Volume 20, Issue 1 (4-2023)
J Res Dev Nurs Midw 2023, 20(1): 4-7 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Tabarsa Z, Yazdi K, Amirkhanloo S, Behnampour N. Prevalence of Recirculation and Related Factors in Hemodialysis Patients in Golestan Province, Iran. J Res Dev Nurs Midw 2023; 20 (1) :4-7
URL: http://nmj.goums.ac.ir/article-1-1278-en.html
URL: http://nmj.goums.ac.ir/article-1-1278-en.html
1- Department of Intensive Care Nursing, School of Nursing and Midwifery, Golestan University of Medical Sciences, Gorgan, Iran
2- Nursing research Center, Golestan University of Medical Sciences, Gorgan, Iran. ,yazdi@goums.ac.ir
3- Department of Internal Medicine, Shahid Sayad Shirazi Educational and Medical Center, Golestan University of Medical Sciences, Gorgan, Iran
4- Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran
2- Nursing research Center, Golestan University of Medical Sciences, Gorgan, Iran. ,
3- Department of Internal Medicine, Shahid Sayad Shirazi Educational and Medical Center, Golestan University of Medical Sciences, Gorgan, Iran
4- Department of Biostatistics and Epidemiology, School of Health, Golestan University of Medical Sciences, Gorgan, Iran
Full-Text [PDF 310 kb]
(1657 Downloads)
| Abstract (HTML) (4059 Views)
Full-Text: (765 Views)
Introduction
Chronic renal failure is a process that leads to the loss of kidney function due to reduced glomerular filtration (1). To survive, a person with ESRD must undergo renal replacement therapy, such as hemodialysis (2). Hemodialysis is a common treatment method in Iran and many other countries (3). The population of patients with renal failure in Iran is 320,000, of which 49% are undergoing hemodialysis treatment (4). Considering the high rate of hemodialysis use in treating patients with renal failure, increasing the quality of dialysis is particularly important. Dialysis is considered to be of good quality when about 70% of the urea in the body is removed during one session, which is called dialysis adequacy and plays a vital role in reducing patient mortality (5). Various factors affect the adequacy of dialysis; vascular access and duration of dialysis sessions are among the factors affecting dialysis adequacy (6). Other factors such as arteriovenous fistula recirculation, variables related to the dialyzer, such as insufficient dialyzer calibration, and patient-related factors such as low vascular access blood flow, patient hypotension, and reducing the duration of hemodialysis sessions decrease the adequacy of dialysis (7).
Insufficient arterial blood flow can lead to recirculation. This condition causes the blood flow rate in the vascular access site to be lower than the extracorporeal blood flow, resulting in the mixing of dialyzed and non-dialyzed blood. Usually, a suitable arterial fistula has a blood flow of about 1000 ml/min. The blood flow of the dialysis machine is 350-500 ml/min under the best conditions. With the proper direction and distance of dialysis needles, arterial and venous blood will never mix. If this is not the case, recirculation will occur (8). Some of the dialyzed blood in dialysis through the venous needle enters the dialyzer again through the arterial needle (7).
Recirculation is diagnosed when the concentration of the blood solution in the arterial line is lower than the systemic circulation. It indicates the mixing of dialyzed and non-dialyzed blood entering the dialyzer. In this phenomenon, the mixing of dialyzed and non-dialyzed blood causes the urea concentration in the blood entering the dialyzer to decrease by between 10-40% or more (9).
The prevalence of recirculation has been reported differently in various studies. In recent studies, its prevalence has been reported to vary from 8 to 17 percent. Abbasi (2015) reported 11.6 percent, Mousavi (2009) reported 17 percent, and Mahboob (2013) reported 8.1 percent (8, 10, 11). The existence of recirculation significantly reduces the adequacy of dialysis. Therefore, periodic assessment of vascular access recirculation in dialysis is crucial for diagnostic purposes in these patients. However, most hemodialysis centers ignore the regular recirculation evaluation of patients (7). Patients with end-stage renal disease (ESRD) depend on hemodialysis for survival. Therefore, periodic assessment of vascular access recirculation indicates the patient's benefit from appropriate dialysis adequacy. Some clinical guidelines consider regular evaluation of recirculation as a method for rapid identification and correction of vascular access (9).
The issue of recirculation and a comprehensive study regarding medical centers is critical. It is used in planning investigations and appropriate actions. The present study was conducted to determine the prevalence of recirculation and related factors among hemodialysis patients in the medical centers of Golestan province, Iran, in 2017.
Methods
This cross-sectional study was conducted with a descriptive-analytical approach on patients with end-stage chronic renal failure undergoing hemodialysis in medical centers of Golestan province, located in northeast Iran in 2017. The study population consisted of patients with end-stage chronic renal failure undergoing hemodialysis in Golestan province at the time of the research. The sample size was determined based on a prevalence of 6.7% of recirculation in the study of Melai et al. (12), a confidence level of 0.95, and a maximum error of 1.5%. With a total population of 747, the sample size in the entire province was determined to be 324 people. The sampling method used was stratified; 11 hemodialysis departments of education and treatment centers in the area were considered as classes. Within each class, simple random sampling was done with proportional allocation. Hemodialysis departments in medical centers of the province were considered as classes. Then, using the list of hemodialysis patients from each center in equal proportion, eligible participants were included in the study using a simple random sampling method.
The study's inclusion criteria include hemodialysis with an arteriovenous fistula or permanent catheter, hemodialysis for at least three months and more than once a week with any type of dialysis machine, dialyzer, and dialysis solution, a pump speed of 250-350 ml per minute, dialysis solution flow of 500 ml per minute with a bicarbonate solution concentration of 35 meq/l (12), the absence of diagnosed mental retardation and psychiatric disorders, and consent to participate in this study. The study did not include hemodialysis patients with temporary vascular access, advanced heart failure, or severe vascular disorders.
A form was used for demographic data collection, such as age, gender, ethnicity, marital status, occupation, monthly income, and education. Clinical information such as the duration of end-stage renal disease, start date of hemodialysis, duration of each session, type of vascular access (arteriovenous fistula or catheter), duration of vascular access, frequency of dialysis per week, distance between venous and arterial needles, distance of needles from arteriovenous fistula, and comorbidities were recorded on another form.
To measure the percentage of recirculation urea, the two-needle method and the formula ([P-A]/ [P-V]*100) were used (1). Here, P refers to the concentration of urea in the peripheral blood, A refers to the attention of urea in the arterial line, and V refers to the attention of urea in the venous line. The cut-off point for the subject was considered to be 10%. Therefore, patients were divided into two groups based on the recirculation percentage: the presence and absence of recirculation. If the recirculation rate of comets was less than 10%, it meant no recirculation, and more than 10% indicated the presence of recirculation (13).
.PNG)
One person conducted all the blood sampling. In the present study, the blood sampling protocol used was 1.5 mL of arterial blood and 1.5 mL of venous blood, taken at most half an hour after the start of dialysis. The blood pump speed of the machine was 250 mL/min from the arterial and venous sets. Then the pump speed was reduced to 50 mL/min, and after 30 seconds, the blood sample was again taken from the arterial location to determine the concentration of peripheral urea (12).
Simultaneously, three blood samples were sent to the central laboratory while maintaining the cold chain at a temperature of 3-5°C. The amount of blood urea was measured using an auto-analyzer BT 3500, which was calibrated with calibrators prior to the test, and Pars test kits. The data was analyzed using SPSS version 16.
Descriptive statistics tests, such as mean, standard deviation, frequency, and percentage of relative frequency, were used to describe demographic and clinical information. The normal distribution of the data was checked using the Kolmogorov-Smirnov test. The chi-square and Fisher's exact tests were used to compare qualitative variables in two groups, and t-tests were used to compare quantitative variables. The significance level of all tests was set to less than 0.05.
The research was approved by the Research Ethics Committee of Golestan University of Medical Sciences in Iran, with the number IR.GOUMS.REC.1397.139.
Results
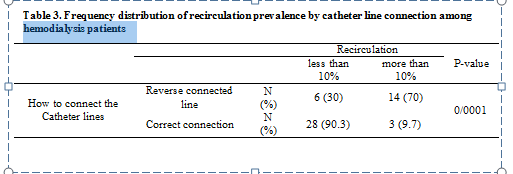
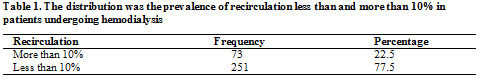
This research showed that the prevalence of recirculation above 10% in patients participating in this study was 22.5%. The recirculation below 10% was 77.5% Table 1.
The mean age of participating patients with recirculation was 58.47 ± 14.16 years. For patients without recirculation, it was 54.79 ± 15.39 years. The mean and standard deviation of vascular access duration in the recirculation group was 28.32 ± 33.64 months. In the group without recirculation, this time was 37.54 ± 38.78 months. The average history of hemodialysis in the group with recirculation was 41.55 ± 19.61 months. The group without recirculation was 47.94 ± 43.90 months. Regarding gender, 170 were male (33 with recirculation and 137 without recirculation). One hundred fifty-four were female (40 people with recirculation and 114 without recirculation).
Regarding the prevalence of recirculation according to the underlying disease, the results showed that the prevalence of recirculation among hemodialysis patients with diabetes was 25.4%, and with hypertension was 23.8%. The chi-square test did not show a statistically significant relationship between recirculation and the type of underlying disease among hemodialysis patients (P = 0.34).
The results showed the prevalence of recirculation according to the location of the fistula. Patients with a fistula in the elbow had more recirculation than those in the wrist and arm. The chi-square test did not show a significant relationship between fistula location and recirculation (P = 0.312) Table 2.
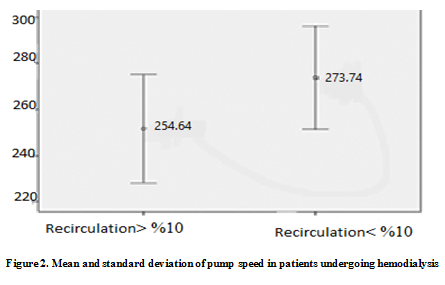
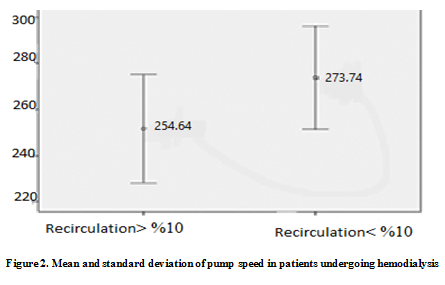
The average pump speed in patients with recirculation was 251.64 ± 23.42. In the group without recirculation, the average pump speed was 273.77 ± 22.35. The result was significant based on the Mann-Whitney U test (P = 3.35×12-12) Figure 1.
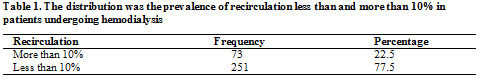
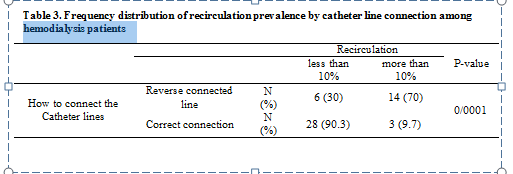
.PNG)
The study results indicate that 70% of patients with a catheter connection called Reverse connected line (connecting the arterial line to the venous line) were in the recirculation group. Only 9.7% of patients who had properly connected catheter lines were in the group without recirculation, and the chi-square test showed a significant relationship between the way catheter lines were connected and the presence of recirculation (P=0.0001) Table 3. Moreover, the results showed that 48.3% of patients who had recirculation of more than 10% had their arterial needle located above the venous needle. There was a significant relationship between the location of the arterial needle and recirculation in the chi-square test (P=0.0001).
The mean and standard deviation of the arterial-venous needle distance with recirculation were 4.12 ± 3.09, while the group without recirculation was 7.38±4.04. Based on the Mann-Whitney test, the result was statistically significant (P = 4.33×10-11) (Figure 2). Furthermore, 19.2% of patients with the opposite direction of the needles had more recirculation than those who had needles in the same direction (3.24%). However, the chi-square test did not show a significant relationship between needle direction and recirculation (P=0.36).
Discussion
The results of the data analysis showed that the prevalence of recirculation among hemodialysis patients in Golestan province, Iran, was 22.5%. In Baladi Mousavi's study (2009), which investigated the prevalence of recirculation in 100 patients undergoing hemodialysis, the rate of recirculation was reported as 17% (10). In Fakhry et al.'s study in 2018 in Egypt, the prevalence of recirculation in arteriovenous fistulas was 42% (14). In 2010, in the survey of recirculation of arteriovenous fistulas in 5 Azar Hospital, Gorgan, Molai et al. reported the prevalence of recirculation to be 15% (13).
Most studies have examined the recirculation rate in arteriovenous fistulas. In the present study, in addition to arteriovenous fistulas, catheters have also been considered. The sample size of the previous studies was small, while the sample size of the present study (324 people) was significant. However, in Fakhry et al.'s study, the recirculation method was based on potassium, which is different from the traditional method based on urea measurement. Analysis of the results did not show a significant relationship between age, gender, duration of vascular access, and recirculation. The results of Vahedi et al.'s study (2017) also showed that the age, gender, and age of the fistula have no significant effect on the recirculation rate (15). The present study showed that in cases where the fistula was located in the elbow cavity of the patients, there was more recirculation than the fistula in the wrist and arm. Data analysis showed no significant relationship between fistula location and recirculation, which was consistent with the study of Molaei et al (6).
In investigating the relation of recirculation with the placement of needles, distance, and direction of venous-arterial needles, it was shown that there is a significant relationship between the placement of needles and recirculation. The recirculation rate was higher when the arterial needle was above the venous needle.
The average distance between arterial and venous needles among hemodialysis patients with recirculation was lower than in patients without recirculation (4.71±4.08). Dagirdaz et al. (2007) emphasized that when using a fistula, the arterial needle should be inserted at the end and at least three centimeters away from the anastomosis site, and the venous needle should be placed 5 centimeters above the arterial needle, which is a more favorable situation (16). In the study of Molaei et al., the direction of the needles and placing the arterial needle above the venous needle caused an increase in recirculation (13). The closer the distance between the arterial needle connection point and the venous needle connection point is, the more likely the dialyzed blood will enter and return to the arterial line, causing an increase in recirculation (17). Previous studies have considered the most common cause of recirculation to be the improper placement of needles, such as their close distance. However, nurses often ignore these parameters, and no technology can assure us that this way of placing the needles is correct and appropriate (18). Vahedi, quoting Basileh et al. (2003), states that the distance between the needles has no effect on recirculation as long as the blood flow of the fistula is greater than the blood flow of the dialysis machine (15). Other factors besides the proper placement of needles, such as severe vein stenosis, improper arterial blood flow, and congestive heart failure, are also factors causing recirculation (10). In the current study, the average pump speed among hemodialysis patients with recirculation was significantly lower than in patients without recirculation. In the case of patients who used catheters, the results showed a higher frequency of recirculation in patients who closed the catheter lines in reverse (venous to arterial line) compared to patients who closed the catheter lines in the correct way.
Atapour et al. (2008) conducted a study on 30 patients undergoing hemodialysis, where 25 patients had permanent catheters and 5 people had temporary catheters. They reported that when the arterial and venous lines were placed in the correct position, the amount of recirculation was less than %10 (19). Abbasi et al. (2015) also showed that the average recirculation rate in people with permanent catheters was 9.5%. People with permanent catheters were divided into two groups. In 11 patients, the arterial and venous lines were appropriately closed, and the recirculation rate was 8.14%. In the 14 patients whose catheter lines were locked in reverse, the recirculation rate was 11.30%. The amount of recirculation was significant based on the approach of the arterial and venous lines in the permanent catheter (8), which was consistent with the results of the present study. However, many other factors such as low flow of vascular access, vascular diseases, and dialyzer characteristics can also influence recirculation, which were not measured in this study due to limitations.
Conclusion
The results of this study show that the location and direction of the arterial-venous needle, the distance between the needles, the method of connecting catheter lines, and the average pump speed are essential factors that affect the prevalence of recirculation in the hemodialysis departments of Golestan province, Iran. Since increased recirculation results in decreased dialysis adequacy, which can ultimately reduce the quality of life and life expectancy of patients, it is crucial to insert the needles accurately to reduce recirculation and improve dialysis quality.
Therefore, it is necessary to train nurses in hemodialysis departments on the proper placement of arterial-venous needles, which should be placed at an appropriate distance from the fistula and in the correct direction relative to each other. Recirculation, observing the aforementioned conditions may signal and predict the occurrence of thrombosis and coagulation at the fistula site, leading to fistula failure. Thus, it is recommended to periodically examine the fistula of patients experiencing recirculation above 10% to check the amount of blood flow or the presence of stenosis using Doppler ultrasound.
Acknowledgement
This article is the result of research project 110077 conducted at Golestan University of Medical Sciences in Iran. Also, it was the result of Zahra Tabarsa's thesis for obtaining a master's degree in critical intensive care nursing from School of Nursing and Midwifery, Golestan University of Medical Sciences. We would like to express our gratitude to the Department of Research and Technology of the University, the Laboratory of 5 Azar Hospital in Gorgan, Iran, for their assistance in the implementation of this research.
Funding source
This research has been supported and funded by the Golestan University of Medical Sciences, Gorgan, Iran (project code: 110077).
Ethical statement
This protocol study has been approved by the Research Ethics Committee of Golestan University of Medical Sciences (Ethical code: IR.GOUMS.REC.1397.139).
Conflict of interest
The authors declare that there is no conflict of interest.
Author contributions
All authors have contributed significantly to this study. Tabarsa and Yazdi designed the project, performed the data collection and wrote the manuscript, Behnampour analyzed data, Amirkhanloo supervised execution of the study and data collection, Yazdi also supervised the study. All the authors approved the content of the manuscript.
Chronic renal failure is a process that leads to the loss of kidney function due to reduced glomerular filtration (1). To survive, a person with ESRD must undergo renal replacement therapy, such as hemodialysis (2). Hemodialysis is a common treatment method in Iran and many other countries (3). The population of patients with renal failure in Iran is 320,000, of which 49% are undergoing hemodialysis treatment (4). Considering the high rate of hemodialysis use in treating patients with renal failure, increasing the quality of dialysis is particularly important. Dialysis is considered to be of good quality when about 70% of the urea in the body is removed during one session, which is called dialysis adequacy and plays a vital role in reducing patient mortality (5). Various factors affect the adequacy of dialysis; vascular access and duration of dialysis sessions are among the factors affecting dialysis adequacy (6). Other factors such as arteriovenous fistula recirculation, variables related to the dialyzer, such as insufficient dialyzer calibration, and patient-related factors such as low vascular access blood flow, patient hypotension, and reducing the duration of hemodialysis sessions decrease the adequacy of dialysis (7).
Insufficient arterial blood flow can lead to recirculation. This condition causes the blood flow rate in the vascular access site to be lower than the extracorporeal blood flow, resulting in the mixing of dialyzed and non-dialyzed blood. Usually, a suitable arterial fistula has a blood flow of about 1000 ml/min. The blood flow of the dialysis machine is 350-500 ml/min under the best conditions. With the proper direction and distance of dialysis needles, arterial and venous blood will never mix. If this is not the case, recirculation will occur (8). Some of the dialyzed blood in dialysis through the venous needle enters the dialyzer again through the arterial needle (7).
Recirculation is diagnosed when the concentration of the blood solution in the arterial line is lower than the systemic circulation. It indicates the mixing of dialyzed and non-dialyzed blood entering the dialyzer. In this phenomenon, the mixing of dialyzed and non-dialyzed blood causes the urea concentration in the blood entering the dialyzer to decrease by between 10-40% or more (9).
The prevalence of recirculation has been reported differently in various studies. In recent studies, its prevalence has been reported to vary from 8 to 17 percent. Abbasi (2015) reported 11.6 percent, Mousavi (2009) reported 17 percent, and Mahboob (2013) reported 8.1 percent (8, 10, 11). The existence of recirculation significantly reduces the adequacy of dialysis. Therefore, periodic assessment of vascular access recirculation in dialysis is crucial for diagnostic purposes in these patients. However, most hemodialysis centers ignore the regular recirculation evaluation of patients (7). Patients with end-stage renal disease (ESRD) depend on hemodialysis for survival. Therefore, periodic assessment of vascular access recirculation indicates the patient's benefit from appropriate dialysis adequacy. Some clinical guidelines consider regular evaluation of recirculation as a method for rapid identification and correction of vascular access (9).
The issue of recirculation and a comprehensive study regarding medical centers is critical. It is used in planning investigations and appropriate actions. The present study was conducted to determine the prevalence of recirculation and related factors among hemodialysis patients in the medical centers of Golestan province, Iran, in 2017.
Methods
This cross-sectional study was conducted with a descriptive-analytical approach on patients with end-stage chronic renal failure undergoing hemodialysis in medical centers of Golestan province, located in northeast Iran in 2017. The study population consisted of patients with end-stage chronic renal failure undergoing hemodialysis in Golestan province at the time of the research. The sample size was determined based on a prevalence of 6.7% of recirculation in the study of Melai et al. (12), a confidence level of 0.95, and a maximum error of 1.5%. With a total population of 747, the sample size in the entire province was determined to be 324 people. The sampling method used was stratified; 11 hemodialysis departments of education and treatment centers in the area were considered as classes. Within each class, simple random sampling was done with proportional allocation. Hemodialysis departments in medical centers of the province were considered as classes. Then, using the list of hemodialysis patients from each center in equal proportion, eligible participants were included in the study using a simple random sampling method.
The study's inclusion criteria include hemodialysis with an arteriovenous fistula or permanent catheter, hemodialysis for at least three months and more than once a week with any type of dialysis machine, dialyzer, and dialysis solution, a pump speed of 250-350 ml per minute, dialysis solution flow of 500 ml per minute with a bicarbonate solution concentration of 35 meq/l (12), the absence of diagnosed mental retardation and psychiatric disorders, and consent to participate in this study. The study did not include hemodialysis patients with temporary vascular access, advanced heart failure, or severe vascular disorders.
A form was used for demographic data collection, such as age, gender, ethnicity, marital status, occupation, monthly income, and education. Clinical information such as the duration of end-stage renal disease, start date of hemodialysis, duration of each session, type of vascular access (arteriovenous fistula or catheter), duration of vascular access, frequency of dialysis per week, distance between venous and arterial needles, distance of needles from arteriovenous fistula, and comorbidities were recorded on another form.
To measure the percentage of recirculation urea, the two-needle method and the formula ([P-A]/ [P-V]*100) were used (1). Here, P refers to the concentration of urea in the peripheral blood, A refers to the attention of urea in the arterial line, and V refers to the attention of urea in the venous line. The cut-off point for the subject was considered to be 10%. Therefore, patients were divided into two groups based on the recirculation percentage: the presence and absence of recirculation. If the recirculation rate of comets was less than 10%, it meant no recirculation, and more than 10% indicated the presence of recirculation (13).
.PNG)
One person conducted all the blood sampling. In the present study, the blood sampling protocol used was 1.5 mL of arterial blood and 1.5 mL of venous blood, taken at most half an hour after the start of dialysis. The blood pump speed of the machine was 250 mL/min from the arterial and venous sets. Then the pump speed was reduced to 50 mL/min, and after 30 seconds, the blood sample was again taken from the arterial location to determine the concentration of peripheral urea (12).
Simultaneously, three blood samples were sent to the central laboratory while maintaining the cold chain at a temperature of 3-5°C. The amount of blood urea was measured using an auto-analyzer BT 3500, which was calibrated with calibrators prior to the test, and Pars test kits. The data was analyzed using SPSS version 16.
Descriptive statistics tests, such as mean, standard deviation, frequency, and percentage of relative frequency, were used to describe demographic and clinical information. The normal distribution of the data was checked using the Kolmogorov-Smirnov test. The chi-square and Fisher's exact tests were used to compare qualitative variables in two groups, and t-tests were used to compare quantitative variables. The significance level of all tests was set to less than 0.05.
The research was approved by the Research Ethics Committee of Golestan University of Medical Sciences in Iran, with the number IR.GOUMS.REC.1397.139.
Results
This research showed that the prevalence of recirculation above 10% in patients participating in this study was 22.5%. The recirculation below 10% was 77.5% Table 1.
The mean age of participating patients with recirculation was 58.47 ± 14.16 years. For patients without recirculation, it was 54.79 ± 15.39 years. The mean and standard deviation of vascular access duration in the recirculation group was 28.32 ± 33.64 months. In the group without recirculation, this time was 37.54 ± 38.78 months. The average history of hemodialysis in the group with recirculation was 41.55 ± 19.61 months. The group without recirculation was 47.94 ± 43.90 months. Regarding gender, 170 were male (33 with recirculation and 137 without recirculation). One hundred fifty-four were female (40 people with recirculation and 114 without recirculation).
Regarding the prevalence of recirculation according to the underlying disease, the results showed that the prevalence of recirculation among hemodialysis patients with diabetes was 25.4%, and with hypertension was 23.8%. The chi-square test did not show a statistically significant relationship between recirculation and the type of underlying disease among hemodialysis patients (P = 0.34).
The results showed the prevalence of recirculation according to the location of the fistula. Patients with a fistula in the elbow had more recirculation than those in the wrist and arm. The chi-square test did not show a significant relationship between fistula location and recirculation (P = 0.312) Table 2.
The average pump speed in patients with recirculation was 251.64 ± 23.42. In the group without recirculation, the average pump speed was 273.77 ± 22.35. The result was significant based on the Mann-Whitney U test (P = 3.35×12-12) Figure 1.
.PNG)
The study results indicate that 70% of patients with a catheter connection called Reverse connected line (connecting the arterial line to the venous line) were in the recirculation group. Only 9.7% of patients who had properly connected catheter lines were in the group without recirculation, and the chi-square test showed a significant relationship between the way catheter lines were connected and the presence of recirculation (P=0.0001) Table 3. Moreover, the results showed that 48.3% of patients who had recirculation of more than 10% had their arterial needle located above the venous needle. There was a significant relationship between the location of the arterial needle and recirculation in the chi-square test (P=0.0001).
The mean and standard deviation of the arterial-venous needle distance with recirculation were 4.12 ± 3.09, while the group without recirculation was 7.38±4.04. Based on the Mann-Whitney test, the result was statistically significant (P = 4.33×10-11) (Figure 2). Furthermore, 19.2% of patients with the opposite direction of the needles had more recirculation than those who had needles in the same direction (3.24%). However, the chi-square test did not show a significant relationship between needle direction and recirculation (P=0.36).
Discussion
The results of the data analysis showed that the prevalence of recirculation among hemodialysis patients in Golestan province, Iran, was 22.5%. In Baladi Mousavi's study (2009), which investigated the prevalence of recirculation in 100 patients undergoing hemodialysis, the rate of recirculation was reported as 17% (10). In Fakhry et al.'s study in 2018 in Egypt, the prevalence of recirculation in arteriovenous fistulas was 42% (14). In 2010, in the survey of recirculation of arteriovenous fistulas in 5 Azar Hospital, Gorgan, Molai et al. reported the prevalence of recirculation to be 15% (13).
Most studies have examined the recirculation rate in arteriovenous fistulas. In the present study, in addition to arteriovenous fistulas, catheters have also been considered. The sample size of the previous studies was small, while the sample size of the present study (324 people) was significant. However, in Fakhry et al.'s study, the recirculation method was based on potassium, which is different from the traditional method based on urea measurement. Analysis of the results did not show a significant relationship between age, gender, duration of vascular access, and recirculation. The results of Vahedi et al.'s study (2017) also showed that the age, gender, and age of the fistula have no significant effect on the recirculation rate (15). The present study showed that in cases where the fistula was located in the elbow cavity of the patients, there was more recirculation than the fistula in the wrist and arm. Data analysis showed no significant relationship between fistula location and recirculation, which was consistent with the study of Molaei et al (6).
In investigating the relation of recirculation with the placement of needles, distance, and direction of venous-arterial needles, it was shown that there is a significant relationship between the placement of needles and recirculation. The recirculation rate was higher when the arterial needle was above the venous needle.
The average distance between arterial and venous needles among hemodialysis patients with recirculation was lower than in patients without recirculation (4.71±4.08). Dagirdaz et al. (2007) emphasized that when using a fistula, the arterial needle should be inserted at the end and at least three centimeters away from the anastomosis site, and the venous needle should be placed 5 centimeters above the arterial needle, which is a more favorable situation (16). In the study of Molaei et al., the direction of the needles and placing the arterial needle above the venous needle caused an increase in recirculation (13). The closer the distance between the arterial needle connection point and the venous needle connection point is, the more likely the dialyzed blood will enter and return to the arterial line, causing an increase in recirculation (17). Previous studies have considered the most common cause of recirculation to be the improper placement of needles, such as their close distance. However, nurses often ignore these parameters, and no technology can assure us that this way of placing the needles is correct and appropriate (18). Vahedi, quoting Basileh et al. (2003), states that the distance between the needles has no effect on recirculation as long as the blood flow of the fistula is greater than the blood flow of the dialysis machine (15). Other factors besides the proper placement of needles, such as severe vein stenosis, improper arterial blood flow, and congestive heart failure, are also factors causing recirculation (10). In the current study, the average pump speed among hemodialysis patients with recirculation was significantly lower than in patients without recirculation. In the case of patients who used catheters, the results showed a higher frequency of recirculation in patients who closed the catheter lines in reverse (venous to arterial line) compared to patients who closed the catheter lines in the correct way.
Atapour et al. (2008) conducted a study on 30 patients undergoing hemodialysis, where 25 patients had permanent catheters and 5 people had temporary catheters. They reported that when the arterial and venous lines were placed in the correct position, the amount of recirculation was less than %10 (19). Abbasi et al. (2015) also showed that the average recirculation rate in people with permanent catheters was 9.5%. People with permanent catheters were divided into two groups. In 11 patients, the arterial and venous lines were appropriately closed, and the recirculation rate was 8.14%. In the 14 patients whose catheter lines were locked in reverse, the recirculation rate was 11.30%. The amount of recirculation was significant based on the approach of the arterial and venous lines in the permanent catheter (8), which was consistent with the results of the present study. However, many other factors such as low flow of vascular access, vascular diseases, and dialyzer characteristics can also influence recirculation, which were not measured in this study due to limitations.
Conclusion
The results of this study show that the location and direction of the arterial-venous needle, the distance between the needles, the method of connecting catheter lines, and the average pump speed are essential factors that affect the prevalence of recirculation in the hemodialysis departments of Golestan province, Iran. Since increased recirculation results in decreased dialysis adequacy, which can ultimately reduce the quality of life and life expectancy of patients, it is crucial to insert the needles accurately to reduce recirculation and improve dialysis quality.
Therefore, it is necessary to train nurses in hemodialysis departments on the proper placement of arterial-venous needles, which should be placed at an appropriate distance from the fistula and in the correct direction relative to each other. Recirculation, observing the aforementioned conditions may signal and predict the occurrence of thrombosis and coagulation at the fistula site, leading to fistula failure. Thus, it is recommended to periodically examine the fistula of patients experiencing recirculation above 10% to check the amount of blood flow or the presence of stenosis using Doppler ultrasound.
Acknowledgement
This article is the result of research project 110077 conducted at Golestan University of Medical Sciences in Iran. Also, it was the result of Zahra Tabarsa's thesis for obtaining a master's degree in critical intensive care nursing from School of Nursing and Midwifery, Golestan University of Medical Sciences. We would like to express our gratitude to the Department of Research and Technology of the University, the Laboratory of 5 Azar Hospital in Gorgan, Iran, for their assistance in the implementation of this research.
Funding source
This research has been supported and funded by the Golestan University of Medical Sciences, Gorgan, Iran (project code: 110077).
Ethical statement
This protocol study has been approved by the Research Ethics Committee of Golestan University of Medical Sciences (Ethical code: IR.GOUMS.REC.1397.139).
Conflict of interest
The authors declare that there is no conflict of interest.
Author contributions
All authors have contributed significantly to this study. Tabarsa and Yazdi designed the project, performed the data collection and wrote the manuscript, Behnampour analyzed data, Amirkhanloo supervised execution of the study and data collection, Yazdi also supervised the study. All the authors approved the content of the manuscript.
Type of study: Original Article |
Subject:
Nursing
References
1. Dehvan F, Monjazebi F, Khanghahi ME, H. Mohammadi H, Gheshlagh R, Kurdi A. Adequacy of Dialysis in Iranian Patients Undergoing Hemodialysis: A Systematic Review and Meta-Analysis. Nephro-Urol Mon. 2018; 10(5).e82235. [View at paplisher] [DOI] [Google Scholar]
2. Parsons TL, Toffelmire EB, King-VanVlack CE. Exercise training during hemodialysis improves dialysis efficacy and physical performance. Archives of physical medicine and rehabilitation. 2006; 87(5):680-687. [View at paplisher] [DOI] [Google Scholar]
3. Ashrafi Z, Ebrahimi H, Sarafha J, The relationship between hemodialysis adequacy and quality of life and spiritual wellbeing in hemodialysis patients. Journal of clinical nursing and midwifery. 2014;4(3):44-51. [View at paplisher] [Google Scholar]
4. Motedayen M, Sarokhani D, Ghiasi B, Khatony A, Hasanpour Dehkordi A. Prevalence of Hypertension in Renal Diseases in Iran: Systematic Review and Meta-Analysis. Int J Prev Med. 2019; 10:124. [View at paplisher] [DOI] [Google Scholar]
5. Abedi Samakoosh M, Aghaie N, Gholami F, Shirzad M, Yosefi E, Teymoorzadeh Baboli M. Assesment Dialysis Adequacy in Hemodialysis Patients of Qaemshar Razi Hospital in 2012. J Mazandaran Univ Med Sci. 2013;23(107):20-27. [View at paplisher] [Google Scholar]
6. Shariati AR, Asayesh H, Nasiri H, Tajbakhsh R, Hesam M, Mollaee E, et all. Comparison of dialysis adequacy in patient's that referred to Golestan province hemodialysis centers. JHPM. 2012;1(3):55-63. [View at paplisher] [Google Scholar]
7. Zeraati A, Beladi Mousavi SS, Beladi Mousavi M. A review article: access recirculation among end stage renal disease patients undergoing maintenance hemodialysis. Nephrourol Mon.2013;5(2):728-32. [View at paplisher] [DOI] [Google Scholar]
8. Abasi M, Lesan Pezeshki M, Asadi N. Study of the Relationship between Vascular Access Types and Recirculation in Chronic Hemodialysis. journal of ilam university of medical sciences. 2015;23(5):81-90. [View at paplisher] [Google Scholar]
9. Gilmore JA. KDOQI clinical practice guidelines and clinical practice recommendations--2006 updates. Nephrology nursing journal. 2006;33(55):487-88. [View at paplisher] [Google Scholar]
10. Beladi Mousavi SS. Arterio-Venous Fistula Recirculation in Hemodialysis: Causes and Prevalences. Shiraz E-Med J.2010;11(4):219-224. [View at paplisher] [Google Scholar]
11. Mahbub T, Chowdhury MN, Jahan F, Islam MN, Khan FM, Sikder NH, Rahman M. Factors responsible for increased percent recirculation in arterio-venous fistula among the haemodialysis patients. Bangladesh Medical Research Council bulletin. 2013;39(1):28-33. [View at paplisher] [DOI] [Google Scholar]
12. Gilpin V, Nichols WK. Vascular access for hemodialysis: thrills and thrombosis. Journal of vascular nursing : official publication of the Society for Peripheral Vascular Nursing. 2010;28(2):78-83. [View at paplisher] [DOI] [Google Scholar]
13. molaei E, aghakhani MJ, Abdollahi AA, Shariati A, Tajbakhsh R. Arteriovenous Fistula Recirculation and its Relationship with Some Factors in Hemodialysis Patients. J Res Dev Nurs Midw. 2010;7(2):15-22. [View at paplisher] [Google Scholar]
14. Fakhry MM, Khedr L, Nour El Din E. Prevalence of Access Recirculation in Prevalent Arterio-Venous (A-V) Fistula Hemodialysis Patients and Its Effect on Hemodialysis Adequacy. The Egyptian Journal of Hospital Medicine. 2018;72(6):4602-4609. [View at paplisher] [DOI] [Google Scholar]
15. Vahedi SA, Aghaali M, Ghanbari Afra L, Asayesh H, Mashhadi F, Saghafi H,et al. The effect of distance and direction of needle cannulation on the recirculation of arteriovenous fistula: A clinical trial. Hayat. 2018;24(2):102-110. [View at paplisher] [Google Scholar]
16. Daugirdas. John BP, Ing. Todd. Handbook of Dialysis. Philadelphia: Lippincott Williams & wilkins; 2007. [View at paplisher] [Google Scholar]
17. Salimi J, Razeghi E, Karjalian H, Meysamie A, Dahhaz M, Dadmehr M. Predicting hemodialysis access failure with the measurement of dialysis access recirculation. Saudi journal of kidney diseases and transplantation. 2008;19(5):781-784. [View at paplisher] [Google Scholar]
18. Laing B, Merlino E, Nelson C. Prevention of Access Recirculation During Hemodialysis Treatment. Bioengineering, :union: College Schenectady, 2019; 2314. [View at paplisher] [Google Scholar]
19. Atapour A, Mosakazemi M, Mortazavi M, Beigi A, Shahidi S. Access recirculation in jugular venous catheter in regular and reversed lines. Iran J Kidney Dis. 2008;2(2):91-4. [View at paplisher] [Google Scholar]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |






