Volume 19, Issue 2 (9-2022)
J Res Dev Nurs Midw 2022, 19(2): 63-67 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Ziaei T, Karimi S, Tatari M. Effects of Virtual Emotion Regulation Training on Positive and Negative Sexual Self-Concept of Diabetic Married Women Covered by Comprehensive Health Centers in Gorgan, Iran. J Res Dev Nurs Midw 2022; 19 (2) :63-67
URL: http://nmj.goums.ac.ir/article-1-1310-en.html
URL: http://nmj.goums.ac.ir/article-1-1310-en.html
1- Counselling and Reproductive Health Research Centre, Golestan University of Medical Sciences, Gorgan, Iran , ziaei@goums.ac.ir
2- Golestan University of Medical Sciences(GOUMS), Gorgan, Iran.
2- Golestan University of Medical Sciences(GOUMS), Gorgan, Iran.
Full-Text [PDF 729 kb]
(402 Downloads)
| Abstract (HTML) (1340 Views)
Author contributions
Full-Text: (114 Views)
Introduction
Sexual self-concept refers to the understanding of oneself as a sexual being (1) and recognizing one's sexual aspects (2). It is influenced by cognition, beliefs, and environment (3) and is related to the sexual experiences and behaviors of a person (4). Sexual self-concept is classified into positive, negative, and situational dimensions (5). These dimensions can be affected by various factors including social factors (6), age (7, 8), race (9), chronic diseases, including diabetes (10), infertility (11, 12), disability (13), sexually transmitted diseases (14), vaginismus (15, 16), depression (17), mental health (18), anxiety (17), body image (19), important sexual events, such as starting sexual behaviors in early adolescence (2), history of sexual abuse in childhood (20, 21), and risky sexual behaviors (22). Promoting the positive dimension of sexual self-concept and controlling the negative dimension of sexual self-concept can improve sexual performance in women of reproductive age (23). Sexual self-concept can also predict marital satisfaction and sexual performance of women (24).
Diabetes can result in many complications that influence the psychological and social well-being of the patients (25). It can also disrupt patients' jobs, family relationships, and sexual relations (26). Diabetic women have a weaker positive sexual self-concept, sexual performance, and sexual satisfaction and a stronger negative sexual self-concept (10, 27-30). Due to the financial costs and psychosocial burden of diabetes (31), the main goal of treating these patients is not only to remove the physical symptoms of the disease but also to improve the overall quality of life (32).
Counseling based on the sexual self-concept via smartphones has been able to increase the score of positive self-concept and decrease the score of negative self-concept (33). Moreover, cognitive-behavioral sex training can improve sexual self-concept (34). In this regard, a study reported that the positive sexual self-concept of infertile women would improve one month after emotional regulation training (12). This approach has been used by experts to solve self-concept-related weaknesses, especially sexual self-concept (35).
Emotion regulation skills increase cognitive, behavioral, motivational, and emotional capabilities, and prepare a person to deal with different situations in life (36, 37). The present study was designed to determine the effects of virtual emotion regulation training on the positive and negative sexual self-concepts of diabetic married women.
Methods
This interventional, controlled study with a pretest-posttest design was conducted on women with type 2 diabetes who had been registered in the comprehensive health centers of Gorgan (northeastern Iran) in 2019. Of an overall of 518 people (aged 18 to 50 years), 42 eligible patients were included in the study (Figure 1). Allocation of samples to the intervention and control groups was done through block allocation (AABB-ABAB ABBA-BAAB-BABA-BBAA) and random selection without placing each block corresponding to the permutations of that block (A represents the intervention group and B represents the control group). The random selection of blocks and placement of samples in the intervention and control groups continued according to the location of the block until the desired amount was reached, which was 21 people in each group. The sample size (17 for each group) was calculated at the confidence level of 0.95 according to a study by Ziaei et al. (12), considering the incidence of depression in diabetic women (0.19) (38), 20% dropout rate, and statistical power of 0.99 using the G power software.
Inclusion criteria included having Iranian nationality, high school education and above, living with a spouse in the last 4 weeks, and confirmed diagnosis of type 2 diabetes according to the results of fasting and non-fasting blood sugar and glucose tolerance tests. Exclusion criteria were a history of physical or mental diseases, taking psychiatric medication, having a history of receiving life skills training, obtaining a score of 36-63 from the Beck's Depression Inventory (BDI) at the beginning of the study, and history of infertility, being pregnant, breastfeeding, and menopause.
The data collection tool included a demographic information form, the Persian version of Snell’s Multidimensional Sexual Self-Concept Questionnaire (MSSCQ), and the Persian version of BDI.
