et al, although nursing schedules and baseline handover practices are familiar, the generalizability of the findings to other wards, other provider types, or other types of handover communication remains uncertain (4). In this regard, Shahian explained that adopting/implementing the I-PASS handover system was significantly lower in surgical wards than in pediatric wards (5). The latter study stated that this issue might be due to the heavy workload and special circumstances of the ICU, which prevented nurses from paying adequate attention to the training and proper application of the I-PASS program. Also, the difference in nurses' work experience can be another reason for this finding. It may be that experienced nurses prefer to use the usual method and are resistant to adopting the new I-PASS method, while new nurses are more compatible with the implementation of the new method (6). Due to the lack of similar studies, there was no possibility to discuss further and compare our findings. Further studies with larger sample sizes and longer follow-ups are needed to obtain more accurate outcomes and investigate these variables (7-10).
The statistical findings showed an increase in the effectiveness of intra-ward training of this system, and nursing shift handover improved in each ward after training. These results are consistent with the results obtained by Rosenbluth (8). This indicates the effectiveness of this approach in improving communication skills during nursing shift handover and transferring relevant information of patients to the next health care provider and confirms the effectiveness of the training method in the use of the I-PASS program by nurses. Therefore, it is suggested that relevant managers and officials could order the necessary planning for promoting and training this model. In the present study, there was a statistically significant difference between the overall mean scores of the ICU and CCU before and after training, which is consistent with the results obtained by Starmer et al (2017) and Starmer (2014) (4, 11). This similarity indicates that the training of caregivers has been successful and effective.
In general, nurses' lack of adherence and adequate attention to I-PASS principles can be considered the most important factors in achieving these results. In this regard, more emphasis should be placed on practice and cultural change to enhance adherence and complete understanding of its benefits. Another reason for the above results could be associated with the practice of the I-PASS principles by nurses in specific situations instead of permanent conditions (12-15). This means that nurses may tailor their use of the I-PASS program to specific circumstances and provide high-quality handovers without strict adherence to the mnemonic (15). Also, different units and differences in patient care needs, as well as the care provided by nurses, can affect the performance of the I-PASS program. Therefore, there is a need to adapt the main structure of the I-PASS tool to the care needs of the units. For instance, the summary of the patient's status can significantly differ between gynecology and oncology units (5). Furthermore, some of them argued that using this method required significant workflow changes, which were unacceptable for nurses. However, according to Shahian, this issue was not related to the use of the I-PASS program but reflected the challenges associated with presenting medical services to a large number of patients during limited working times. This is because the I-PASS program, due to its structure, leads to greater efficiency and effectiveness in delivery and transformation (5).
Finally, because the sustainability of the I-PASS program in medical centers requires a cultural change by training in the simplest ways, it is recommended that further studies be conducted on the use, training way, and effects of this method on other items. Also, educating students in colleges and engaging professors and faculty members can lead to profound changes and thus greatly impact adherence to its application.
Conclusion
The results of this study provide a new method for nurses' training in hospitals to improve patients' health and safety. The I-PASS program can solve many challenges during shift changes and nurses’ workflow. Therefore, this method can be a suitable alternative to the common methods of shift handover in hospital wards.
Acknowledgement
The authors would like to express their gratitude to the Research Committee and Vice-Chancellor in Research and Technology Affairs of Bam University of Medical Sciences for their support in conducting this study, as well as to all the nurses who participated in this study at Pasteur Hospital for their valuable support.
Funding sources
This study was supported by the Vice-Chancellor for Research and Technology of Bam University of Medical Sciences (there was no grant).
Ethical statement
This study was approved by the Ethics Committee of Bam University of Medical Sciences (code: IR.MUBAM.REC.1399.012). Verbal and written consent was obtained from all participants.
Conflicts of interest
There is no conflict of interest regarding the publication of this article.
Author contributions
Study concept and design: A.O.; Analysis and interpretation of the data: M. R and T.M.S; Drafting of the manuscript: A.O. and Sh.A.; Critical revision of the manuscript for important intellectual content: A.O, T.M.S. and M.R.; Statistical analysis: M.R.
In this study, 89.4% of participants (42 nurses) were female, and 68.1% (32 nurses) worked in the ICU ward. The mean age of nurses was 33.25 ± 5.00 years, and the mean year of their work experience was 8.08 ± 5.27 years. There were no significant differences between sex, age, and work experiences with the mean scores of nursing shift handover (P > 0.05).
