Volume 19, Issue 1 (1-2022)
J Res Dev Nurs Midw 2022, 19(1): 34-38 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Afshar A, Pashaeypoor S, Hghani S, Sarkhani N, Nikpeyma N. Relationship between Adherence to Treatment and Self-Efficacy in the Elderly with Arthritis. J Res Dev Nurs Midw 2022; 19 (1) :34-38
URL: http://nmj.goums.ac.ir/article-1-1301-en.html
URL: http://nmj.goums.ac.ir/article-1-1301-en.html
1- Department of Community Health and Geriatric Nursing, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
2- Nursing Care Research Center, Iran University of Medical Science, Tehran, Iran
3- Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
4- Department of Community Health and Geriatric Nursing, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran ,Nikpeyma@yahoo.com
2- Nursing Care Research Center, Iran University of Medical Science, Tehran, Iran
3- Nursing and Midwifery Care Research Center, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran
4- Department of Community Health and Geriatric Nursing, School of Nursing and Midwifery, Tehran University of Medical Sciences, Tehran, Iran ,
Full-Text [PDF 779 kb]
(1190 Downloads)
| Abstract (HTML) (2795 Views)
Full-Text: (471 Views)
Highlights:
What is current knowledge?
According to the existing literature, no study has examined the relationship between adherence to treatment and self-efficacy in the elderly with arthritis, as one of the most common diseases of elderly people.
What is new here?
This study shows there is a direct relationship between treatment adherence and self-efficacy. It is necessary to identify the predictive and effective factors accordingly. It is also necessary to improve the level of treatment adherence and self-efficacy by health planners.
Introduction
Aging may result in a decrease in the volume and number of muscle fibers, muscle weakness, change in connective tissue, and a decrease in flexibility of the joints. In the elderly, these changes can subsequently result in development of joint diseases, such as arthritis (1). Arthritis refers to more than a hundred types of diseases including osteoarthritis in the elderly (2), rheumatoid arthritis, gout, and infectious arthritis (3). As one of the most common diseases of the elderly, arthritis accounts for 31% of the total number of diseases (4). According to reports, 22.7% of the adult population in the United States was diagnosed with arthritis between 2013 and 2015, half of which were older people (5). The overall prevalence of osteoarthritis in Iran is reported to be 17.3% and more common among women (6). Complications of arthritis include chronic pain, ankylosis, impaired physical mobility, fatigue, impaired self-image, and low self-esteem (7).
Treatment adherence is an important aspect of arthritis management (8). This includes adherence to health recommendations (9), medication, diet, and activity plans (10). Disregarding treatment adherence may increase disease severity and lead to disability, which increases the need for immediate treatment and hospitalization (8). Poor adherence to treatment recommendations in the elderly might be due to various physical and mental disorders, including vision and hearing problems, cognitive impairment, several chronic diseases, and complex treatment procedures. This may ultimately lead to symptom exacerbation, disease progression, increased mortality rate, and higher costs (9, 11, 12). Moreover, it has been argued that poor adherence to treatment can reduce efficiency of exercise programs in older people with osteoarthritis (13).
Treatment adherence may be associated with a variety of individual, economic, and social factors (14). Self-efficacy is considered as one of the individual factors that may be directly related to treatment adherence in the elderly (15). It refers to people’s ability to perform expected functions and involves reassuring of one’s ability to optimally perform self-care. Self-efficacy creates motivation, which can play an effective role in building a sense of psychological, social, and individual well-being (16). The elderly are more likely to develop chronic physical and psychological illness and dependency on others for daily activities, which subsequently results in reduced self-efficacy among these individuals (17). In the elderly with rheumatoid arthritis, as the severity of the disease increases, self-efficacy in controlling pain, performing daily activities, and controlling other symptoms decreases (18). Maly et al. reported that increasing self-efficacy in the elderly with osteoarthritis can improve their ability to walk (19). Moreover, self-efficacy is an important component of behavior change in the elderly (20).
Given the importance of treatment adherence and self-efficacy in patients with chronic diseases, this study was designed to determine the relationship between treatment adherence and self-efficacy in the elderly with arthritis. We believe that the results of this study could enable nurses to plan for improving treatment adherence and self-efficacy in the elderly with arthritis.
Methods
This descriptive-correlational study was conducted in 2019 in Tehran, Iran. The research population included the elderly with arthritis who were referred to the clinics of hospitals affiliated with the Tehran University of Medical Sciences. The sample size was calculated by considering 95% confidence level and 80% test power, assuming that a minimum correlation coefficient of 0.2 is sought between adherence to treatment and self-efficacy to have a statistically significant relationship between the two variables. Two hundred eligible patients were recruited from three clinics of Baharloo Hospital (n=70), Ziaian Hospital (n=65), and Shariati Hospital (n=65) through convenience sampling method. Inclusion criteria were being a patient over the age of 60 years, confirmed diagnosis of arthritis, lack of psychiatric disorders, and ability to read and write.
Data were collected using a demographic information form, Modanloo adherence to treatment questionnaire (MATQ) and the perceived self-efficacy scale. The demographic information questionnaire recorded age, sex, level of education, occupational status, marital status, income level, insurance, the reason for referral, living status, type of residential house, access to elevator, history of chronic diseases, history of taking medication, duration of illness, ability to perform personal duties, ability to do household chores, and ability to work outside. The MATQ questionnaire was developed to investigate treatment adherence in patients with chronic diseases (21). The questionnaire includes 40 items with seven subscales; making effort for treatment (nine items), intention to take the treatment (seven items), adaptability (seven items), integrating illness into life (five items), adherence to treatment (four items), commitment to treatment (five items), and indecisiveness for applying treatment (three items). The responses are scored based on a six-point Likert scale (from “not at all = 0” to “completely agree = 5”). A total MATQ score of 0–200 can be obtained. The overall scores of 75-100, 50-74, 26-29, and 0-25 indicate very good, good, moderate, and poor adherence to treatment, respectively. The validity and reliability of the questionnaire were measured by the developers, and a Cronbach’s alpha coefficient of 0.92 was obtained for the scale (21). The perceived self-efficacy scale was developed by Lorig et al. (1989) in the United States (22) and consists of 20 items and three subscales; pain (five items), functioning (nine items), and other symptoms (six items). Each item is scored based on a 10-point Likert scale, and a higher overall score indicates higher self-efficacy. The reliability of the original scale was confirmed by obtaining a Cronbach’s alpha coefficient of 0.9. After obtaining permission from the developers of the scale, the original scale was translated using the standard open translation method, and the content validity was assessed qualitatively based on the opinions of a panel of experts. The reliability of the instrument, in this study, was confirmed by obtaining Cronbach’s alpha coefficients of 0.806 and 0.941 for the subscales of pain and functioning and other symptoms, respectively. A total Cronbach’s alpha coefficient of 0.963 was obtained for the scale. After conducting the test-retest reliability measure, the correlation coefficients of 0.905 and 0.922 were obtained for the subscales of pain and functioning and other symptoms, respectively. A total coefficient of 0.953 was obtained for the whole scale.
The study received approval from the ethics committee of Tehran University of Medical Sciences, Tehran, Iran (ethical code: IR.TUMS.FNM.REC.1397.205). Participation in the study was voluntary. Written informed consent was obtained from all participants. The questionnaires were completed in the clinics after explaining the study objectives. Data were summarized using descriptive statistics (frequency, mean, and standard deviation) and analyzed using inferential statistics (the Pearson correlation coefficient) in SPSS software (version 16). The statistical significance level was set at 0.05.
Results
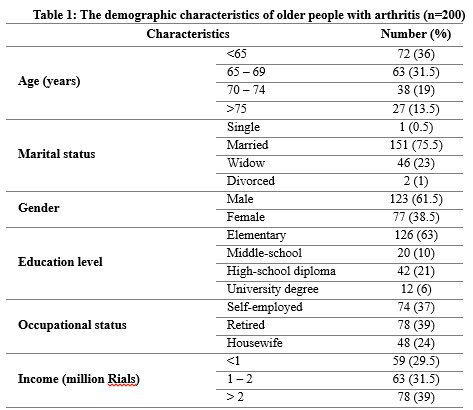
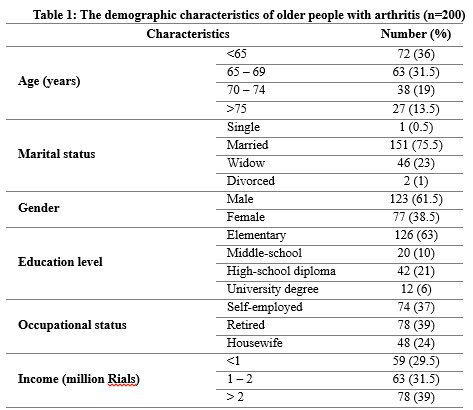
The mean age of the patients was 67.97±5.32 years. The majority of the participants were male (61.5%), married (75.5%), and with elementary education (63%) (Table 1).