The MSSCQ was originally designed by Snell in 1998 (39) and standardized by Ziaei et al. (2012) in Iran (5). The Persian version has 78 questions, 3 dimensions, and 18 sub-dimensions. The positive dimension of sexual self-concept includes 10 areas of sexual self-efficacy, sexual awareness, motivation to avoid risky sexual relations, self-blame in sexual problems, sexual optimism, sexual management, sexual self-esteem, sexual satisfaction, prevention of sexual problems, and internal control of sexual issues. The negative dimension of sexual self-concept includes four areas of sexual anxiety, sexual depression, sexual surveillance, and fear of sexual intercourse. Each field consists of 3 to 5 items. Items belonging to each area are distributed throughout the questionnaire. The answers to the questions are scored on a Likert scale from 0 (does not apply to me at all) to 4 (completely applies to me). Four items are scored in reverse. The minimum score in the positive and negative self-concept dimensions is zero, the maximum score in the positive self-concept is 176, and the maximum negative self-concept score is 64. The reliability of the questionnaire has been reported as 0.89 (5).
The BDI was developed in 1961 by Beck et al. and includes 21 items in the form of sequential phrases, each phrase corresponding to a specific symptom of depression (40). The subjects should choose the sentence that expresses their current state the most. Quantitative values of each item range from 0 to 30 in a way that 0 is mental health in the desired item, 1 is mild disorder, 2 is moderate disorder, and 3 is severe disorder. Only one sentence in each item has the highest score and is therefore considered in the calculations. The sum of scores ranges from 0 to 63 and a negative score is not considered. An overall score of 1-18, 19-28, 29-35, and 36-63 indicates normal mental health, mild depression, moderate depression, and severe depression, respectively. This questionnaire was standardized in Iran by Hojjat et al. (2014) with an alpha coefficient of 0.85 (41).
A written informed consent form was obtained from all subjects before participation. The questionnaires were completed three times: at baseline, immediately after the last training session, and one month after the last training session.
The training was held by an MSc student in midwifery counseling and under the supervision of professors in reproductive health and Counseling (Table 1). The four training sessions were held once a week. The content and structure of each session were based on the principles of group cognitive therapy and skills workshop training (42). At the end of the study period, the training file was given to the members of the control group.
Data were analyzed using SPSS16 and descriptive statistics including mean, standard deviation (SD), as well as frequency and percentage. Repeated measures analysis of variance, Bonferroni's post hoc test, and the chi-square test was also used for data analysis. The normality of quantitative variables and the dimensions of sexual self-concept were assessed using the Shapiro-Wilk test. All analyzes were carried out at a significance level of 0.05.
.JPG)
Results
The average age of the participants in the intervention and control groups was 58.1 ± 4.53 and 55.41 ± 4.99 years, respectively. The average duration of diabetes treatment in both groups was 6 years. Most of the subjects were homemakers and not receiving insulin. Demographic variables did not differ significantly between the two groups (Table 2).
There was no statistically significant difference in the mean scores of depression between the two groups at all test intervals (Table 3).
.JPG)
.JPG)
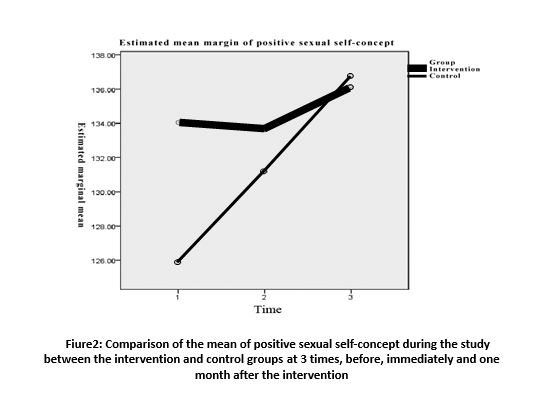
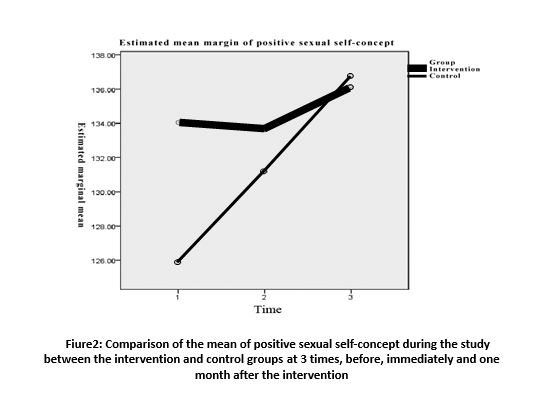
The time-group interaction effect on the positive sexual self-concept was not statistically significant. At baseline, the mean score of positive sexual self-concept in the control group was lower than in the intervention group; however, after the intervention, it increased in the control group and decreased in the intervention group. One month after the intervention, the mean score of positive sexual self-concept increased in both groups (Figure 2).
There was a significant time-group interaction effect on the negative sexual self-concept (P=0.023), but the effect of group was not statistically significant (Table 4).In the negative sexual self-concept, the effect of time was significant (P=0.035), meaning that changes in the mean score of negative sexual self-concept in at least one of the intervention or control groups were significant over time. The changes within the intervention group over time were significant at baseline and after the intervention. The mean score of the negative sexual self-concept at baseline was higher in the intervention group than in the control group; however, it decreased immediately after the intervention and remained unchanged in the control group. One month after the intervention, the mean score of the negative sexual self-concept decreased in the control group and increased in the intervention group (Figure 3).
.JPG)

Participants in the experimental group and 56.70% of the participants in the control group were men. In addition, 83.3% of the participants in the experimental group and 80% of those in the control group were married. Result of the Chi-square test and t-test showed no significant difference in the variables of age, gender, marital status, level of education, occupation, history of smoking, and underlying diseases between the study groups (P>0.05) (Table 1).
Results of the independent t-test showed a significant difference in self-efficacy scores between the study groups at time of discharge (P=0.29). In addition, there was a significant difference in self-efficacy scores two weeks (P=0.01) and four weeks (P=0.001) after discharge from the hospital. According to the results of the repeated-measures ANOVA, the self-efficacy score in the experimental group increased significantly over time. Furthermore, group and time had significant effects on the self-efficacy score (P<0.05) (Table 2).
Discussion
The present study was conducted to determine the effects of virtual emotion regulation training on the positive and negative sexual self-concept of diabetic women. In the intervention group, the mean score of negative sexual self-concept in diabetic women decreased significantly after the intervention. However, the mean score of positive sexual self-concept after the intervention did not differ significantly between the study groups. Yazdani et al. (2018) found that sex therapy along with routine infertility counseling via smartphones reduces the negative self-concept of infertile women immediately and one month after the intervention. In this study, the positive sexual self-concept of infertile women increased immediately and one month after the intervention. In a study by Ziaei et al. (2017), counseling on sexual self-concept reduced the negative sexual self-concept and strengthened sexual performance in women of reproductive age. It also increased the positive sexual self-concept in women of reproductive age (23). In a study by Ghorbanshiroudi, cognitive-behavioral therapy caused a significant reduction in negative sexual self-concept and a significant increase in the positive sexual self-concept of married women immediately after the intervention (43). In another study, cognitive-behavioral sex therapy was effective in improving women's sexual self-concept and decreasing the mean score of negative sexual self-concept (34).
In the study by Ziaei et al., the negative sexual self-concept did not change immediately after the intervention but decreased after one month. In addition, the positive sexual self-concept decreased immediately after the intervention and increased after the one-month follow-up, indicating the interaction effect of time (12).
The result of the present study about the effect of emotion regulation training on the positive sexual self-concept was not consistent with the results of other studies. However, since the main goal of our study i.e. reduction of the negative sexual self-concept was achieved, the positive self-concept might require a longer time to change. Nevertheless, it should be noted that holding virtual group meetings rather than face-to-face interventions could have a significant impact on the outcome of the intervention (44, 45).
The limitations of this study were holding classes virtually due to the coronavirus disease pandemic, difficulty in installing Skype on the subjects’ mobile phones, and Internet connection interruptions during the trainings.
Conclusion
Since reducing the negative dimension of sexual self-concept is one of the important aspects of promoting women's sexual health, especially in those suffering from chronic diseases, emotion regulation training could be a beneficial approach for reducing negative emotions, particularly in diabetic women. It is recommended to compare the outcomes of virtual and face-to-face approaches to determine the most effective method for reducing the negative dimension of sexual self-concept.
Acknowledgement
This article has been derived from a master's degree thesis on midwifery counseling. The authors would like to thank all participants as well as the Vice-Chancellor for Research and Technology of Golestan University of Medical Sciences and the Faculty of Nursing and Midwifery for their support and cooperation.
Funding source
The study received financial support from the Golestan University of Medical Sciences, Iran.
Ethical statement
This study was approved by the ethics committee of Golestan University of Medical Sciences (ethics code IR.GOUMS.REC.1399.183). A written informed consent form was obtained from all subjects prior to participation.