There was a significant difference between the mean scores of nursing shift handover before and after the program implementation in the CCU ward from 1.88 ± 0.32 to 3.62 ± 0.98 (P = 0.018) and in the ICU ward from 2.37 ± 0.84 to 2.93 ± 0.35 (P = 0.013). Also, the mean score of the CCU was higher than that of the ICU (P = 0.01) after the program implementation. The scores of the I-PASS program were measured before and after the implementation (Tables 1 and 2).
Table 1. The test of the I-PASS program correlation in the CCU and ICU wards |
Table 2. Comparison of the I-PASS program mean scores before and after training in both wards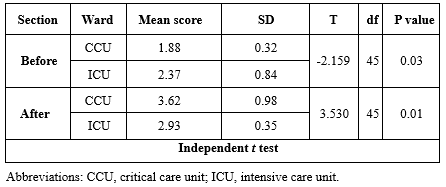 |
Discussion
The results indicated no significant associations between demographic variables and the mean scores of nursing shift handover after training. In explaining this result, it can be assumed that the I-PASS program is a novel technique globally, and it has not been researched and practiced in Iran so far. Therefore, nurses and health care providers need more practice to perform this program; in addition, promoting its application requires special educational measures and time spent on training. The results showed a significant correlation between ward and the mean scores of nursing shift handover after training; thus, the mean score of nursing shift handover was higher in the CCU than in the ICU. According to Starmer et al, although nursing schedules and baseline handover practices are familiar, the generalizability of the findings to other wards, other provider types, or other types of handover communication remains uncertain (4). In this regard, Shahian explained that adopting/implementing the I-PASS handover system was significantly lower in surgical wards than in pediatric wards (5). The latter study stated that this issue might be due to the heavy workload and special circumstances of the ICU, which prevented nurses from paying adequate attention to the training and proper application of the I-PASS program. Also, the difference in nurses' work experience can be another reason for this finding. It may be that experienced nurses prefer to use the usual method and are resistant to adopting the new I-PASS method, while new nurses are more compatible with the implementation of the new method (6). Due to the lack of similar studies, there was no possibility to discuss further and compare our findings. Further studies with larger sample sizes and longer follow-ups are needed to obtain more accurate outcomes and investigate these variables (7-10).
The statistical findings showed an increase in the effectiveness of intra-ward training of this system, and nursing shift handover improved in each ward after training. These results are consistent with the results obtained by Rosenbluth (8). This indicates the effectiveness of this approach in improving communication skills during nursing shift handover and transferring relevant information of patients to the next health care provider and confirms the effectiveness of the training method in the use of the I-PASS program by nurses. Therefore, it is suggested that relevant managers and officials could order the necessary planning for promoting and training this model. In the present study, there was a statistically significant difference between the overall mean scores of the ICU and CCU before and after training, which is consistent with the results obtained by Starmer et al (2017) and Starmer (2014) (4, 11). This similarity indicates that the training of caregivers has been successful and effective.
In general, nurses' lack of adherence and adequate attention to I-PASS principles can be considered the most important factors in achieving these results. In this regard, more emphasis should be placed on practice and cultural change to enhance adherence and complete understanding of its benefits. Another reason for the above results could be associated with the practice of the I-PASS principles by nurses in specific situations instead of permanent conditions (12-15). This means that nurses may tailor their use of the I-PASS program to specific circumstances and provide high-quality handovers without strict adherence to the mnemonic (15). Also, different units and differences in patient care needs, as well as the care provided by nurses, can affect the performance of the I-PASS program. Therefore, there is a need to adapt the main structure of the I-PASS tool to the care needs of the units. For instance, the summary of the patient's status can significantly differ between gynecology and oncology units (5). Furthermore, some of them argued that using this method required significant workflow changes, which were unacceptable for nurses. However, according to Shahian, this issue was not related to the use of the I-PASS program but reflected the challenges associated with presenting medical services to a large number of patients during limited working times. This is because the I-PASS program, due to its structure, leads to greater efficiency and effectiveness in delivery and transformation (5).
Finally, because the sustainability of the I-PASS program in medical centers requires a cultural change by training in the simplest ways, it is recommended that further studies be conducted on the use, training way, and effects of this method on other items. Also, educating students in colleges and engaging professors and faculty members can lead to profound changes and thus greatly impact adherence to its application.
Conclusion
The results of this study provide a new method for nurses' training in hospitals to improve patients' health and safety. The I-PASS program can solve many challenges during shift changes and nurses’ workflow. Therefore, this method can be a suitable alternative to the common methods of shift handover in hospital wards.
Acknowledgement
The authors would like to express their gratitude to the Research Committee and Vice-Chancellor in Research and Technology Affairs of Bam University of Medical Sciences for their support in conducting this study, as well as to all the nurses who participated in this study at Pasteur Hospital for their valuable support.
Funding sources
This study was supported by the Vice-Chancellor for Research and Technology of Bam University of Medical Sciences (there was no grant).
Ethical statement
This study was approved by the Ethics Committee of Bam University of Medical Sciences (code: IR.MUBAM.REC.1399.012). Verbal and written consent was obtained from all participants.
Conflicts of interest
There is no conflict of interest regarding the publication of this article.
Author contributions
Study concept and design: A.O.; Analysis and interpretation of the data: M. R and T.M.S; Drafting of the manuscript: A.O. and Sh.A.; Critical revision of the manuscript for important intellectual content: A.O, T.M.S. and M.R.; Statistical analysis: M.R.
Type of study: Original Article |
Subject:
Nursing
References
1. Starmer AJ, Schnock KO, Lyons A, Hehn RS, Graham DA, Keohane C, et al. Effects of the I-PASS Nursing Handoff Bundle on communication quality and workflow. BMJ Qual Saf. 2017;26(12):949-57. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. O'Rourke J, Abraham J, Riesenberg LA, Matson J, Lopez KD. A Delphi study to identify the core components of nurse to nurse handoff. J Adv Nurs. 2018;74(7):1659-71. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Blazin LJ, Sitthi-Amorn J, Hoffman JM, Burlison JD. Improving patient handoffs and transitions through adaptation and implementation of I-PASS across multiple handoff settings. Pediatr Qual Saf. 2020;5(4):e323. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. Ransom B, Winters K. The I-PASS mnemonic and the occurrence of handoff related errors in adult acute care hospitals: a systematic review protocol. JBI Database System Rev Implement Rep. 2018;16(1):21-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Duong JA, Jensen TP, Morduchowicz S, Mourad M, Harrison JD, Ranji SR. Exploring physician perspectives of residency holdover handoffs: a qualitative study to understand an increasingly important type of handoff. J Gen Intern Med. 2017;32(6):654-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
6. Lescinskas E, Stewart D, Shah C. Improving handoffs: implementing a training program for incoming internal medicine residents. J Grad Med Educ. 2018;10(6):698-701. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Saag HS, Chen J, Denson JL, Jones S, Horwitz L, Cocks PM. Warm handoffs: a novel strategy to improve End-of-Rotation care transitions. J Gen Intern Med. 2018;33(1):116-9. [View at Publisher] [DOI] [PMID] [Google Scholar]
8. Thompson JE, Collett LW, Langbart MJ, Purcell NJ, Boyd SM, Yuminaga Y, et al. Using the ISBAR handover tool in junior medical officer handover: a study in an Australian tertiary hospital. Postgrad Med J. 2011;87(1027):340-4. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Shahian DM, McEachern K, Rossi L, Chisari RG, Mort E. Large-scale implementation of the I-PASS handover system at an academic medical centre. BMJ Qual saf. 2017;26(9):760-70. [View at Publisher] [DOI] [PMID] [Google Scholar]
10. Shahian D. I-PASS handover system: a decade of evidence demands action. BMJ Qual Saf. 2021;30(10):769-74. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Simamora RH, Fathi A. The Influence of Training Handover based SBAR Communication for Improving Patients Safety. Indian J Public Health Res Dev. 2019;10(9):1280-5. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. O'Toole JK, Starmer AJ, Calaman S, Campos M-L, Goldstein J, Hepps J, et al. I-PASS mentored implementation handoff curriculum: implementation guide and resources. MedEdPORTAL: the journal of teaching and learning resources. 2018;14:10736. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Hughes HK, Serwint JR, O'Toole JK, Spector ND, Ngo TL. I-PASS Adherence and Implications for Future Handoff Training. J Grad Med Educ. 2019;11(3):301-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. O'Toole JK, Starmer AJ, Calaman S, Campos M-L, Hepps J, Lopreiato JO, et al. I-PASS Mentored implementation handoff curriculum: champion training materials. MedEdPORTAL. 2019;15:10794. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. O'Toole JK, Hepps J, Starmer AJ, Patel SJ, Rosenbluth G, Calaman S, et al. I-PASS Mentored implementation handoff curriculum: frontline provider training materials. MedEdPORTAL. 2020;16:10912. [View at Publisher] [DOI] [PMID] [Google Scholar]
16. Abadi NE, Rahimzadeh M, Omidi A, Farahani F, Malekyan L, Jalayer F. The relationship between moral courage and quality of work life among nursing staff in Bam hospitals. J Adv Pharm Educ Res. 2020;10(S1). [View at Publisher] [Google Scholar]
17. Rosenbluth G, Destino LA, Starmer AJ, Landrigan CP, Spector ND, Sectish TC, et al. I-PASS handoff program: Use of a campaign to effect transformational change. Pediatr Qual Saf. 2018;3(4):e088. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Jorro Barón F, Pumara CD, Tittarelli MAJ, Raimondo A, Urtasun M, Valentini L. Improved handoff quality and reduction in adverse events following implementation of a Spanish-language version of the I-PASS bundle for pediatric hospitalized patients in Argentina. J Patient Safety and Risk Management. 2020;25(6):225-32. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Tufts LM, Damron CL, Flesher SL. Addition of CORES to the I-PASS handoff: a resident-led quality improvement study. Pediatr Qual Saf. 2020;5(1):e251. [View at Publisher] [DOI] [PMID] [Google Scholar]
20. Starmer AJ, Spector ND, Srivastava R, West DC, Rosenbluth G, Allen AD, et al. Changes in medical errors after implementation of a handoff program. N Engl J Med. 2014;371(19):1803-12. [View at Publisher] [DOI] [PMID] [Google Scholar]
21. Yahyapour Z, Jahanian F, Hosseini Nejad M, Asadi T, Montazer H, Pashaei M. Evaluating I-PASS System Implementation in Improvement of Handoff Process among Emergency Medicine Residents of Mazandaran University of Medical Sciences. Iran J Emerg Med. 2021;8(1):e10. [View at Publisher] [DOI] [Google Scholar]
22. Abdollahi L, Sheini-Jaberi P, Rokhafrooz D. The effect of using SBAR model in shift handover on patient and nurse satisfaction in the emergency department. J Health Admin. 2022;25(1):24-34. [View at Publisher] [DOI] [Google Scholar]
23. Suganandam DK. Handoff communication: Hallmark of nurses. Indian J Continuing Nursing Education. 2018;19(1):12-20. [View at Publisher] [Google Scholar]
24. Clements K. High-reliability and the I-PASS communication tool. Nurs Manage. 2017;48(3):12-3. [View at Publisher] [DOI] [PMID] [Google Scholar]
25. Starmer A, O'Toole J, Spector N, West D, Sectish T, Schnipper J, et al. Mentored implementation of the I-PASS handoff program in diverse clinical environments. BMJ Qual Saf. 2016;25(12):1009. [View at Publisher] [DOI] [Google Scholar]
26. Kulesa JT, Balsara SL, Ghebremariam ET, Colyer J. Designing a Process for Cardiology Patient Transfers: A Quality Improvement, Descriptive Study on Interprovider Communication and Resident Education. Pediatr Qual Saf. 2020;5(3):e300. [View at Publisher] [DOI] [PMID] [Google Scholar]
27. Fitzgerald KM, Banerjee TR, Starmer AJ, Caplan GH, Alkuwari M, Hillier DF, et al. Effect of a Multispecialty Faculty Handoff Initiative on Safety Culture and Handoff Quality. Pediatric quality & safety. 2022;7(2):e539. [View at Publisher] [DOI] [PMID] [Google Scholar]
28. Coffey M, Thomson K, Li S-A, Bismilla Z, Starmer AJ, O'Toole JK, et al. Resident experiences with implementation of the I-PASS handoff bundle. J Grad Med Educ. 2017;9(3):313-20. [View at Publisher] [DOI] [PMID] [Google Scholar]
29. Starmer AJ, Spector ND, West DC, Srivastava R, Sectish TC, Landrigan CP, et al. Integrating research, quality improvement, and medical education for better handoffs and safer care: disseminating, adapting, and implementing the I-PASS program. Jt Comm J Qual Patient Saf. 2017;43(7):319-29. [View at Publisher] [DOI] [PMID] [Google Scholar]
30. Davis R, Davis J, Berg K, Berg D, Morgan CJ, Russo S, et al. Patient handoff education: are medical schools catching up? Am J Med Qual. 2018;33(2):140-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |