Volume 19, Issue 2 (9-2022)
J Res Dev Nurs Midw 2022, 19(2): 37-40 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abdollahi F, Taher Harikandeie S S, Dehghankar L, Tayebi Myaneh Z, Zarrabadi Pour S. Evaluation of Relationship between Health Literacy and Illness Perception in Patients with Multiple Sclerosis in Iran. J Res Dev Nurs Midw 2022; 19 (2) :37-40
URL: http://nmj.goums.ac.ir/article-1-1285-en.html
URL: http://nmj.goums.ac.ir/article-1-1285-en.html
Fariba Abdollahi1 

 , Seyede Soghra Taher Harikandeie2
, Seyede Soghra Taher Harikandeie2 

 , Leila Dehghankar3
, Leila Dehghankar3 

 , Zahra Tayebi Myaneh2
, Zahra Tayebi Myaneh2 

 , Simin Zarrabadi Pour3
, Simin Zarrabadi Pour3 




 , Seyede Soghra Taher Harikandeie2
, Seyede Soghra Taher Harikandeie2 

 , Leila Dehghankar3
, Leila Dehghankar3 

 , Zahra Tayebi Myaneh2
, Zahra Tayebi Myaneh2 

 , Simin Zarrabadi Pour3
, Simin Zarrabadi Pour3 


1- Department of Medical Sciences, Qazvin branch, Islamic Azad University, Qazvin, Iran
2- Department of Nursing, School of Nursing, Alborz University of Medical Sciences, Alborz, Iran
3- Department of Nursing, Social Determinants of Health Research Center, Qazvin University of Medical Sciences, Qazvin, Iran
2- Department of Nursing, School of Nursing, Alborz University of Medical Sciences, Alborz, Iran
3- Department of Nursing, Social Determinants of Health Research Center, Qazvin University of Medical Sciences, Qazvin, Iran
Full-Text [PDF 618 kb]
(1223 Downloads)
| Abstract (HTML) (2960 Views)
Full-Text: (353 Views)
Introduction
Multiple sclerosis (MS) is an autoimmune and progressive disease that lead to impaired neurotransmission as well as sensory and motor function (1-2). An estimated 2.5 million people worldwide are living with MS (3). The incidence rate of MS in Iran is reported to be 5-5.89 cases per 100,000 persons (4). This debilitating disease has significant economic, social, psychological, and physical consequences (2, 5, and 6).
Chronic diseases is one of the leading causes of psychological and cognitive disorders, illness perception is influenced by several factors including individual, social and environmental factors These factors influence the patient's perception of the nature, cause, treatability, controllability, and consequences of the illness (2, 5, and 6). It is important to examine the consequences of MS, such as illness perception. Research shows that illness perception in patients with chronic illnesses, such as MS, affects disease management, treatment, follow-up, and adaptation as well as quality of life. Lack of self-perception of illness leads to social-psychological dysfunction (6-7).
Given the extent of the physical and psychological complications of MS, it is essential to improve quality of life in patients with MS (5). Providing support and promoting illness perception can be an effective approach to improve the quality of life of patients with MS. In this regard, determining illness perception among patients with MS should be considered as part of health care services. As key personnel in healthcare services, nurses play a vital role in promoting illness perception (7).Moving towards patient-centered health care systems and active patient participation in treatment require a high level of health literacy (1,8, and 9). Health literacy is a key determinant of community health defined as the social and cognitive skills leading to the preservation and promotion of health (10-11). According to previous studies, health literacy in Iran is inadequate (1,8), which has negative effects on physical and mental functioning, medication compliance, self-care behaviors, participation in medical decision making, disease management, and quality of life (7,8,12,13). Health literacy is influenced by several factors including individual factors such as age, sex, race, and education as well as social, economic, cultural, and language factors. Despite the importance of health literacy in management of chronic diseases, a limited number of studies has been conducted to determine factors related to health literacy in different societies (1,12,and14). In Jafari’s (2018) research, Correlation test showed a positive and significant relationship between caregivers' health literacy and the behavior of women with MS (P<0.001, r=0.35) (15). low health literacy has negative effects on illness perception and medication compliance (16). in Perez’s (2015) research, correlation test showed a significant relationship between acculturation, health literacy and illness perception (17). There is limited evidence related to health literacy and illness perception in patients with Multiple Sclerosis Context. Moreover, the impact of health literacy on different aspects of illness perception in patients with MS is not clear (18,19). Therefore, the present study aimed to determine the relationship between health literacy and illness perception in patients with MS.
Methods
This was a correlational study performed on patients with MS who had been referred to neurology clinic of Abu Ali Sina Hospital in Qazvin (Iran) from August 2017 to March 2018.
An a priori power analysis was conducted, indicating that for a significance level of .05, and power of .95, a minimum sample size of 100 participants would be needed for the analysis in this study (17).
Inclusion criteria consisted of having MS based on medical records, age of over 18 years, no mental and psychological illness, and having minimum reading and writing skills. Subjects who did not answer to more than 20% of questions and those unwilling to participate in the study were excluded. Data were collected using a demographic and illness characteristics questionnaire, the brief illness perception questionnaire (BIPQ), and the Newest Vital Sign (NVS) health literacy instrument. The BIPQ was developed by Broadbent et al. (2006) and measures the outcomes, duration, personal control, treatment control, nature, concerns, perception and recognition of current illness, as well as emotional response, and the cause of the disease. The questionnaire consists of nine items. The first eight items are scored 0-10, three items (2,3, and 6) are reverse-scored, and the ninth item is an open-ended question on the three major causes of the disease from the patient's perspective. In the final analysis, each subscale should be analyzed separately. The total score of illness perception is obtained by summing the scores of items one to eight (score of 0-80), and a lower score indicates stronger illness perception. Scores of 0 to 27, 28-55, and 56-80 indicate high, moderate, and low illness perceptions, respectively (17). A Cronbach's alpha coefficient of 0.8 has been reported for this questionnaire, and the test-retest reliability coefficient with a six-week interval for different questions ranged from 0.42 to 0.75 (5).
The NVS health literacy instrument was designed by Weiss et al. (2005) in the United States to assess functional health literacy, assessing reading comprehension and numeracy skills. The questionnaire includes six questions and requires three minutes to complete. Scores vary from 0 to 6, with higher scores indicating higher degrees of literacy. A score of more than 4 indicates adequate literacy, A score 2 to 3 indicates a possibility of limited health literacy, whereas a score of less than 1 indicates a high likelihood of limited health literacy.To complete this questionnaire, a standard ice cream nutritional label was given to each subject. The subject held on to the label until all questions were answered. Cronbach's alpha coefficient for this questionnaire was 0.8, indicating the appropriate internal homogeneity of the questionnaire (20).
The study was approved by the Ethics Committee of Iran University of Medical Sciences (ethical code: IUMS.REC.1395.28546), and written informed consent was taken from all participants.
Analysis of data was carried out using SPSS Statistics 22.0. Normal distribution of data was tested using the Kolmogorov-Smirnov test, and the Pearson correlation coefficient was used to investigate the correlation of health literacy with illness perception and its related factors. Two linear regression models were used to determine the predictors of health literacy and patients' illness perception, so that in the first linear regression model, patients' health literacy was predicted by age, gender, level of education, marital status, occupation, income, insurance status, duration of illness, and body mass index (BMI). Then, using the second linear regression model, patients' illness perception, as a dependent variable, was predicted by health literacy and other independent variables used in the first regression model. The statistical significance level was set at 0.05.
Results
Most of the patients were female (75%), married (70%), and university graduates (64%). The mean age of patients and duration of illness were 33.43±8.53 years and 4.3±4.48 years, respectively (Table 1). Based on the results, Adequate HL level was found in 11% of patients; 26% had intermediate HL level, and 63% had low HL level Moreover, the mean score of illness perception was 35.53±1.31.