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Sexual self-concept refers to the understanding of oneself as a sexual being (1) and recognizing one's sexual aspects (2). It is influenced by cognition, beliefs, and environment (3) and is related to the sexual experiences and behaviors of a person (4). Sexual self-concept is classified into positive, negative, and situational dimensions (5). These dimensions can be affected by various factors including social factors (6), age (7, 8), race (9), chronic diseases, including diabetes (10), infertility (11, 12), disability (13), sexually transmitted diseases (14), vaginismus (15, 16), depression (17), mental health (18), anxiety (17), body image (19), important sexual events, such as starting sexual behaviors in early adolescence (2), history of sexual abuse in childhood (20, 21), and risky sexual behaviors (22). Promoting the positive dimension of sexual self-concept and controlling the negative dimension of sexual self-concept can improve sexual performance in women of reproductive age (23). Sexual self-concept can also predict marital satisfaction and sexual performance of women (24).
Diabetes can result in many complications that influence the psychological and social well-being of the patients (25). It can also disrupt patients' jobs, family relationships, and sexual relations (26). Diabetic women have a weaker positive sexual self-concept, sexual performance, and sexual satisfaction and a stronger negative sexual self-concept (10, 27-30). Due to the financial costs and psychosocial burden of diabetes (31), the main goal of treating these patients is not only to remove the physical symptoms of the disease but also to improve the overall quality of life (32).
Counseling based on the sexual self-concept via smartphones has been able to increase the score of positive self-concept and decrease the score of negative self-concept (33). Moreover, cognitive-behavioral sex training can improve sexual self-concept (34). In this regard, a study reported that the positive sexual self-concept of infertile women would improve one month after emotional regulation training (12). This approach has been used by experts to solve self-concept-related weaknesses, especially sexual self-concept (35).
Emotion regulation skills increase cognitive, behavioral, motivational, and emotional capabilities, and prepare a person to deal with different situations in life (36, 37). The present study was designed to determine the effects of virtual emotion regulation training on the positive and negative sexual self-concepts of diabetic married women.
Methods
This interventional, controlled study with a pretest-posttest design was conducted on women with type 2 diabetes who had been registered in the comprehensive health centers of Gorgan (northeastern Iran) in 2019. Of an overall of 518 people (aged 18 to 50 years), 42 eligible patients were included in the study (Figure 1). Allocation of samples to the intervention and control groups was done through block allocation (AABB-ABAB ABBA-BAAB-BABA-BBAA) and random selection without placing each block corresponding to the permutations of that block (A represents the intervention group and B represents the control group). The random selection of blocks and placement of samples in the intervention and control groups continued according to the location of the block until the desired amount was reached, which was 21 people in each group. The sample size (17 for each group) was calculated at the confidence level of 0.95 according to a study by Ziaei et al. (12), considering the incidence of depression in diabetic women (0.19) (38), 20% dropout rate, and statistical power of 0.99 using the G power software.
Inclusion criteria included having Iranian nationality, high school education and above, living with a spouse in the last 4 weeks, and confirmed diagnosis of type 2 diabetes according to the results of fasting and non-fasting blood sugar and glucose tolerance tests. Exclusion criteria were a history of physical or mental diseases, taking psychiatric medication, having a history of receiving life skills training, obtaining a score of 36-63 from the Beck's Depression Inventory (BDI) at the beginning of the study, and history of infertility, being pregnant, breastfeeding, and menopause.
The data collection tool included a demographic information form, the Persian version of Snell’s Multidimensional Sexual Self-Concept Questionnaire (MSSCQ), and the Persian version of BDI.
The MSSCQ was originally designed by Snell in 1998 (39) and standardized by Ziaei et al. (2012) in Iran (5). The Persian version has 78 questions, 3 dimensions, and 18 sub-dimensions. The positive dimension of sexual self-concept includes 10 areas of sexual self-efficacy, sexual awareness, motivation to avoid risky sexual relations, self-blame in sexual problems, sexual optimism, sexual management, sexual self-esteem, sexual satisfaction, prevention of sexual problems, and internal control of sexual issues. The negative dimension of sexual self-concept includes four areas of sexual anxiety, sexual depression, sexual surveillance, and fear of sexual intercourse. Each field consists of 3 to 5 items. Items belonging to each area are distributed throughout the questionnaire. The answers to the questions are scored on a Likert scale from 0 (does not apply to me at all) to 4 (completely applies to me). Four items are scored in reverse. The minimum score in the positive and negative self-concept dimensions is zero, the maximum score in the positive self-concept is 176, and the maximum negative self-concept score is 64. The reliability of the questionnaire has been reported as 0.89 (5).
The BDI was developed in 1961 by Beck et al. and includes 21 items in the form of sequential phrases, each phrase corresponding to a specific symptom of depression (40). The subjects should choose the sentence that expresses their current state the most. Quantitative values of each item range from 0 to 30 in a way that 0 is mental health in the desired item, 1 is mild disorder, 2 is moderate disorder, and 3 is severe disorder. Only one sentence in each item has the highest score and is therefore considered in the calculations. The sum of scores ranges from 0 to 63 and a negative score is not considered. An overall score of 1-18, 19-28, 29-35, and 36-63 indicates normal mental health, mild depression, moderate depression, and severe depression, respectively. This questionnaire was standardized in Iran by Hojjat et al. (2014) with an alpha coefficient of 0.85 (41).
A written informed consent form was obtained from all subjects before participation. The questionnaires were completed three times: at baseline, immediately after the last training session, and one month after the last training session.
The training was held by an MSc student in midwifery counseling and under the supervision of professors in reproductive health and Counseling (Table 1). The four training sessions were held once a week. The content and structure of each session were based on the principles of group cognitive therapy and skills workshop training (42). At the end of the study period, the training file was given to the members of the control group.
Data were analyzed using SPSS16 and descriptive statistics including mean, standard deviation (SD), as well as frequency and percentage. Repeated measures analysis of variance, Bonferroni's post hoc test, and the chi-square test was also used for data analysis. The normality of quantitative variables and the dimensions of sexual self-concept were assessed using the Shapiro-Wilk test. All analyzes were carried out at a significance level of 0.05.
.JPG)
Results
The average age of the participants in the intervention and control groups was 58.1 ± 4.53 and 55.41 ± 4.99 years, respectively. The average duration of diabetes treatment in both groups was 6 years. Most of the subjects were homemakers and not receiving insulin. Demographic variables did not differ significantly between the two groups (Table 2).
There was no statistically significant difference in the mean scores of depression between the two groups at all test intervals (Table 3).
.JPG)
.JPG)
The time-group interaction effect on the positive sexual self-concept was not statistically significant. At baseline, the mean score of positive sexual self-concept in the control group was lower than in the intervention group; however, after the intervention, it increased in the control group and decreased in the intervention group. One month after the intervention, the mean score of positive sexual self-concept increased in both groups (Figure 2).
There was a significant time-group interaction effect on the negative sexual self-concept (P=0.023), but the effect of group was not statistically significant (Table 4).In the negative sexual self-concept, the effect of time was significant (P=0.035), meaning that changes in the mean score of negative sexual self-concept in at least one of the intervention or control groups were significant over time. The changes within the intervention group over time were significant at baseline and after the intervention. The mean score of the negative sexual self-concept at baseline was higher in the intervention group than in the control group; however, it decreased immediately after the intervention and remained unchanged in the control group. One month after the intervention, the mean score of the negative sexual self-concept decreased in the control group and increased in the intervention group (Figure 3).
.JPG)

Participants in the experimental group and 56.70% of the participants in the control group were men. In addition, 83.3% of the participants in the experimental group and 80% of those in the control group were married. Result of the Chi-square test and t-test showed no significant difference in the variables of age, gender, marital status, level of education, occupation, history of smoking, and underlying diseases between the study groups (P>0.05) (Table 1).
Results of the independent t-test showed a significant difference in self-efficacy scores between the study groups at time of discharge (P=0.29). In addition, there was a significant difference in self-efficacy scores two weeks (P=0.01) and four weeks (P=0.001) after discharge from the hospital. According to the results of the repeated-measures ANOVA, the self-efficacy score in the experimental group increased significantly over time. Furthermore, group and time had significant effects on the self-efficacy score (P<0.05) (Table 2).
Discussion
The present study was conducted to determine the effects of virtual emotion regulation training on the positive and negative sexual self-concept of diabetic women. In the intervention group, the mean score of negative sexual self-concept in diabetic women decreased significantly after the intervention. However, the mean score of positive sexual self-concept after the intervention did not differ significantly between the study groups. Yazdani et al. (2018) found that sex therapy along with routine infertility counseling via smartphones reduces the negative self-concept of infertile women immediately and one month after the intervention. In this study, the positive sexual self-concept of infertile women increased immediately and one month after the intervention. In a study by Ziaei et al. (2017), counseling on sexual self-concept reduced the negative sexual self-concept and strengthened sexual performance in women of reproductive age. It also increased the positive sexual self-concept in women of reproductive age (23). In a study by Ghorbanshiroudi, cognitive-behavioral therapy caused a significant reduction in negative sexual self-concept and a significant increase in the positive sexual self-concept of married women immediately after the intervention (43). In another study, cognitive-behavioral sex therapy was effective in improving women's sexual self-concept and decreasing the mean score of negative sexual self-concept (34).
In the study by Ziaei et al., the negative sexual self-concept did not change immediately after the intervention but decreased after one month. In addition, the positive sexual self-concept decreased immediately after the intervention and increased after the one-month follow-up, indicating the interaction effect of time (12).
The result of the present study about the effect of emotion regulation training on the positive sexual self-concept was not consistent with the results of other studies. However, since the main goal of our study i.e. reduction of the negative sexual self-concept was achieved, the positive self-concept might require a longer time to change. Nevertheless, it should be noted that holding virtual group meetings rather than face-to-face interventions could have a significant impact on the outcome of the intervention (44, 45).
The limitations of this study were holding classes virtually due to the coronavirus disease pandemic, difficulty in installing Skype on the subjects’ mobile phones, and Internet connection interruptions during the trainings.
Conclusion
Since reducing the negative dimension of sexual self-concept is one of the important aspects of promoting women's sexual health, especially in those suffering from chronic diseases, emotion regulation training could be a beneficial approach for reducing negative emotions, particularly in diabetic women. It is recommended to compare the outcomes of virtual and face-to-face approaches to determine the most effective method for reducing the negative dimension of sexual self-concept.
Acknowledgement
This article has been derived from a master's degree thesis on midwifery counseling. The authors would like to thank all participants as well as the Vice-Chancellor for Research and Technology of Golestan University of Medical Sciences and the Faculty of Nursing and Midwifery for their support and cooperation.
Funding source
The study received financial support from the Golestan University of Medical Sciences, Iran.
Ethical statement
This study was approved by the ethics committee of Golestan University of Medical Sciences (ethics code IR.GOUMS.REC.1399.183). A written informed consent form was obtained from all subjects prior to participation.
Conflict of interest
The authors declare that there is no conflict of interest regarding the publication of this article.
Author contributions
TZ and SK presented the initial idea. TZ, SK, and MT gathered and analyzed the data. SK wrote the manuscript. All authors read and approved the final manuscript.
Type of Study: Original Article |
Subject:
Midwifery
References
1. O'Sullivan LF, Meyer-Bahlburg HF, McKeague IW. The development of the sexual self-concept inventory for early adolescent girls. Psychology of Women Quarterly. 2006;30(2):139-49. [View at paplisher] [DOI] [Google Scholar]
2. Hensel DJ, Fortenberry JD, O'Sullivan LF, Orr DP. The developmental association of sexual self-concept with sexual behavior among adolescent women. Journal of adolescence. 2011;34(4):675-84. [View at paplisher] [DOI] [Google Scholar]
3. To Siu-M, Phyllis KW, Cherry HT, Kan Kwok D, D. LC. Sexual compulsivity, sexual self-concept, and cognitive outcomes of sexual behavior of young Chinese Hong Kong males with compulsive sexual behavior: Implications for intervention and prevention. Child Youth Serv Rev. 2019;104. [View at paplisher] [DOI] [Google Scholar]
4. Rostosky SS, Dekhtyar O, Cupp PK, Anderman EM. Sexual self-concept and sexual self-efficacy in adolescents: a possible clue to promoting sexual health? Journal of sex research. 2008;45(3):277-86. [View at paplisher] [DOI] [Google Scholar]
5. Ziaei T, Khoei EM, Salehi M, Farajzadegan Z. Psychometric properties of the farsi version of modified multidimensional sexual self-concept questionnaire. Iran J Nurs Midwifery Res. 2013;18(6):439. [View at paplisher] [Google Scholar]
6. Potki R, Ziaei T, Faramarzi M, Moosazadeh M, Shahhosseini Z. Bio-psycho-social factors affecting sexual self-concept: A systematic review. Electronic physician. 2017;9(9):5172. [View at paplisher] [DOI] [Google Scholar]
7. Hensel DJ, Fortenberry JD, O'Sullivan LF, Orr DP. The developmental association of sexual self-concept with sexual behavior among adolescent women. J Adolesc. 2011;34(4):675-84. [View at paplisher] [DOI] [Google Scholar]
8. Deutsch AR, Hoffman L, Wilcox BL. Sexual self-concept: testing a hypothetical model for men and women. J Sex Res. 2014;51(8):932-45. [View at paplisher] [DOI] [Google Scholar]
9. Holmes MC. Mental health and sexual self-concept discrepancies in a sample of young black women. J Black Psychol. 2002;28(4):347-70. [View at paplisher] [DOI] [Google Scholar]
10. Ziaei T, Mansourian F, Khoori E, Tatari M. Comparison of sexual self-concept in married diabetic and non-diabetic women referred to Gorgan healthcare centers: An analytical cross-sectional study. Journal of Research Development in Nursing & Midwifery. 2020;17:0-. [View at paplisher] [Google Scholar]
11. Lotfollahi H, Riazi H, Omani-Samani R, Maroufizadeh S, Montazeri A. Sexual self-concept in fertile and infertile women: a comparative study. Int J Fertile Steril. 2021;15(1):60. [View at paplisher] [Google Scholar]
12. Ziaei T, Gordani N, Behnampour N, Naghinasab Ardehaei F, Gharajeh S. The effect of mood regulation education on general and sexual self-concept of infertile women. J Res Dev Nurs Midw. 2020;17:0-. [View at paplisher] [Google Scholar]
13. Salehi M, Tavakol HK, Shabani M, Ziaei T. The relationship between self-esteem and sexual self-concept in people with physical-motor disabilities. Iran Red Crescent Med J. 2015;17(1):25359. [View at paplisher] [DOI] [Google Scholar]
14. Tiet Q, Guadagno R, S. G. Turn down the silence:disclosing genital herpes status to modereate the relationship between stigma and sexual self-concept.: Alliant international university.; 2021. [View at paplisher] [Google Scholar]
15. Reissing ED, Binik YM, Khalif S, Cohen D, Amsel R. Etiological correlates of vaginismus: sexual and physical abuse, sexual knowledge, sexual self-schema, and relationship adjustment. J Sex Marital Ther. 2003;29(1):47-59. [View at paplisher] [DOI] [Google Scholar]
16. Dikmen SNT, Safak Y. Effect of early maladaptive schemas and sexual self-schemas in vaginismus. Int J Med Rev Case Rep. 2020;4(11):15-21. [View at paplisher] [DOI] [Google Scholar]
17. Heidari M, Ghodusi M, Rafiei H. Sexual self-concept and its relationship to depression, stress and anxiety in postmenopausal women. J Menopausal Med. 2017;23(1):42. [View at paplisher] [DOI] [Google Scholar]
18. Peitl MV, Peitl V, Pavlović E. Sexual self-perception in schizophrenic and depressive patients. Nord J Psychiatry. 2011;65(5):306-10. [View at paplisher] [DOI] [Google Scholar]
19. Hannier S, Baltus A, P. DS. The role of physical satisfaction in women's sexual self-esteem. J Sexol. 2017;09(011):1-11. [View at paplisher] [Google Scholar]
20. Rellini AH, Meston CM. Sexual self-schemas, sexual dysfunction, and the sexual responses of women with a history of childhood sexual abuse. Arch Sex Behav. 2011;40(2):351-62. [View at paplisher] [DOI] [Google Scholar]
21. Guyon R, Fernet M, Canivet C, Tardif M, Godbout N. Sexual self-concept among men and women child sexual abuse survivors: emergence of differentiated profiles. Child Abuse Negl. 2020;104(481):104481. [View at paplisher] [DOI] [Google Scholar]
22. Zarea S, Ahi Q, Vaziri S, Shahabizadeh F. Sexual schemas and high-risk sexual behaviors in female students: the mediating role of cognitive emotion regulation. Int Arch Health Sci. 2020;7(4):203. [View at paplisher] [DOI] [Google Scholar]
23. Ziaei T, Farahmand Rad H, Rezaei Aval M, Roshandel G. The relationship between sexual self-concept and sexual function in women of reproductive age referred to health centers in Gorgan, north east of Iran. JMRH. 2017;5(3):969-77. [View at paplisher] [Google Scholar]
24. Potki R, Ziaei T, Moosazadeh M, Faramarzi M, Shahhosseini Z. Predictive role of sexual self-concept in marital satisfaction and sexual function in reproductive-aged women. JMRH. 2020;8(3):2334-41. [View at paplisher] [Google Scholar]
25. Khodabakhshi Koolaee A, Falsafinejad M, A. N. Evaluation of effectiveness of resilience training on psychological well-being of patients with type 2 diabetes. Diabetes Nurse. 2016;4(3):30-40.[Persian]. [View at paplisher] [Google Scholar]
26. Jahanlou SHA, Sobhani A, N. A. A comparison of two standard quality of life questionnaires for evaluation of the relationship between personality characteristics and glycemic control in diabetic patients. AMUJ. 2010;13(2):28-34.[Persian]. [View at paplisher] [Google Scholar]
27. Gandhi J, Dagur G, Warren K, Smith N, Khan SA. The role of sexual dysfunction and infertility on reproductive health in diabetics: pathogenesis, evaluation, and management. Curr Diabetes Rev. 2017;13(0):1-9. [View at paplisher] [DOI] [Google Scholar]
28. Afshari P, Yazdizadeh S, Abedi P, Rashidi H. The relation of diabetes type 2 with sexual function among reproductive age women in iran, a case-control study. Adv Med. 2017;20(17):1-5. [View at paplisher] [DOI] [Google Scholar]
29. Samadi N, Safavi M, Mahmoodi J. Impact of quality of life education on self-concept among type 2 diabetes patients. J Diabetes Metab. 2011;2(5):1-5. [View at paplisher] [DOI] [Google Scholar]
30. Barbagallo F, Mongioì LM, Cannarella R, La Vignera S, Condorelli RA, Calogero AE. Sexual dysfunction in diabetic women: an update on current knowledge. Diabetology. 2020;1(1):11-21. [View at paplisher] [DOI] [Google Scholar]
31. Tol A, Pourreza A, Tavasoli E, A. RF. Determination on knowledge and health literacy among women with type 2 diabetes in teaching hospitals of TUMS. Journal of Hospital. 2012;11(3):45-52.[Persian]. [View at paplisher] [Google Scholar]
32. Tavakkoli L, A. D. Compare the quality of life in type 2 diabetic patients with healthy individuals. . ZJRMS. 2017;19(2). [View at paplisher] [DOI] [Google Scholar]
33. Yazdani M, Mahmoodi Z, Azin SA, Qorbani M. The effect of counseling based on sexual self-concept via social networks on smartphone in infertile women: a randomized controlled trial. Int J Community Based Nurs Midwifery. 2019;7(3):231. [View at paplisher] [Google Scholar]
34. Vahidvaghef M. Study the effectiveness of cognitive-behavioral sex training in improving women's sexual self-concept in Tehran, Iran. Tehran: Universitat Autònoma de Barcelona; 2015. [View at paplisher] [Google Scholar]
35. Afroz G, Ghasemzadeh S, Taziki T, Delgoshad A. Effectiveness of mood regulation skills training on self concept and social competence of students with learning disabilities. J Learn Disabil. 2014;3(3):6-24. [View at paplisher] [Google Scholar]
36. Shepherd-McMullen C, Mearns J, Stokes JE, Mechanic MB. Negative mood regulation expectancies moderate the relationship between psychological abuse and avoidant coping. J Interpers Violence. 2015;30(9):1553-66. [View at paplisher] [DOI] [Google Scholar]
37. Ziaei T, Farahmand Rad H, Roshandel Gh, M. A. Effect of counseling based of sexual self-concept on the sexual health of women in reproductive age. JGJORM. 2018;3(5):85-90. [View at paplisher] [Google Scholar]
38. Naeem A, Shuaib M, Abid MH, Imran M. Prevalence of depression among type2 diabetes mellitus in Pakistani population. Prof Med J. 2019;26(06):919-23. [View at paplisher] [DOI] [Google Scholar]
39. Snell WE. The multidimensional sexual self-concept questionnaire. Handbook of sexuality-related measures. 1998:521-4. [View at paplisher] [Google Scholar]
40. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4(6):561-71. [View at paplisher] [DOI] [Google Scholar]
41. Hojat M, Shapurian R, Mehryar AH. Psychometric properties of a persian version of the short form of the beck depression inventory for iranian college students. Psychol Rep. 1986;59(1):331-8. [View at paplisher] [DOI] [Google Scholar]
42. Fati L, Mootabi F, Mohamad khani SH, M. KzA. Collection of life skills. 1, editor. Tehran: Miankooshk; 2016.
43. Ghorbanshiroudi S,Azari N,Khalatbari J. Studying the effectiveness of cognitive-behavioral therapy in developing sexual self-concept. Int J Basic Appl Sci. 2012;2(4):3378-81. [View at paplisher] [Google Scholar]
44. Gharagozloo N, Moradhaseli M, Atadokht A. Comparison of the effectiveness of face-to-face and virtual cognitive-behavioral couple therapy on post-traumatic stress disorder in extramarital relationships. JCD. 2018;17(65):186-206[Persian]. [View at paplisher] [Google Scholar]
45. Paxton SJ, McLean SA, Gollings EK, Faulkner C, Wertheim EH. Comparison of face‐to‐face and internet interventions for body image and eating problems in adult women:an RCT. Int J Eat Disord. 2007;40:692-704. [View at paplisher] [DOI] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





