Volume 20, Issue 2 (10-2023)
J Res Dev Nurs Midw 2023, 20(2): 50-53 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Kolagari S, Najafi M, Brojerdi M, Modanloo M. Clinical competency of nurses working at Intensive Care Units and its associated factors. J Res Dev Nurs Midw 2023; 20 (2) :50-53
URL: http://nmj.goums.ac.ir/article-1-1294-en.html
URL: http://nmj.goums.ac.ir/article-1-1294-en.html
1- Nursing Research Center, Golestan University of Medical Sciences, Gorgan, Iran
2- School of Nursing and Midwifery, Golestan University of Medical Sciences, Gorgan, Iran
3- Nursing Research Center, Golestan University of Medical Sciences Gorgan, Iran , Modanloo1@yahoo.com
2- School of Nursing and Midwifery, Golestan University of Medical Sciences, Gorgan, Iran
3- Nursing Research Center, Golestan University of Medical Sciences Gorgan, Iran , Modanloo1@yahoo.com
Full-Text [PDF 404 kb]
(110 Downloads)
| Abstract (HTML) (691 Views)
Full-Text: (44 Views)
Introduction
Rapid changes in the health system demand providing quality and safe nursing care, which has always been a goal of nursing, a process that requires competency (1, 2). As frontline care providers, nurses need to maintain their competency in order to provide professional and clinical duties (1). Competency refers to the ability to recognize and judge behaviors and acquire the skills required for effectively fulfilling duties (3), and nursing competency is to use these skills to promote the professional position of nursing (4). Nursing clinical competency is one of the main indicators in the assessment of nursing performance and a behavior-oriented concept revolving around the clinical and professional duties of nurses (1, 5). The clinical competency of intensive care unit (ICU) nurses has been reported as desirable in some studies and average in others (6). Clinical competency indicates nurses’ ability to deliver effective and safe clinical performance and fulfill professional responsibilities in practice (7). Clinical competency is a key concept in nursing, denoting the judicious application of technical and communication skills, knowledge, clinical reasoning, emotions, and values, and critical thinking in the clinical environment (3). Evaluation of clinical competency can help nurses and managers recognize and become aware of clinical performance in hospital wards and special care units in particular (8). Intensive care units are among the key wards of hospitals hosting patients with critical and acute conditions, such as acute respiratory distress syndrome (ARDS), trauma, multiple organ failure, acute sepsis, shock, and poisoning, who require constant and careful monitoring (9). These units are generally full of high-tech equipment and patients suffering from multi-organ failure who need to receive safe care from competent nurses (10). The professional and moral duties of nurses have expanded substantially in parallel with rapid growth in science, advances in technology, the complexity and diversity of therapeutic methods (11), care levels, patient safety, and the need for providing quality care in wards such as ICUs (12). Researchers believe that delivering standard nursing care demands upgrading competency levels and employing experienced and competent personnel. The lack of clinical competency in ICU nurses can lead to medical errors, rework, patient dissatisfaction, and the waste of time and energy (13, 14). The results of a study by Haj-Bagheri and Eshraghi (2018) showed that there was a direct relationship between the level of clinical competency and the quality of nursing care (7). Also, the findings of Sasaki et al. revealed a direct and significant correlation between clinical competency level and work experience (14). Regarding the importance of the clinical competency of ICU nurses, this study aimed to determine the clinical competency of ICU nurses and its associated factors in hospitals affiliated with the Golestan University of Medical Sciences.
Methods
This descriptive inferential study was conducted on the ICU nurses of 2019. According to a study by Shuryabi et al. (2017), who reported excellent clinical competency in 75% of nurses, this ratio was used as the basis for determining the sample size (6). Considering the type, I error (α) of 5%, the accuracy of 10%, and the dropout probability of 20%, the sample size was calculated using the following formula as n= 128. After taking into account the 20% likelihood of dropout, the final sample size was calculated as n= 160.
n=(Z_(1-α⁄2)^2×P ×(1-P))/d^2
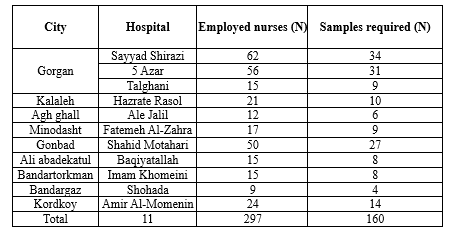
Following a sampling framework, 160 nurses working in the ICUs of the hospitals affiliated with the Golestan University of Medical Sciences in Gorgan, Kalaleh, Aq-qala, Minodasht, Gonbad, Aliabad, Bandar-e-gaz, and Kordkoy cities were recruited by simple random sampling based on stratification and corresponding to the size of each stratum (the number of ICU nurses in each hospital) (Table 1). Simple random sampling of nurses was based on the national code. After preparing a list of nurses working in hospitals affiliated with the Golestan University of Medical Sciences, those whose national codes had an even number on the far-right side were chosen to be included in the study.
Inclusion criteria were willingness to participate in the study, providing informed consent, having at least six months of work experience in ICUs, and not suffering from evident physical or psychological problems. After explaining the objectives of the research and obtaining written informed consent, a demographic information form and the Intensive and Critical Care Nursing Competence Scale (ICCN-CS) were provided to the ICU nurses working in different shifts (i.e., morning, evening, and night) in the teaching hospitals affiliated to the Golestan University of Medical Sciences. It took approximately 10-15 minutes for each nurse to complete the questionnaires. The ICCN-CS is an 80-item questionnaire designed by Nakaya et al. in Finland and translated into Persian and culturally adapted by Shuryabi et al. (2017) in a study supported by the Shahid Beheshti University of Medical Sciences, Iran (6). The reliability of the questionnaire was approved by Cronbach’s alpha coefficient (α) of 0.98. The 80 items of this scale assessed nursing clinical competency in four dimensions, including knowledge (20 items), skills (20 items), attitudes and values (20 items), and experience (20 items). The scoring was based on a Likert scale (1-5), where the scores of the knowledge and skills dimensions were categorized as poor (1 score) to excellent (5 scores). The score of the dimension of attitudes and values was categorized from complete disagreement (1 score) to complete agreement (5 scores), and regarding the experience dimension, the final score was categorized from completely inadequate (1 score) to completely adequate (5 scores). The range of the final clinical competency score was from 80 to 400, which was stratified as poor (80-160), average (161-240), good (241-320), and excellent (321-400) (6).
Rapid changes in the health system demand providing quality and safe nursing care, which has always been a goal of nursing, a process that requires competency (1, 2). As frontline care providers, nurses need to maintain their competency in order to provide professional and clinical duties (1). Competency refers to the ability to recognize and judge behaviors and acquire the skills required for effectively fulfilling duties (3), and nursing competency is to use these skills to promote the professional position of nursing (4). Nursing clinical competency is one of the main indicators in the assessment of nursing performance and a behavior-oriented concept revolving around the clinical and professional duties of nurses (1, 5). The clinical competency of intensive care unit (ICU) nurses has been reported as desirable in some studies and average in others (6). Clinical competency indicates nurses’ ability to deliver effective and safe clinical performance and fulfill professional responsibilities in practice (7). Clinical competency is a key concept in nursing, denoting the judicious application of technical and communication skills, knowledge, clinical reasoning, emotions, and values, and critical thinking in the clinical environment (3). Evaluation of clinical competency can help nurses and managers recognize and become aware of clinical performance in hospital wards and special care units in particular (8). Intensive care units are among the key wards of hospitals hosting patients with critical and acute conditions, such as acute respiratory distress syndrome (ARDS), trauma, multiple organ failure, acute sepsis, shock, and poisoning, who require constant and careful monitoring (9). These units are generally full of high-tech equipment and patients suffering from multi-organ failure who need to receive safe care from competent nurses (10). The professional and moral duties of nurses have expanded substantially in parallel with rapid growth in science, advances in technology, the complexity and diversity of therapeutic methods (11), care levels, patient safety, and the need for providing quality care in wards such as ICUs (12). Researchers believe that delivering standard nursing care demands upgrading competency levels and employing experienced and competent personnel. The lack of clinical competency in ICU nurses can lead to medical errors, rework, patient dissatisfaction, and the waste of time and energy (13, 14). The results of a study by Haj-Bagheri and Eshraghi (2018) showed that there was a direct relationship between the level of clinical competency and the quality of nursing care (7). Also, the findings of Sasaki et al. revealed a direct and significant correlation between clinical competency level and work experience (14). Regarding the importance of the clinical competency of ICU nurses, this study aimed to determine the clinical competency of ICU nurses and its associated factors in hospitals affiliated with the Golestan University of Medical Sciences.
Methods
This descriptive inferential study was conducted on the ICU nurses of 2019. According to a study by Shuryabi et al. (2017), who reported excellent clinical competency in 75% of nurses, this ratio was used as the basis for determining the sample size (6). Considering the type, I error (α) of 5%, the accuracy of 10%, and the dropout probability of 20%, the sample size was calculated using the following formula as n= 128. After taking into account the 20% likelihood of dropout, the final sample size was calculated as n= 160.
n=(Z_(1-α⁄2)^2×P ×(1-P))/d^2
Following a sampling framework, 160 nurses working in the ICUs of the hospitals affiliated with the Golestan University of Medical Sciences in Gorgan, Kalaleh, Aq-qala, Minodasht, Gonbad, Aliabad, Bandar-e-gaz, and Kordkoy cities were recruited by simple random sampling based on stratification and corresponding to the size of each stratum (the number of ICU nurses in each hospital) (Table 1). Simple random sampling of nurses was based on the national code. After preparing a list of nurses working in hospitals affiliated with the Golestan University of Medical Sciences, those whose national codes had an even number on the far-right side were chosen to be included in the study.
Inclusion criteria were willingness to participate in the study, providing informed consent, having at least six months of work experience in ICUs, and not suffering from evident physical or psychological problems. After explaining the objectives of the research and obtaining written informed consent, a demographic information form and the Intensive and Critical Care Nursing Competence Scale (ICCN-CS) were provided to the ICU nurses working in different shifts (i.e., morning, evening, and night) in the teaching hospitals affiliated to the Golestan University of Medical Sciences. It took approximately 10-15 minutes for each nurse to complete the questionnaires. The ICCN-CS is an 80-item questionnaire designed by Nakaya et al. in Finland and translated into Persian and culturally adapted by Shuryabi et al. (2017) in a study supported by the Shahid Beheshti University of Medical Sciences, Iran (6). The reliability of the questionnaire was approved by Cronbach’s alpha coefficient (α) of 0.98. The 80 items of this scale assessed nursing clinical competency in four dimensions, including knowledge (20 items), skills (20 items), attitudes and values (20 items), and experience (20 items). The scoring was based on a Likert scale (1-5), where the scores of the knowledge and skills dimensions were categorized as poor (1 score) to excellent (5 scores). The score of the dimension of attitudes and values was categorized from complete disagreement (1 score) to complete agreement (5 scores), and regarding the experience dimension, the final score was categorized from completely inadequate (1 score) to completely adequate (5 scores). The range of the final clinical competency score was from 80 to 400, which was stratified as poor (80-160), average (161-240), good (241-320), and excellent (321-400) (6).
|
Table 1. Sampling framework for collecting study data
 |
For data analysis, we used SPSS 16 software, descriptive statistics (such as frequency, percentage, mean, and standard deviation), and inferential statistics. As the Kolmogorov-Smirnov test revealed that the data had non-normal distribution, the Kruskal-Wallis (for age, type of contract, work experience, ethnicity, work shift, and overtime) and Mann-Whitney (for marital status, gender, educational status, and job position) tests were used for analysis. The confidence interval was designated as 95%, and the statistical significance level as 0.05.
Results
In this study, out of 160 ICU nurses enrolled, 156 responded to the questionnaires (a response rate of 97.5%). The mean age of responders was 32.02 ± 6.25 years, most of whom were female (75%), married (64.1%), and of Persian ethnicity (75%). Also, most of the nurses had bachelor’s degrees (91.7%), worked on rotating shifts (39.7%), were permanently employed (42.3%), and had work experience of less than 5 years (41.7%). Data analysis showed that the level of overall clinical competency among the ICU nurses assessed was excellent. Regarding individual dimensions, clinical competency was also excellent in the knowledge dimension but poor in the dimension of skills (Table 2).
The highest and lowest mean scores of clinical competencies among ICU nurses belonged to the knowledge and skill dimensions, respectively (Table 3).
Results
In this study, out of 160 ICU nurses enrolled, 156 responded to the questionnaires (a response rate of 97.5%). The mean age of responders was 32.02 ± 6.25 years, most of whom were female (75%), married (64.1%), and of Persian ethnicity (75%). Also, most of the nurses had bachelor’s degrees (91.7%), worked on rotating shifts (39.7%), were permanently employed (42.3%), and had work experience of less than 5 years (41.7%). Data analysis showed that the level of overall clinical competency among the ICU nurses assessed was excellent. Regarding individual dimensions, clinical competency was also excellent in the knowledge dimension but poor in the dimension of skills (Table 2).
|
Table 2. The frequency of clinical competency dimensions' scores of Nurses (n=156)
 |
|
Table 3. Mean score of clinical competencies and its dimensions in ICUs nurses
 |
Regarding demographic variables, the highest mean score of clinical competencies was observed in nurses in the age group of 42-47 years, as well as male, married, and permanently employed nurses, those with 15-20 years of work experience, nurses with Persian ethnicity, those working in rotating shifts, nurses with bachelor's degrees, and those with <30 hours overtime work. However, nursing clinical competency showed a statistically significant relationship only with age, marital status, type of contract, work experience, and overtime hours (P<0.05, Table 4).
|
Table 4. Relationship between clinical competence and demographic characteristics in ICUs nurses
 |
Discussion
The results of the present study showed that most of the ICU nurses enrolled had excellent levels of clinical competency, which was consistent with the observations of Faraji et al. (15) and Elhami et al. (16). On the other hand, the clinical competency score fell in the good category in the studies of Sasaki et al. and Haj-Bagheri et al. and in the average category in the study of Karami et al. The relatively acceptable clinical competency of ICU nurses seems to be related to the deliberate apportion of competent nurses to special care units, continuous evaluation of nurses’ clinical competency by nursing managers, implementing plans to improve clinical competency, and upgrading existing facilities (7, 14, 17). Among the dimensions assessed, our results indicated that nursing clinical competency was at an excellent level in the field of knowledge, but it was observed to be poor in the field of skills, and these dimensions attained the highest and lowest competency scores, respectively. Meanwhile, Hasani et al. reported that the level of clinical competency was high in both the knowledge and skill dimensions (18).
Regarding the association of clinical competency with demographic variables, our findings showed that the mean competency score was higher in the age group of 42-47 years than in other age groups, and there was a statistically significant link between clinical competency and age. This observation agreed with the results of Karami et al., Shuryabi et al., and Haj-Bagheri et al. (6, 17) but opposed the findings of Faraji et al. (16). In the present study, the highest mean score of clinical competencies belonged to male nurses; however, there was no significant relationship between clinical competency and gender. This observation was also consistent with the findings of Sasaki et al. and Mirlashari et al. In the present research, unlike previous studies, we utilized a specialized tool to assess nursing clinical competency, which could reveal more details on this topic, justifying preferences toward relying on male nurses for managing critical clinical situations (14, 19).
We also noticed that married nurses attained a higher mean clinical competency score compared to single nurses. There was also a significant association between clinical competency and marital status, which was consistent with the findings of Karami et al. but inconsistent with the observation of Mirlashari et al. It seems that married nurses have better motivations to fulfill their professional duties and acquire higher competency in the work environment, allowing them to have superior job security than unmarried nurses (17, 19).
Moreover, we observed that permanently employed nurses attained a higher mean clinical competency score than nurses with non-permanent contracts, and there was a significant link between clinical competency and the type of contract. This finding was in line with the report of Shuryabi et al. It is obvious that permanently employed nurses have more incentives to acquire experience and achieve promotion due to their better job security (6).
The mean clinical competency score was also the highest among nurses with a work experience of 15-20 years, and there was a significant relationship between clinical competency and work experience. This was consistent with the observation of Elhami et al. but inconsistent with the report of Faraji et al. It appears that the high clinical competency of nurses with work experience beyond 15 years can reflect the substantial impact of work experience on acquiring clinical competency skills (15, 16).
We here observed no significant relationship between clinical competency and the job position of nurses, which was in agreement with the study of Sasaki et al. (14). Although nurses of Persian ethnicity acquired a higher clinical competency score, no significant association was identified between clinical competency and ethnicity. We found no studies assessing the association of clinical competency with ethnicity or the job position of nurses, so we could not provide comparisons in this regard.
Also, the highest mean clinical competency score was obtained by nurses working in rotating shifts; however, work shift was not significantly associated with clinical competency, which was in line with the findings of Haj-Bagheri et al. and Faraji et al. (7). Taking into account that most nurses experience rotating shifts at the beginning of their careers, one can justify the lack of a significant relationship between the type of work shift and clinical competency.
The highest mean score of clinical competencies was obtained by nurses who hold bachelor’s degrees, but no significant association was noticed between clinical competency and the level of education. This finding was in parallel with the report of Shouryabi et al. (6). It seems that specialized clinical competency skills can be determined by not only their educational levels but also their clinical experience as nurses in wards such as ICUs. Due to advances in science and technology, the level of education alone cannot be adequate for providing quality nursing care, so nurses need to participate in specialized courses and acquaint themselves with novel nursing care methods.
Finally, the highest mean clinical competency score was achieved by nurses who had overtime working below 30 hours, reflecting a significant association between clinical competency and overtime work. This observation agrees with the report of Elhami et al. (15). It seems that prolonged overtime work can exhaust nurses, leading to their burnout and providing low-quality care.
One of the strengths of this study was the assessment of the clinical competency of ICU nurses using a specialized and indigenized tool in Iran. Among the limitations of the present study, one can mention the potential impacts of ICU nurses’ high workload, many items in the questionnaires, and the lack of adequate time to complete the questionnaires on nurses’ responses. Health system planners are recommended to focus on improving the clinical competency of ICU nurses by boosting their clinical skills.
Conclusion
It is of crucial importance for ICU nurses to achieve high clinical competency. Clinical competency assessment can help boost the quality of nursing care during crises and critical conditions. In our study, the overall clinical competency of ICU nurses was observed to be excellent, and this level was also observed in the knowledge dimension; however, the lowest clinical competency belonged to the dimension of skills. In addition, the clinical competency of ICU nurses was significantly associated with age, gender, marital status, work experience, and the type of contract, highlighting the need for paying more attention to these variables to boost the clinical competency of ICU nurses.
Acknowledgement
We would like to express our gratitude to the Deputy of Research and Technology of Golestan University of Medical Sciences for the financial and scientific support for this project. We also thank the nurses participating in this research.
Funding sources
This study was supported by the Golestan University of Medical Sciences.
Ethical statement
The present study was related to a MSc. thesis in the field of critical care nursing approved by the Faculty of Nursing and Midwifery and the Ethics Committee of the Golestan University of Medical Sciences (IR.GOUMS.REC.1398.065). Written informed consent was obtained from the nurses participating in this research.
Conflicts of interest
The authors declare that they have no conflict of interest.
Author contributions
All authors actively participated in the study’s design and implementation, as well as in the preparation of the initial and final drafts of the manuscript. All authors approved the final version of the manuscript.
The results of the present study showed that most of the ICU nurses enrolled had excellent levels of clinical competency, which was consistent with the observations of Faraji et al. (15) and Elhami et al. (16). On the other hand, the clinical competency score fell in the good category in the studies of Sasaki et al. and Haj-Bagheri et al. and in the average category in the study of Karami et al. The relatively acceptable clinical competency of ICU nurses seems to be related to the deliberate apportion of competent nurses to special care units, continuous evaluation of nurses’ clinical competency by nursing managers, implementing plans to improve clinical competency, and upgrading existing facilities (7, 14, 17). Among the dimensions assessed, our results indicated that nursing clinical competency was at an excellent level in the field of knowledge, but it was observed to be poor in the field of skills, and these dimensions attained the highest and lowest competency scores, respectively. Meanwhile, Hasani et al. reported that the level of clinical competency was high in both the knowledge and skill dimensions (18).
Regarding the association of clinical competency with demographic variables, our findings showed that the mean competency score was higher in the age group of 42-47 years than in other age groups, and there was a statistically significant link between clinical competency and age. This observation agreed with the results of Karami et al., Shuryabi et al., and Haj-Bagheri et al. (6, 17) but opposed the findings of Faraji et al. (16). In the present study, the highest mean score of clinical competencies belonged to male nurses; however, there was no significant relationship between clinical competency and gender. This observation was also consistent with the findings of Sasaki et al. and Mirlashari et al. In the present research, unlike previous studies, we utilized a specialized tool to assess nursing clinical competency, which could reveal more details on this topic, justifying preferences toward relying on male nurses for managing critical clinical situations (14, 19).
We also noticed that married nurses attained a higher mean clinical competency score compared to single nurses. There was also a significant association between clinical competency and marital status, which was consistent with the findings of Karami et al. but inconsistent with the observation of Mirlashari et al. It seems that married nurses have better motivations to fulfill their professional duties and acquire higher competency in the work environment, allowing them to have superior job security than unmarried nurses (17, 19).
Moreover, we observed that permanently employed nurses attained a higher mean clinical competency score than nurses with non-permanent contracts, and there was a significant link between clinical competency and the type of contract. This finding was in line with the report of Shuryabi et al. It is obvious that permanently employed nurses have more incentives to acquire experience and achieve promotion due to their better job security (6).
The mean clinical competency score was also the highest among nurses with a work experience of 15-20 years, and there was a significant relationship between clinical competency and work experience. This was consistent with the observation of Elhami et al. but inconsistent with the report of Faraji et al. It appears that the high clinical competency of nurses with work experience beyond 15 years can reflect the substantial impact of work experience on acquiring clinical competency skills (15, 16).
We here observed no significant relationship between clinical competency and the job position of nurses, which was in agreement with the study of Sasaki et al. (14). Although nurses of Persian ethnicity acquired a higher clinical competency score, no significant association was identified between clinical competency and ethnicity. We found no studies assessing the association of clinical competency with ethnicity or the job position of nurses, so we could not provide comparisons in this regard.
Also, the highest mean clinical competency score was obtained by nurses working in rotating shifts; however, work shift was not significantly associated with clinical competency, which was in line with the findings of Haj-Bagheri et al. and Faraji et al. (7). Taking into account that most nurses experience rotating shifts at the beginning of their careers, one can justify the lack of a significant relationship between the type of work shift and clinical competency.
The highest mean score of clinical competencies was obtained by nurses who hold bachelor’s degrees, but no significant association was noticed between clinical competency and the level of education. This finding was in parallel with the report of Shouryabi et al. (6). It seems that specialized clinical competency skills can be determined by not only their educational levels but also their clinical experience as nurses in wards such as ICUs. Due to advances in science and technology, the level of education alone cannot be adequate for providing quality nursing care, so nurses need to participate in specialized courses and acquaint themselves with novel nursing care methods.
Finally, the highest mean clinical competency score was achieved by nurses who had overtime working below 30 hours, reflecting a significant association between clinical competency and overtime work. This observation agrees with the report of Elhami et al. (15). It seems that prolonged overtime work can exhaust nurses, leading to their burnout and providing low-quality care.
One of the strengths of this study was the assessment of the clinical competency of ICU nurses using a specialized and indigenized tool in Iran. Among the limitations of the present study, one can mention the potential impacts of ICU nurses’ high workload, many items in the questionnaires, and the lack of adequate time to complete the questionnaires on nurses’ responses. Health system planners are recommended to focus on improving the clinical competency of ICU nurses by boosting their clinical skills.
Conclusion
It is of crucial importance for ICU nurses to achieve high clinical competency. Clinical competency assessment can help boost the quality of nursing care during crises and critical conditions. In our study, the overall clinical competency of ICU nurses was observed to be excellent, and this level was also observed in the knowledge dimension; however, the lowest clinical competency belonged to the dimension of skills. In addition, the clinical competency of ICU nurses was significantly associated with age, gender, marital status, work experience, and the type of contract, highlighting the need for paying more attention to these variables to boost the clinical competency of ICU nurses.
Acknowledgement
We would like to express our gratitude to the Deputy of Research and Technology of Golestan University of Medical Sciences for the financial and scientific support for this project. We also thank the nurses participating in this research.
Funding sources
This study was supported by the Golestan University of Medical Sciences.
Ethical statement
The present study was related to a MSc. thesis in the field of critical care nursing approved by the Faculty of Nursing and Midwifery and the Ethics Committee of the Golestan University of Medical Sciences (IR.GOUMS.REC.1398.065). Written informed consent was obtained from the nurses participating in this research.
Conflicts of interest
The authors declare that they have no conflict of interest.
Author contributions
All authors actively participated in the study’s design and implementation, as well as in the preparation of the initial and final drafts of the manuscript. All authors approved the final version of the manuscript.
Type of Study: Original Article |
Subject:
Nursing
References
1. Mrayyan MT, Abunab HY, Khait AA, Rababa MJ, Al-Rawashdeh S, Algunmeeyn A, et al. Competency in nursing practice: a concept analysis. BMJ Open. 2023;13(6):e067352. [View at Publisher] [DOI] [PMID] [Google Scholar]
2. Jamal K, Alameri RA, Alqahtani FM, AlGarni RS, Alamri NA, Elshnawie HA, et al. Knowledge and Attitudes of Critical Care Nurses Regarding Pain Management in Saudi Arabia. Med Arch. 2023;77(1):49-55. [View at Publisher] [DOI] [PMID] [Google Scholar]
3. Nabizadeh-Gharghozar Z, Alavi NM, Ajorpaz NM. Clinical competence in nursing: A hybrid concept analysis. Nurse Educ Today. 2021;97:104728. [View at Publisher] [DOI] [PMID] [Google Scholar]
4. DeGrande H, Liu F, Greene P, Stankus J-A. Developing professional competence among critical care nurses: An integrative review of literature. Intensive Crit Care Nurs. 2018;49:65-71. [View at Publisher] [DOI] [PMID] [Google Scholar]
5. Ghorbani S, Heshmati Nabavi F, Heidarian Miri H, Mazlom SR, Akbari Rad SA, Mohebbi T. Evaluation of clinical competence of novice nurses from the perspective of head nurses, a cross-sectional descriptive study in mashhad university of medical sciences in 2019. Quarterly Journal of Nursing Management. 2021;10(1):60-7. [View at Publisher] [Google Scholar]
6. Shouryabi AA, Ghahrisarabi A, Anboohi SZ, Nasiri M, Rassouli M. Psychometric properties of the Persian version of the Intensive and Critical Care Nursing Competence Scale version-1 (ICCN-CS-1). Electron physician. 2017;9(11):5785-92. [View at Publisher] [DOI] [PMID] [Google Scholar]
7. Adib Hajbaghery M, Eshraghi Arani N. Assessing Nurses' Clinical Competence from Their Own Viewpoint and the viewpoint of Head Nurses: A Descriptive Study. Iran Journal of Nursing. 2018;31(111):52-64. [View at Publisher] [DOI] [Google Scholar]
8. Wangensteen S, Finnbakk E, Adolfsson A, Kristjansdottir G, Roodbol P, Ward H, et al. Postgraduate nurses' self-assessment of clinical competence and need for further training. A European cross-sectional survey. Nurse Educ Today. 2018;62:101-6. [View at Publisher] [DOI] [PMID] [Google Scholar]
9. Shokrzadeh M, Jafari D, Hoseinpoor R, Delaram A, Pouyan Sadr A, Masodi E, et al. Frequency of Poisoning Leading to Hospitalization in the Intensive Care Units in Northeastern Iran, 2008-2018. J Res Dev Nurs Midw. 2021;18(1):26-9. [View at Publisher] [DOI] [Google Scholar]
10. Willman A, Bjuresäter K, Nilsson J. Newly graduated registered nurses' self‐assessed clinical competence and their need for further training. Nurs Open. 2020;7(3):720-30. [View at Publisher] [DOI] [PMID] [Google Scholar]
11. Zakeri MA, Bazmandegan G, Ganjeh H, Zakeri M, Mollaahmadi S, Anbariyan A, et al. Is nurses' clinical competence associated with their compassion satisfaction, burnout and secondary traumatic stress? A cross‐sectional study. Nurs Open. 2020;8(1):354-63. [View at Publisher] [DOI] [PMID] [Google Scholar]
12. Jeon Y, Meretoja R, Vahlberg T, Leino‐Kilpi H. Developing and psychometric testing of the anaesthesia nursing competence scale. J Eval Clin Pract. 2020;26(3):866-78. [View at Publisher] [DOI] [PMID] [Google Scholar]
13. Fukada M. Nursing competency: Definition, structure and development. Yonago Acta Med. 2018;61(1):1-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
14. Sasaki S, Fukada M, Okuda R, Fujihara Y. Impact of Organization and Career Commitment on Clinical Nursing Competency. Yonago Acta Med. 2019;62(2):221-31. [View at Publisher] [DOI] [PMID] [Google Scholar]
15. Elhami S, Ban M, Mousaviasl S, Zahedi A. Self-Evaluation of Nurses Clinical Competency based on Benner Theory. Middle East Journal of Family Medicine. 2018;16(3):191-7. [View at Publisher] [DOI] [Google Scholar]
16. Faraji A, Karimi M, Azizi SM, Janatolmakan M, Khatony A. Evaluation of clinical competence and its related factors among ICU nurses in Kermanshah-Iran: A cross-sectional study. Int J Nurs Sci. 2019;6(4):421-5. [View at Publisher] [DOI] [PMID] [Google Scholar]
17. Karami A, Farokhzadian J, Foroughameri G. Nurses' professional competency and organizational commitment: is it important for human resource management? PLoS One. 2017;12(11):e0187863. [View at Publisher] [DOI] [PMID] [Google Scholar]
18. Hassani P, Abdi A, Jalali R, Salari N. Relationship between the use of intuition in clinical practice and the clinical competence of critical care nurses. Int J Evid Based Healthc. 2017;15(4):171-7. [View at Publisher] [DOI] [PMID] [Google Scholar]
19. Mirlashari J, Qommi R, Nariman S, Bahrani N, Begjani J. Clinical competence and its related factors of nurses in neonatal intensive care units. J Caring Sci. 2016;5(4):317-24. [View at Publisher] [DOI] [PMID] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |