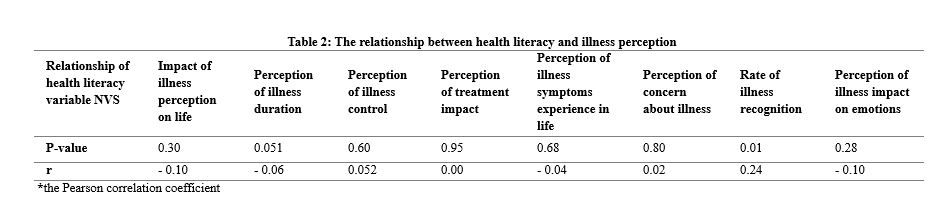
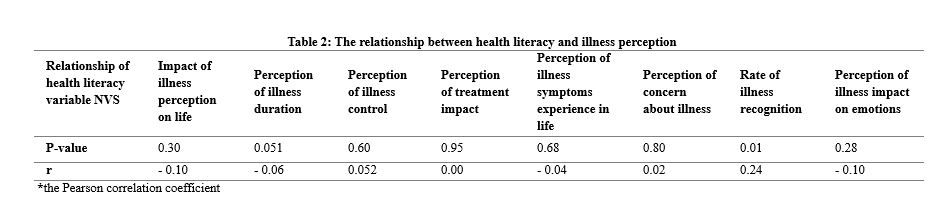
There was a weak correlation between health literacy and the mean score of illness perception among patients with MS (r=-0/014, P=0.893). In addition, there was a significant relationship between health literacy and perception and recognition of present illness, as a subscale of illness perception (r=0.243, P=0.015) (Table 2).
Duration of illness was found as the only variable that could predict health literacy (β=0/052, P=0.035). The independent variables of the regression model completely explained 37.6% of the health literacy changes (Table 3).
When investigating predictors of illness perception, only income could significantly predict illness perception (β=1.87, P=0.05). This model predicted 35.7% of the illness perception changes (Table 4).
Discussion
This study aimed to investigate the relationship between health literacy and illness perception in patients with MS. The results showed that 63% of patients had a high likelihood of limited health literacy, as in previous studies, different results have been reported (8, 10, 12, 21, 22). The conflict may reflect that they used different measures for health literacy (the Rapid Estimate of Adult Literacy in Medicine (12), the S-TOFHLA tool (22 (or due to differences in the research setting, educational systems and the duration of illness (17).
In the present study, income was found as a predictor of illness perception in patients with MS. People with higher incomes achieved a higher illness perception score. Consistent with this finding, a study by Boonsatean et al. (2016) on patients with type 2 diabetes showed that poor socioeconomic status is accompanied with lower illness perception. On the other hand, income is significantly correlated with education level so that people with higher education level have more opportunities to earn money, and Low income is accompanied with lower quality of life (23). Previous studies also reported that ethnic minorities with lower income and lower education levels often have low health literacy (16, 19, and 24). This study demonstrated that low income significantly predict illness perception. Studies on the other groups of patients showed similar findings, chronic illness can cause several complications such as tension, fear, depressed mood, it may have negative effect on illness perception (20).
Duration of the illness was found as another predictor of health literacy in a way that patients who had the illness for a longer time had higher health literacy. This may be related to the fact that having to deal with an illness for a longer period provides the opportunity to obtain sufficient information about the disease. Contrary to this finding, Marrie et al. (2014) reported that a shorter illness duration was accompanied by an increase in health literacy score in patients with MS (19). The inconsistency of the findings on this issue could be related to differences in study environment, ethnicity, demographic characteristics, and patient's tendency to obtain quick access to information at the onset of the disease.
Our results show no association between health literacy and the mean total score of illness perception, this study demonstrated that duration of illness perception significantly associated with health literacy. Health literacy is significantly related to patients' knowledge so that higher health literacy is accompanied with increased disease awareness (25). According to the Common Sense Model, patients' illness perception is influenced by the information provided to them (26), and the relationship between health literacy and illness perception could be justified by increased awareness and recognition of the disease
. Shiyanbola et al. (2018) stated that health literacy was significantly associated with disease risk perception in patients with type 2 diabetes so that low health literacy led to increased disease risk perception and poor adherence to treatment (27).
In a study by Basharpoor et al. (2015), perception of illness duration and illness concern in cancer patients were significantly correlated with health literacy (28). A study by Federman et al. (2013) also showed that asthma patients with poor health literacy believed that their illness is present only at the time of symptoms manifestation, and did not believe that the nature of illness is chronic (22). Perez et al. (2015) reported a significant relationship between health literacy, culture, and illness perception (disease outcomes, control, symptoms, and emotions) (17). However, we found no significant relationship between health literacy and illness perception (illness duration and concern of illness). This inconsistency could be related to the differences in the study population, culture, and health literacy measurement tools.
In explaining the research findings can be stated Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information needed to make appropriate health decisions given the small study population and the sampling method used in the present study, it was not possible to reach a definite conclusion about causal relationship. Therefore, caution should be exercised when generalizing the results of the present study. One of the limitations of this study is the type of questionnaire used to measure health literacy because it focuses only on reading and computing skills, while these skills are only part of the health literacy skills.
Conclusion
The findings from this study indicate a substantial opportunity for improving illness perception, through improved health literacy. Health literacy appears to be the strongest identified factor that influences illness perception. To date, enhancing diabetes-related health literacy by developing readable health-care materials has been the most frequent intervention in general practice. Interventions to enhance health literacy of patients with T2DM is recommended in order to improve illness perception. It is essential to promote health literacy in order to improve understanding the nature and consequences of the disease, as well as to increase the ability to adapt to the disease.
Acknowledgements
The findings of the present study were derived from a research project approved by the Iran University of Medical Sciences, Iran. The authors would like to appreciate all participants, officials at the Iran University of Medical Sciences and Qazvin University of Medical Sciences, and the respected colleagues at Booali Sina Hospital for their cooperation.
Funding source
his research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors
Ethical statement
Written consent was obtained from all individuals prior to participation in the study. The study was approved by the Ethics Committee of Iran University of Medical Sciences (ethical code: IUMS.REC.1395.28546).
Conflict of interest
The authors declare that there is no conflict of interest regarding publication of this article.
Author contributions
The authors confirm contribution to the paper as follows: study conception and design: Abdollahi.F; data collection: Taher Harikandeie.S, Dehghankar. L; analysis and interpretation of results: Tayebi Myaneh.Z, Zarrabadi Pour.S; draft manuscript preparation: Taher Harikandeie.S, Abdollahi.F. All authors reviewed the results and approved the final version of the manuscript.

.JPG)
.JPG)
Multiple sclerosis (MS) is an autoimmune and progressive disease that lead to impaired neurotransmission as well as sensory and motor function (1-2). An estimated 2.5 million people worldwide are living with MS (3). The incidence rate of MS in Iran is reported to be 5-5.89 cases per 100,000 persons (4). This debilitating disease has significant economic, social, psychological, and physical consequences (2, 5, and 6).
Chronic diseases is one of the leading causes of psychological and cognitive disorders, illness perception is influenced by several factors including individual, social and environmental factors These factors influence the patient's perception of the nature, cause, treatability, controllability, and consequences of the illness (2, 5, and 6). It is important to examine the consequences of MS, such as illness perception. Research shows that illness perception in patients with chronic illnesses, such as MS, affects disease management, treatment, follow-up, and adaptation as well as quality of life. Lack of self-perception of illness leads to social-psychological dysfunction (6-7).
Given the extent of the physical and psychological complications of MS, it is essential to improve quality of life in patients with MS (5). Providing support and promoting illness perception can be an effective approach to improve the quality of life of patients with MS. In this regard, determining illness perception among patients with MS should be considered as part of health care services. As key personnel in healthcare services, nurses play a vital role in promoting illness perception (7).Moving towards patient-centered health care systems and active patient participation in treatment require a high level of health literacy (1,8, and 9). Health literacy is a key determinant of community health defined as the social and cognitive skills leading to the preservation and promotion of health (10-11). According to previous studies, health literacy in Iran is inadequate (1,8), which has negative effects on physical and mental functioning, medication compliance, self-care behaviors, participation in medical decision making, disease management, and quality of life (7,8,12,13). Health literacy is influenced by several factors including individual factors such as age, sex, race, and education as well as social, economic, cultural, and language factors. Despite the importance of health literacy in management of chronic diseases, a limited number of studies has been conducted to determine factors related to health literacy in different societies (1,12,and14). In Jafari’s (2018) research, Correlation test showed a positive and significant relationship between caregivers' health literacy and the behavior of women with MS (P<0.001, r=0.35) (15). low health literacy has negative effects on illness perception and medication compliance (16). in Perez’s (2015) research, correlation test showed a significant relationship between acculturation, health literacy and illness perception (17). There is limited evidence related to health literacy and illness perception in patients with Multiple Sclerosis Context. Moreover, the impact of health literacy on different aspects of illness perception in patients with MS is not clear (18,19). Therefore, the present study aimed to determine the relationship between health literacy and illness perception in patients with MS.
Methods
This was a correlational study performed on patients with MS who had been referred to neurology clinic of Abu Ali Sina Hospital in Qazvin (Iran) from August 2017 to March 2018.
An a priori power analysis was conducted, indicating that for a significance level of .05, and power of .95, a minimum sample size of 100 participants would be needed for the analysis in this study (17).
Inclusion criteria consisted of having MS based on medical records, age of over 18 years, no mental and psychological illness, and having minimum reading and writing skills. Subjects who did not answer to more than 20% of questions and those unwilling to participate in the study were excluded. Data were collected using a demographic and illness characteristics questionnaire, the brief illness perception questionnaire (BIPQ), and the Newest Vital Sign (NVS) health literacy instrument. The BIPQ was developed by Broadbent et al. (2006) and measures the outcomes, duration, personal control, treatment control, nature, concerns, perception and recognition of current illness, as well as emotional response, and the cause of the disease. The questionnaire consists of nine items. The first eight items are scored 0-10, three items (2,3, and 6) are reverse-scored, and the ninth item is an open-ended question on the three major causes of the disease from the patient's perspective. In the final analysis, each subscale should be analyzed separately. The total score of illness perception is obtained by summing the scores of items one to eight (score of 0-80), and a lower score indicates stronger illness perception. Scores of 0 to 27, 28-55, and 56-80 indicate high, moderate, and low illness perceptions, respectively (17). A Cronbach's alpha coefficient of 0.8 has been reported for this questionnaire, and the test-retest reliability coefficient with a six-week interval for different questions ranged from 0.42 to 0.75 (5).
The NVS health literacy instrument was designed by Weiss et al. (2005) in the United States to assess functional health literacy, assessing reading comprehension and numeracy skills. The questionnaire includes six questions and requires three minutes to complete. Scores vary from 0 to 6, with higher scores indicating higher degrees of literacy. A score of more than 4 indicates adequate literacy, A score 2 to 3 indicates a possibility of limited health literacy, whereas a score of less than 1 indicates a high likelihood of limited health literacy.To complete this questionnaire, a standard ice cream nutritional label was given to each subject. The subject held on to the label until all questions were answered. Cronbach's alpha coefficient for this questionnaire was 0.8, indicating the appropriate internal homogeneity of the questionnaire (20).
The study was approved by the Ethics Committee of Iran University of Medical Sciences (ethical code: IUMS.REC.1395.28546), and written informed consent was taken from all participants.
Analysis of data was carried out using SPSS Statistics 22.0. Normal distribution of data was tested using the Kolmogorov-Smirnov test, and the Pearson correlation coefficient was used to investigate the correlation of health literacy with illness perception and its related factors. Two linear regression models were used to determine the predictors of health literacy and patients' illness perception, so that in the first linear regression model, patients' health literacy was predicted by age, gender, level of education, marital status, occupation, income, insurance status, duration of illness, and body mass index (BMI). Then, using the second linear regression model, patients' illness perception, as a dependent variable, was predicted by health literacy and other independent variables used in the first regression model. The statistical significance level was set at 0.05.
Results
Most of the patients were female (75%), married (70%), and university graduates (64%). The mean age of patients and duration of illness were 33.43±8.53 years and 4.3±4.48 years, respectively (Table 1). Based on the results, Adequate HL level was found in 11% of patients; 26% had intermediate HL level, and 63% had low HL level Moreover, the mean score of illness perception was 35.53±1.31.
There was a weak correlation between health literacy and the mean score of illness perception among patients with MS (r=-0/014, P=0.893). In addition, there was a significant relationship between health literacy and perception and recognition of present illness, as a subscale of illness perception (r=0.243, P=0.015) (Table 2).
Duration of illness was found as the only variable that could predict health literacy (β=0/052, P=0.035). The independent variables of the regression model completely explained 37.6% of the health literacy changes (Table 3).
When investigating predictors of illness perception, only income could significantly predict illness perception (β=1.87, P=0.05). This model predicted 35.7% of the illness perception changes (Table 4).
Discussion
This study aimed to investigate the relationship between health literacy and illness perception in patients with MS. The results showed that 63% of patients had a high likelihood of limited health literacy, as in previous studies, different results have been reported (8, 10, 12, 21, 22). The conflict may reflect that they used different measures for health literacy (the Rapid Estimate of Adult Literacy in Medicine (12), the S-TOFHLA tool (22 (or due to differences in the research setting, educational systems and the duration of illness (17).
In the present study, income was found as a predictor of illness perception in patients with MS. People with higher incomes achieved a higher illness perception score. Consistent with this finding, a study by Boonsatean et al. (2016) on patients with type 2 diabetes showed that poor socioeconomic status is accompanied with lower illness perception. On the other hand, income is significantly correlated with education level so that people with higher education level have more opportunities to earn money, and Low income is accompanied with lower quality of life (23). Previous studies also reported that ethnic minorities with lower income and lower education levels often have low health literacy (16, 19, and 24). This study demonstrated that low income significantly predict illness perception. Studies on the other groups of patients showed similar findings, chronic illness can cause several complications such as tension, fear, depressed mood, it may have negative effect on illness perception (20).
Duration of the illness was found as another predictor of health literacy in a way that patients who had the illness for a longer time had higher health literacy. This may be related to the fact that having to deal with an illness for a longer period provides the opportunity to obtain sufficient information about the disease. Contrary to this finding, Marrie et al. (2014) reported that a shorter illness duration was accompanied by an increase in health literacy score in patients with MS (19). The inconsistency of the findings on this issue could be related to differences in study environment, ethnicity, demographic characteristics, and patient's tendency to obtain quick access to information at the onset of the disease.
Our results show no association between health literacy and the mean total score of illness perception, this study demonstrated that duration of illness perception significantly associated with health literacy. Health literacy is significantly related to patients' knowledge so that higher health literacy is accompanied with increased disease awareness (25). According to the Common Sense Model, patients' illness perception is influenced by the information provided to them (26), and the relationship between health literacy and illness perception could be justified by increased awareness and recognition of the disease
. Shiyanbola et al. (2018) stated that health literacy was significantly associated with disease risk perception in patients with type 2 diabetes so that low health literacy led to increased disease risk perception and poor adherence to treatment (27).
In a study by Basharpoor et al. (2015), perception of illness duration and illness concern in cancer patients were significantly correlated with health literacy (28). A study by Federman et al. (2013) also showed that asthma patients with poor health literacy believed that their illness is present only at the time of symptoms manifestation, and did not believe that the nature of illness is chronic (22). Perez et al. (2015) reported a significant relationship between health literacy, culture, and illness perception (disease outcomes, control, symptoms, and emotions) (17). However, we found no significant relationship between health literacy and illness perception (illness duration and concern of illness). This inconsistency could be related to the differences in the study population, culture, and health literacy measurement tools.
In explaining the research findings can be stated Health literacy is the degree to which individuals have the capacity to obtain, process, and understand basic health information needed to make appropriate health decisions given the small study population and the sampling method used in the present study, it was not possible to reach a definite conclusion about causal relationship. Therefore, caution should be exercised when generalizing the results of the present study. One of the limitations of this study is the type of questionnaire used to measure health literacy because it focuses only on reading and computing skills, while these skills are only part of the health literacy skills.
Conclusion
The findings from this study indicate a substantial opportunity for improving illness perception, through improved health literacy. Health literacy appears to be the strongest identified factor that influences illness perception. To date, enhancing diabetes-related health literacy by developing readable health-care materials has been the most frequent intervention in general practice. Interventions to enhance health literacy of patients with T2DM is recommended in order to improve illness perception. It is essential to promote health literacy in order to improve understanding the nature and consequences of the disease, as well as to increase the ability to adapt to the disease.
Acknowledgements
The findings of the present study were derived from a research project approved by the Iran University of Medical Sciences, Iran. The authors would like to appreciate all participants, officials at the Iran University of Medical Sciences and Qazvin University of Medical Sciences, and the respected colleagues at Booali Sina Hospital for their cooperation.
Funding source
his research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors
Ethical statement
Written consent was obtained from all individuals prior to participation in the study. The study was approved by the Ethics Committee of Iran University of Medical Sciences (ethical code: IUMS.REC.1395.28546).
Conflict of interest
The authors declare that there is no conflict of interest regarding publication of this article.
Author contributions
The authors confirm contribution to the paper as follows: study conception and design: Abdollahi.F; data collection: Taher Harikandeie.S, Dehghankar. L; analysis and interpretation of results: Tayebi Myaneh.Z, Zarrabadi Pour.S; draft manuscript preparation: Taher Harikandeie.S, Abdollahi.F. All authors reviewed the results and approved the final version of the manuscript.

.JPG)
.JPG)
Type of study: Original Article |
Subject:
Management and Health System
References
1. pooryaghob, M., Abdollahi, F., Mobadery, T., haji shabanha, N., Bajalan, Z. Assesse the Health literacy in Multiple Sclerosis patients. Journal of Health Literacy. 2018; 2(4):266-274. [Persian]. [View at paplisher] [DOI] [Google Scholar]
2. Morowati Sharifabad M, Momeni Z, Eslami M, DehghaniTafti A, Hakimzadeh A. Study of Factors Associated with Self-Care Behaviors in Patients with Multiplesclerosis in Yazd City Based on Health Belief Model. TB. 2016; 15(2):82-93[Persian]. [View at paplisher] [Google Scholar]
3. Nazari F, Soheili M, Hosseini S, Shaygannejad V.A comparison of the effects of reflexology and relaxation on pain in women with multiple sclerosis.Journal of Complementary and Integrative Medicine. 2016; 13(1):65-71. [View at paplisher] [DOI] [Google Scholar]
4. Dehghani r, kazemi moghaddam v. Investigation of the possible causes of the increased prevalence of multiple sclerosis in Iran: a review. Pars of Jahrom University of Medical Sciences. 2015; 13(2):17–25. [View at paplisher] [DOI] [Google Scholar]
5. aghayousefi, A., shaghaghi, F., dehestani, M., barghi irani, Z. The Relationship between Quality of Life (QoL) and Psychological Capital with Illness Perception in MS Patients. Health Psychology, 2012; 1(1):29-41[Persian]. [View at paplisher] [Google Scholar]
6. Abdollahi F, Tayebi Myaneh Z, Rashvand F. The Relationship between Perception of Illness and Health-related Behaviors in Patients with Multiple Sclerosis. JHC. 2019; 21(2):145-155. [Persian] [View at paplisher] [DOI] [Google Scholar]
7. Obiwuru O, Joseph S, Liu L, Palomeque A, Tarlow L, Langer-Gould AM, et al. Perceptions of multiple sclerosis in Hispanic Americans: need for targeted messaging. International Journal of MS Care. 2017; 19(3):131-39. [View at paplisher] [DOI] [Google Scholar]
8. Khosravi A, Ahmadzadeh KH. Investigating health literacy Level of patients referred to Bushehr hospitals and recognizing its effective factors. Iran South Med J. 2016;18(6):1245-1253. [View at paplisher] [Google Scholar]
9. Peyman N,Peyman N, Doosti H. Health Literacy and Health-promoting Lifestyle among Health Volunteers in Neyshabour. Journal of Ilam univ med sci. 2018; 26(3):7-15. [View at paplisher] [DOI] [Google Scholar]
10. Mohammadpour M, Zarifinezhad E, Armand R. A Study of Correlation between Applied Health Literacy and Self-Care Behaviors in Hypertensive Patients of Gachsaran City, 2016. Qom Univ Med Sci J.2018; 12(10): 55-65 [Persian]. [View at paplisher] [DOI] [Google Scholar]
11. Izadirad H, Niknami S, Zareban I, Hidarnia A, Masoudy G. Relationship between health literacy and prenatal care in young pregnant women. J Health Lit. 2017; 2(3) :141-147. [View at paplisher] [DOI] [Google Scholar]
12. Ghanbari A, Rahmatpour P, Khalili M, Mokhtari N. Health Literacy and its Relationship with Cancer Screening Behaviors among the Employees of Guilan University of Medical Sciences Journal of Health and Care. 2017; 18(4):306-315. [Persian] [View at paplisher] [DOI] [Google Scholar]
13. SheikhSharafi H, Seyedamini B. Assessment of health literacy and self-care in heart failure patients. J Health Lit. 2017; 1(4):203-219. [View at paplisher]
14. Schulz PJ, Pessina A, Hartung U, Petrocchi S. Effects of Objective and Subjective Health Literacy on Patients’ Accurate Judgment of Health Information and Decision-Making Ability: Survey Study J Med Internet Res 2021;23(1):e20457. [View at paplisher] [DOI] [Google Scholar]
15. Jafari Y, Vahedian-Shahroodi M, Tehrani H, Esmaily H, Haresabadi M, Shariati M. The relationship between caregivers' health literacy and the behavior of women with Multiple Sclerosis. Iranian journal of obstetrics, Gynecology and infertility.2018; 21(7):64-71. [View at paplisher] [Google Scholar]
16. Kale M, Federman A, Krauskopf K, Wolf M, Conor R, Martynenko M,Leventhal H,Wisnivesky.The Association of Health Literacy with Illness and Medication Beliefs among Patients with Chronic Obstructive Pulmonary Disease J,PLoS ONE. 2015; 10(4). [View at paplisher] [DOI] [Google Scholar]
17. Perez A. Acculturation, Health Literacy, and Illness Perceptions of Hypertension among Hispanic Adults. J Transcult Nurs. 2015; 26(4):386-94. [View at paplisher] [DOI] [Google Scholar]
18. Farghadani Z, Taheri-Kharameh Z, Amiri-Mehra A, Ghajari H, Barati M. The relationship between health literacy and self-care behaviors among patients with heart failure. Hayat, Journal of School of Nursing and Midwifery, Tehran University of Medical Sciences. 2018; 24(2):186-196. (Persian) [View at publisher] [Google Scholar] [View at paplisher] [DOI] [Google Scholar]
19. Marrie R, MD, Salter A, Tyry T, Fox R, and Cutter G. Health Literacy Association with Health Behaviors and Health Care Utilization in Multiple Sclerosis: A Cross-Sectional Study, Interact J Med Res. 2014;3(1):3-14. [View at paplisher] [Google Scholar]
20. Javadzade H, Sharifirad Gh, Reisi M, Tavassoli E, Rajati F. Health Literacy among Adults of Isfahan, Iran. J Health Syst Res 2013; 9(5):540-9[Persian]. [View at paplisher] [Google Scholar]
21. Yousefi A, Shaghaghi F, Dehestani M, BarghiIrani Z. The relationship between quality of life (QoL) and psychological capital with illness perception in MS patients. Health Psychology. 2012; 1(2):10-12 [Persian]. [View at paplisher] [Google Scholar]
22. Federman a , Alex D., Michael Wolf b, Anastasia Sofianou a, Elizabeth A.H. Wilson b, Melissa Martynenko Ethan A. Halm c, Howard Leventhal d, Juan P. Wisnivesky The association of health literacy with illness and medication beliefs among older adults with asthma. Patient Education and Counseling Iournal. 2013:92(2); 273–278. [View at paplisher] [DOI] [Google Scholar]
23. BoonsateanW, DychawyRosner I, Carlsson A and Östman M. The Influences of Income and Education on the Illness Per¬ception and Self-Management of Thai Adults with Type 2 Diabetes.J Diabetes MetabDisord 2016:3(2); 1-8. [View at paplisher] [DOI] [Google Scholar]
24. Yen-Ming Huang, Olayinka O Shiyanbola1 Paul D Smith. Association of health literacy and medication self-efficacy with medication adherence and diabetes control. Patient Preference and Adherence. 2018:12; 793–802. [View at paplisher] [DOI] [Google Scholar]
25. Cavanaugh K, Osborn C, Tentori F, Rothman R, Ikizler T, WallstonK. Performance of a brief survey to assess health literacy in patients receiving hemodialysis. Clinical Kidney Journal. 2015; 8(4): 462–468. [View at paplisher] [DOI] [Google Scholar]
26. Kale M, Federman A, Krauskopf K, Wolf M, Conor R, MartynenkoM,LeventhalH,Wisnivesky. The Association of Health Literacy with Illness and Medication Beliefs among Patients with Chronic Obstructive Pulmonary Disease. J,PLoS ONE.2014;10(4). [View at paplisher] [DOI] [Google Scholar]
27. O.Shiyanbola, Elizabeth Unni, Yen-Ming Huang,Cameron Lanier. The association of health literacy with illness perceptions, medication beliefs, and medication adherence among individuals with type 2 diabetes.Research in Social and Administrative Pharmacy. 2018;14(9):824-830. [View at paplisher] [DOI] [Google Scholar]
28. Basharpoor S, NasriNasrabadi B, Heidari F, Molavi P. The Role of Health Beliefs and Illness Perceptions in Predicting Health-Promoting Behaviors in Cancer Patients.Iran J Health Educ Health Promot. 2018; 6(2): 102-113. [View at paplisher] [DOI] [Google Scholar]
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |