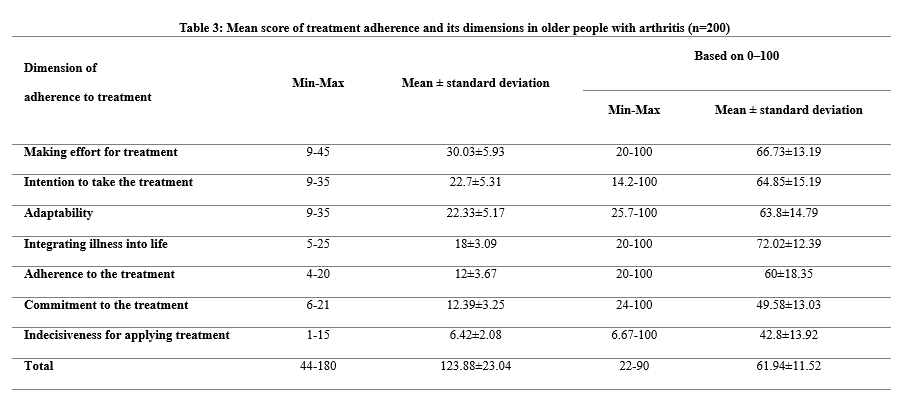
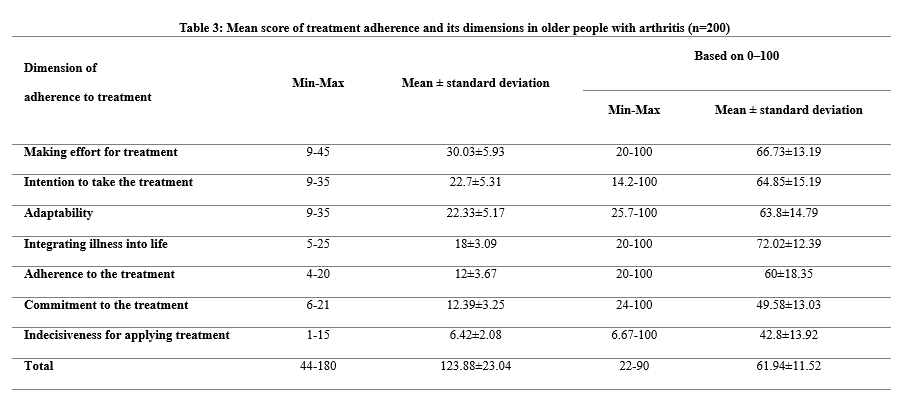
According to the results, 71.5% of the participants had good treatment adherence (Table 2). The mean score of adherence to treatment was 123.88±32.04, which was equal to 61.94±11.52 based on 0-100. Moreover, the highest mean score of adherence to treatment was observed in the subscale of integrating illness into life (72.02±12.39), and the lowest mean score was observed in the subscale of indecisiveness for applying treatment (42.8±13.92) (Table 3).
The mean total score for self-efficacy was 119.8±35.3, which was equal to 6.3±1.85 based on 1-10, indicating a moderate level of self-efficacy among the subjects (Table 2). In addition, the highest mean score of self-efficacy was observed in the subscale of functioning (6.77±2), and the lowest mean score was observed in the subscale of pain (5.36±1.91) (Table 4).
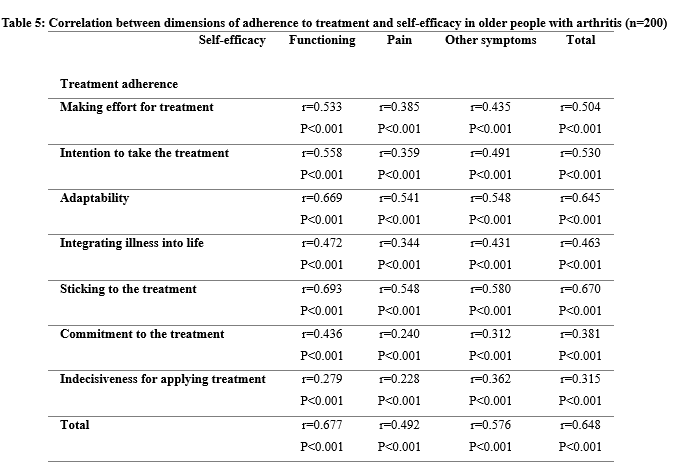
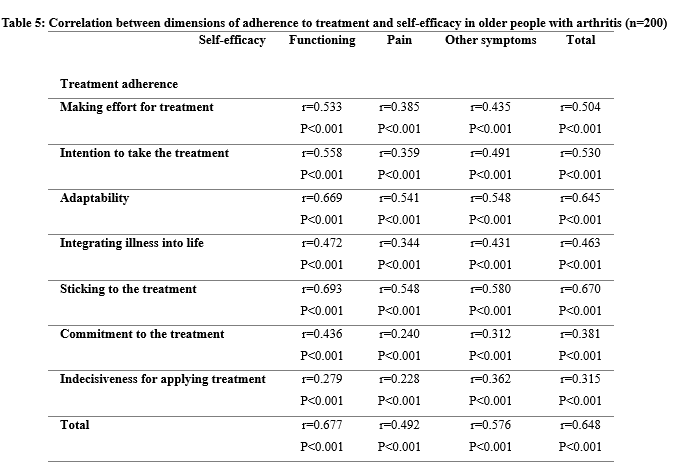
The results of the Pearson correlation coefficient showed a direct correlation between self-efficacy scores and treatment adherence scores and their subscales (Table 5). The strongest direct correlation for self-efficacy was observed in the subscale of functioning and adherence to treatment (r=0.693), while the weakest direct correlation was observed in the subscale of pain and indecisiveness for applying treatment (r=0.228).
Discussion
Based on the results, more than half of the elderly with arthritis had a good level of adherence to treatment. This is consistent with some local and international studies in terms of treatment adherence in chronic patients (8, 10). In a previous study in Iran, 80% of hypertensive patients showed relatively optimum adherence to treatment (10). In another study in Iran, there was a moderate to good level of medication adherence among patients with rheumatoid arthritis (8). On the other hand, some studies reported a low level of adherence to treatment among patients with chronic diseases (23-25). Adherence to treatment can reduce treatment costs and risk of complications, which ultimately results in improvement of patients' physical and mental well-being. Therefore, good adherence to treatment in the elderly can help to control the complications of the disease and empower them to care for themselves (9).
In our study, there was a moderate level of self-efficacy among the elderly with arthritis. Torki et al. also found that the general self-efficacy in the elderly living in rest homes was moderate (25). Similarly, Narimani and Samadifard also reported moderate self-efficacy among the elderly (26). Meanwhile, in China, Gong and Mao reported low self-efficacy among young adults with rheumatoid arthritis (27).
We found a significant and direct correlation between self-efficacy and adherence to treatment among the elderly with arthritis. Self-efficacy is considered an important factor in changing health-related behaviors. Such changes are facilitated by individuals’ sense of control. In other words, if people believe that they can do something to solve problems, they will feel more committed to doing it (15). Our findings in this regard are generally consistent with the results of previous studies in Iran and other countries. Vangeli et al. reported a strong relationship between social-psychological factors, such as self-efficacy, and lack of adherence to treatment among patients with inflammatory diseases (28). Nafradi et al. believed that empowering individuals and improving their self-efficacy can promote adherence to treatment (29). Moreover, Andini et al. found that adherence to treatment was poor in patients with low self-efficacy (30). Shao et al. found a significant correlation between adherence to treatment and self-efficacy in patients with type 2 diabetes (31). In a study by Daniali et al., there was a weak correlation between self-efficacy and adherence to treatment among patients with chronic disease (32). McCulley et al. reported a negative relationship between self-efficacy and treatment adherence in adults with rheumatoid arthritis (33). In fact, when there is no proper self-efficacy, it is less likely to adhere to health care behaviors.
Our study population was limited to the elderly in Tehran; therefore, it is necessary to be cautious when generalizing the results of the present study to other communities. Also, due to the limited number of local researchers in this field, it was difficult to comprehensively compare the findings. It is recommended to consider the cognitive, individual, and social differences of the elderly in future studies.
Conclusion
Based on the findings of the present study, adherence to treatment and self-efficacy are relatively desirable among the elderly with arthritis in Tehran, Iran. Moreover, there is a direct relationship between treatment adherence and self-efficacy. Given the importance of adherence to treatment and self-efficacy in chronic diseases, it is necessary to identify the predictive and effective factors accordingly. It is also necessary to improve the level of treatment adherence and self-efficacy by health planners, especially nurses.
Acknowledgements
This article has been derived from results of a master's thesis on geriatric nursing, conducted at the faculty of Nursing and Midwifery, Tehran University of Medical Sciences. The researchers are truly thankful to all individuals who participated in this study.
What is current knowledge?
According to the existing literature, no study has examined the relationship between adherence to treatment and self-efficacy in the elderly with arthritis, as one of the most common diseases of elderly people.
What is new here?
This study shows there is a direct relationship between treatment adherence and self-efficacy. It is necessary to identify the predictive and effective factors accordingly. It is also necessary to improve the level of treatment adherence and self-efficacy by health planners.
Introduction
Aging may result in a decrease in the volume and number of muscle fibers, muscle weakness, change in connective tissue, and a decrease in flexibility of the joints. In the elderly, these changes can subsequently result in development of joint diseases, such as arthritis (1). Arthritis refers to more than a hundred types of diseases including osteoarthritis in the elderly (2), rheumatoid arthritis, gout, and infectious arthritis (3). As one of the most common diseases of the elderly, arthritis accounts for 31% of the total number of diseases (4). According to reports, 22.7% of the adult population in the United States was diagnosed with arthritis between 2013 and 2015, half of which were older people (5). The overall prevalence of osteoarthritis in Iran is reported to be 17.3% and more common among women (6). Complications of arthritis include chronic pain, ankylosis, impaired physical mobility, fatigue, impaired self-image, and low self-esteem (7).
Treatment adherence is an important aspect of arthritis management (8). This includes adherence to health recommendations (9), medication, diet, and activity plans (10). Disregarding treatment adherence may increase disease severity and lead to disability, which increases the need for immediate treatment and hospitalization (8). Poor adherence to treatment recommendations in the elderly might be due to various physical and mental disorders, including vision and hearing problems, cognitive impairment, several chronic diseases, and complex treatment procedures. This may ultimately lead to symptom exacerbation, disease progression, increased mortality rate, and higher costs (9, 11, 12). Moreover, it has been argued that poor adherence to treatment can reduce efficiency of exercise programs in older people with osteoarthritis (13).
Treatment adherence may be associated with a variety of individual, economic, and social factors (14). Self-efficacy is considered as one of the individual factors that may be directly related to treatment adherence in the elderly (15). It refers to people’s ability to perform expected functions and involves reassuring of one’s ability to optimally perform self-care. Self-efficacy creates motivation, which can play an effective role in building a sense of psychological, social, and individual well-being (16). The elderly are more likely to develop chronic physical and psychological illness and dependency on others for daily activities, which subsequently results in reduced self-efficacy among these individuals (17). In the elderly with rheumatoid arthritis, as the severity of the disease increases, self-efficacy in controlling pain, performing daily activities, and controlling other symptoms decreases (18). Maly et al. reported that increasing self-efficacy in the elderly with osteoarthritis can improve their ability to walk (19). Moreover, self-efficacy is an important component of behavior change in the elderly (20).
Given the importance of treatment adherence and self-efficacy in patients with chronic diseases, this study was designed to determine the relationship between treatment adherence and self-efficacy in the elderly with arthritis. We believe that the results of this study could enable nurses to plan for improving treatment adherence and self-efficacy in the elderly with arthritis.
Methods
This descriptive-correlational study was conducted in 2019 in Tehran, Iran. The research population included the elderly with arthritis who were referred to the clinics of hospitals affiliated with the Tehran University of Medical Sciences. The sample size was calculated by considering 95% confidence level and 80% test power, assuming that a minimum correlation coefficient of 0.2 is sought between adherence to treatment and self-efficacy to have a statistically significant relationship between the two variables. Two hundred eligible patients were recruited from three clinics of Baharloo Hospital (n=70), Ziaian Hospital (n=65), and Shariati Hospital (n=65) through convenience sampling method. Inclusion criteria were being a patient over the age of 60 years, confirmed diagnosis of arthritis, lack of psychiatric disorders, and ability to read and write.
Data were collected using a demographic information form, Modanloo adherence to treatment questionnaire (MATQ) and the perceived self-efficacy scale. The demographic information questionnaire recorded age, sex, level of education, occupational status, marital status, income level, insurance, the reason for referral, living status, type of residential house, access to elevator, history of chronic diseases, history of taking medication, duration of illness, ability to perform personal duties, ability to do household chores, and ability to work outside. The MATQ questionnaire was developed to investigate treatment adherence in patients with chronic diseases (21). The questionnaire includes 40 items with seven subscales; making effort for treatment (nine items), intention to take the treatment (seven items), adaptability (seven items), integrating illness into life (five items), adherence to treatment (four items), commitment to treatment (five items), and indecisiveness for applying treatment (three items). The responses are scored based on a six-point Likert scale (from “not at all = 0” to “completely agree = 5”). A total MATQ score of 0–200 can be obtained. The overall scores of 75-100, 50-74, 26-29, and 0-25 indicate very good, good, moderate, and poor adherence to treatment, respectively. The validity and reliability of the questionnaire were measured by the developers, and a Cronbach’s alpha coefficient of 0.92 was obtained for the scale (21). The perceived self-efficacy scale was developed by Lorig et al. (1989) in the United States (22) and consists of 20 items and three subscales; pain (five items), functioning (nine items), and other symptoms (six items). Each item is scored based on a 10-point Likert scale, and a higher overall score indicates higher self-efficacy. The reliability of the original scale was confirmed by obtaining a Cronbach’s alpha coefficient of 0.9. After obtaining permission from the developers of the scale, the original scale was translated using the standard open translation method, and the content validity was assessed qualitatively based on the opinions of a panel of experts. The reliability of the instrument, in this study, was confirmed by obtaining Cronbach’s alpha coefficients of 0.806 and 0.941 for the subscales of pain and functioning and other symptoms, respectively. A total Cronbach’s alpha coefficient of 0.963 was obtained for the scale. After conducting the test-retest reliability measure, the correlation coefficients of 0.905 and 0.922 were obtained for the subscales of pain and functioning and other symptoms, respectively. A total coefficient of 0.953 was obtained for the whole scale.
The study received approval from the ethics committee of Tehran University of Medical Sciences, Tehran, Iran (ethical code: IR.TUMS.FNM.REC.1397.205). Participation in the study was voluntary. Written informed consent was obtained from all participants. The questionnaires were completed in the clinics after explaining the study objectives. Data were summarized using descriptive statistics (frequency, mean, and standard deviation) and analyzed using inferential statistics (the Pearson correlation coefficient) in SPSS software (version 16). The statistical significance level was set at 0.05.
Results
The mean age of the patients was 67.97±5.32 years. The majority of the participants were male (61.5%), married (75.5%), and with elementary education (63%) (Table 1).
According to the results, 71.5% of the participants had good treatment adherence (Table 2). The mean score of adherence to treatment was 123.88±32.04, which was equal to 61.94±11.52 based on 0-100. Moreover, the highest mean score of adherence to treatment was observed in the subscale of integrating illness into life (72.02±12.39), and the lowest mean score was observed in the subscale of indecisiveness for applying treatment (42.8±13.92) (Table 3).
The mean total score for self-efficacy was 119.8±35.3, which was equal to 6.3±1.85 based on 1-10, indicating a moderate level of self-efficacy among the subjects (Table 2). In addition, the highest mean score of self-efficacy was observed in the subscale of functioning (6.77±2), and the lowest mean score was observed in the subscale of pain (5.36±1.91) (Table 4).
The results of the Pearson correlation coefficient showed a direct correlation between self-efficacy scores and treatment adherence scores and their subscales (Table 5). The strongest direct correlation for self-efficacy was observed in the subscale of functioning and adherence to treatment (r=0.693), while the weakest direct correlation was observed in the subscale of pain and indecisiveness for applying treatment (r=0.228).
Discussion
Based on the results, more than half of the elderly with arthritis had a good level of adherence to treatment. This is consistent with some local and international studies in terms of treatment adherence in chronic patients (8, 10). In a previous study in Iran, 80% of hypertensive patients showed relatively optimum adherence to treatment (10). In another study in Iran, there was a moderate to good level of medication adherence among patients with rheumatoid arthritis (8). On the other hand, some studies reported a low level of adherence to treatment among patients with chronic diseases (23-25). Adherence to treatment can reduce treatment costs and risk of complications, which ultimately results in improvement of patients' physical and mental well-being. Therefore, good adherence to treatment in the elderly can help to control the complications of the disease and empower them to care for themselves (9).
In our study, there was a moderate level of self-efficacy among the elderly with arthritis. Torki et al. also found that the general self-efficacy in the elderly living in rest homes was moderate (25). Similarly, Narimani and Samadifard also reported moderate self-efficacy among the elderly (26). Meanwhile, in China, Gong and Mao reported low self-efficacy among young adults with rheumatoid arthritis (27).
We found a significant and direct correlation between self-efficacy and adherence to treatment among the elderly with arthritis. Self-efficacy is considered an important factor in changing health-related behaviors. Such changes are facilitated by individuals’ sense of control. In other words, if people believe that they can do something to solve problems, they will feel more committed to doing it (15). Our findings in this regard are generally consistent with the results of previous studies in Iran and other countries. Vangeli et al. reported a strong relationship between social-psychological factors, such as self-efficacy, and lack of adherence to treatment among patients with inflammatory diseases (28). Nafradi et al. believed that empowering individuals and improving their self-efficacy can promote adherence to treatment (29). Moreover, Andini et al. found that adherence to treatment was poor in patients with low self-efficacy (30). Shao et al. found a significant correlation between adherence to treatment and self-efficacy in patients with type 2 diabetes (31). In a study by Daniali et al., there was a weak correlation between self-efficacy and adherence to treatment among patients with chronic disease (32). McCulley et al. reported a negative relationship between self-efficacy and treatment adherence in adults with rheumatoid arthritis (33). In fact, when there is no proper self-efficacy, it is less likely to adhere to health care behaviors.
Our study population was limited to the elderly in Tehran; therefore, it is necessary to be cautious when generalizing the results of the present study to other communities. Also, due to the limited number of local researchers in this field, it was difficult to comprehensively compare the findings. It is recommended to consider the cognitive, individual, and social differences of the elderly in future studies.
Conclusion
Based on the findings of the present study, adherence to treatment and self-efficacy are relatively desirable among the elderly with arthritis in Tehran, Iran. Moreover, there is a direct relationship between treatment adherence and self-efficacy. Given the importance of adherence to treatment and self-efficacy in chronic diseases, it is necessary to identify the predictive and effective factors accordingly. It is also necessary to improve the level of treatment adherence and self-efficacy by health planners, especially nurses.
Acknowledgements
This article has been derived from results of a master's thesis on geriatric nursing, conducted at the faculty of Nursing and Midwifery, Tehran University of Medical Sciences. The researchers are truly thankful to all individuals who participated in this study.
Funding source
The authors received no financial support for the research, authorship, and/or publication of this article.
Ethical statement
The study received approval from the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran (ethical code: IR.TUMS.FNM.REC.1397.205). Participation in the study was voluntary, and written informed consent was obtained from all participants after explaining the research objectives.
Conflict of interest
The authors declare that there is no conflict of interest regarding publication of this article.
Author contributions
Conceptualization: Methodology, analysis, research a review: Ali Afshar, Nasrin Nikpeyma,Shahzad Pashaeypoor, Shima Haghani, Naeimeh Sarkhani, Writing- review and editing: Ali Afshar, Nasrin Nikpeyma, Shahzad Pashaeypoor, Shima Haghani, Naeimeh Sarkhani.

.PNG)
.PNG)

.PNG)
.PNG)
Type of study: Original Article |
Subject:
Nursing
References
1. Eliopoulos C. Gerontological nursing. Lippincott Williams & Wilkins; 2013. [Google Scholar]
2. CDC. Arthritis [Internet]. Centers for Disease Control and Prevention. 2021 [cited 2022 Jul 5]. Available from:https://www.cdc.gov/chronicdisease/resources/publications/factsheets/arthritis.htm
3. Carpenter D, Hartigan C, Thompkins D. Introduction to National Certification Examinations. Adult-Gerontology Acute Care Nurse Practitioner Q&A Review. 2018 Nov 28:1.5]. Available from:https://escholarship.umassmed.edu/gsn_pp/116/
4. Top 10 Chronic Conditions Affecting Older Adults [Internet]. @NCOAging. [cited 2022 Jul 5]. Available from:https://www.ncoa.org/article/the-top-10-most-common-chronic-conditions-in-older-adults
5. Barbour KE, Helmick CG, Boring M, Brady TJ. Vital signs: prevalence of doctor-diagnosed arthritis and arthritis-attributable activity limitation-United States, 2013-2015. MMWR. 2017; 66(9):246. [View at paplisher] [DOI] [PMID] [Google Scholar]
6. Jazayeri MD, Qoreishi MD, Hoseinzadeh S, Reza H, Babanejad MS, Jazayeri MD, et all. Investigation of the Asporin Gene Polymorphism as a Risk Factor for Knee Osteoarthritis in Iran. IJOS. 2015; 13(1):30-5. [Persian] [View at paplisher] [Google Scholar]
7. Feldthusen C, Björk M, Forsblad-d'Elia H, Mannerkorpi K. Perception, consequences, communication, and strategies for handling fatigue in persons with rheumatoid arthritis of working age-a focus group study. Clinical rheumatology. 2013; 32(5):557-66. [View at paplisher] [DOI] [PMID] [Google Scholar]
8. Salehi Z, Norouzi Tabrizi K, Hoseini MA, Sedghi Goyaghaj N, Soltani PR. The study of the correlation between medication adherence and quality of life of Rheumatoid Arthritis patients. JCNM. 2017; 4(3): 1-13. [Persian] [View at paplisher] [Google Scholar]
9. Scheiman-Elazary A, Duan L, Shourt C, Agrawal H, Ellashof D, Cameron-Hay M, Furst DE. The rate of adherence to antiarthritis medications and associated factors among patients with rheumatoid arthritis: a systematic literature review and metaanalysis. The Journal of rheumatology. 2016; 43(3):512-23. [View at paplisher] [DOI] [PMID] [Google Scholar]
10. Masror Roudsari DD, Dabiri Golchin M, Haghani H. Relationship between adherence to therapeutic regimen and health related quality of life in hypertensive patients. IJN. 2013; 26(85):44-54. [Persian] [View at paplisher] [Google Scholar]
11. Patton DE, Hughes CM, Cadogan CA, Ryan CA. Theory-based interventions to improve medication adherence in older adults prescribed polypharmacy: a systematic review. Drugs & aging. 2017; 34(2):97-113. [View at paplisher] [DOI] [PMID] [Google Scholar]
12. Garcia-Gonzalez A, Richardson M, Popa-Lisseanu MG, Cox V, Kallen MA, Janssen N, Ng B, Marcus DM, Reveille JD, Suarez-Almazor ME. Treatment adherence in patients with rheumatoid arthritis and systemic lupus erythematosus. Clinical rheumatology. 2008; 27(7):883-9. [View at paplisher] [DOI] [PMID] [Google Scholar]
13. Marks R, Allegrante JP. Chronic osteoarthritis and adherence to exercise: a review of the literature. JAPA. 2005; 13(4):434-60. [View at paplisher] [DOI] [PMID] [Google Scholar]
14. Lee WP, Lee SS, Xin X, Thumboo J. Towards a better understanding of reasons for non-adherence to treatment among patients with rheumatoid arthritis: A focus group study. PSH. 2017; 26(2):109-13. [View at paplisher] [DOI] [Google Scholar]
15. Sedghi Goyaghaj N, Pishgooie AH, Ghorbani S, Basatin M, Azadehjoo N. Correlation between Self-efficacy and Adherence to Therapeutic Regimen in Veterans with Spinal Cord Injury. IJWPH. 2019; 11(1):41-7. [Persian] [View at paplisher] [Google Scholar]
16. Martinez-Calderon J, Zamora-Campos C, Navarro-Ledesma S, Luque-Suarez A. The role of self-efficacy on the prognosis of chronic musculoskeletal pain: a systematic review. The Journal of Pain. 2018; 19(1):10-34. [View at paplisher] [DOI] [PMID] [Google Scholar]
17. Susanto T, Rasny H, Susumaningrum LA, Yunanto RA, Nur KR. Prevalence of hypertension and predictive factors of self-efficacy among elderly people with hypertension in institutional-based rehabilitation in Indonesia. Education. 2019; 21(1), 14-21. [View at paplisher] [DOI] [Google Scholar]
18. Somers TJ, Shelby RA, Keefe FJ, Godiwala N, Lumley MA, Mosley‐Williams A, et al. Disease severity and domain‐specific arthritis self‐efficacy: Relationships to pain and functioning in patients with rheumatoid arthritis. Arthritis care & research. 2010; 62(6):848-56. [View at paplisher] [DOI] [PMID] [Google Scholar]
19. Maly MR, Costigan PA, Olney SJ. Self-efficacy mediates walking performance in older adults with knee osteoarthritis. JG Series A: Biological Sciences and Medical Sciences. 2007; 62(10):1142-6. [View at paplisher] [DOI] [PMID] [Google Scholar]
20. Ory MG, Lee S, Han G, Towne SD, Quinn C, Neher T, et al. Effectiveness of a lifestyle intervention on social support, self-efficacy, and physical activity among older adults: evaluation of texercise select. IJERPH. 2018; 15(2):234. [View at paplisher] [DOI] [PMID] [Google Scholar]
21. Seyed Fatemi N, Rafii F, Hajizadeh E, Modanloo M. Psychometric properties of the adherence questionnaire in patients with chronic disease: A mix method study. Koomesh. 2018; 20(2):179-91. [Persian] [View at paplisher] [Google Scholar]
22. Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self‐efficacy in people with arthritis. Arthritis & Rheumatism: OJACR. 1989; 32(1):37-44. [View at paplisher] [DOI] [PMID] [Google Scholar]
23. Rahmati M, Rejeh N, Heravi Karimooi M, Tadrisi SD. Investigating the relationship between health literacy and adherence with treatment regimen in the elderly with hypertension. IJNR. 2019; 13(5):15-22. [Persian] [View at paplisher] [Google Scholar]
24. Marks R. Knee osteoarthritis and exercise adherence: a review. Current aging science. 2012; 5(1):72-83. [View at paplisher] [DOI] [PMID] [Google Scholar]
25. Torki Y, Hajikazemi E, Bastani F, Haghani H. General Self Efficacy in Elderly Living in Rest-Homes. IJN (2008-5923). 2011; 24(73): 55-62. [Persian] [View at paplisher] [Google Scholar]
26. Narimani M, Samadifard H. Social Health in the elderly: The Role of Self-esteem, Self-efficiency and happiness. Aging Psychology. 2017; 3(3):199-206. [Persian] [View at paplisher] [Google Scholar]
27. Gong G, Mao J. Health-related quality of life among Chinese patients with rheumatoid arthritis: the predictive roles of fatigue, functional disability, self-efficacy, and social support. Nursing research. 2016; 65(1):55-67. [View at paplisher] [DOI] [PMID] [Google Scholar]
28. Vangeli E, Bakhshi S, Baker A, Fisher A, Bucknor D, Mrowietz U, et al. A systematic review of factors associated with non-adherence to treatment for immune-mediated inflammatory diseases. Advances in therapy. 2015; 32(11):983-1028. [View at paplisher] [DOI] [PMID] [Google Scholar]
29. Nafradi L, Nakamoto K, Schulz PJ. Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PloS one. 2017; 12(10):e0186458. [View at paplisher] [DOI] [PMID] [Google Scholar]
30. Andini S, Yona S, Waluyo A. Self-efficacy, depression, and adherence to antiretroviral therapy (ART) among Indonesian women with HIV. Enfermeria clinica. 2019; 29:687-90. [View at paplisher] [DOI] [Google Scholar]
31. Shao Y, Liang L, Shi L, Wan C, Yu S. The effect of social support on glycemic control in patients with type 2 diabetes mellitus: the mediating roles of self-efficacy and adherence. JDR. 2017; 2017. 280417. [View at paplisher] [DOI] [PMID] [Google Scholar]
32. Daniali SS, Darani FM, Eslami AA, Mazaheri M. Relationship between self-efficacy and physical activity, medication adherence in chronic disease patients. ABR. 2017; 6 (36). [View at paplisher] [DOI] [PMID] [Google Scholar]
33. McCulley C, Katz P, Trupin L, Yelin EH, Barton JL. Association of medication beliefs, self-efficacy, and adherence in a diverse cohort of adults with rheumatoid arthritis. The Journal of rheumatology. 2018; 45(12):1636-42. [View at paplisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






